Crosslinking
Early results of a prospective, randomized clinical trial centered in Teaneck, N.J., show no differences in simultaneous Intacs and corneal crosslinking compared to sequential treatment—Intacs and followed by crosslinking at three months for keratoconus and ectasia. Studies suggest that the beneficial effects of CXL are not achieved until six months postoperatively, which indicates early healing may be confounding results. In the trial, 31 eyes were randomized to receive Intacs followed by corneal collagen crosslinking on the same day (Sim group) (15 eyes) or Intacs followed by CXL at three months postoperatively (Seq group) (16 eyes). All eyes received symmetric 350-µm Intacs segments (Addition Technology) and CXL was performed using the UVX system (Peschke Meditrade). Clinical outcomes including UCVA, BCVA, MRSE, manifest cylinder and topographic changes (Kmax) using the Pentacam were assessed pre- and postoperatively.
Thirteen eyes in the Sim group and seven eyes in the Seq group have data collected to three months postoperatively. For Sim eyes, mean UCVA preoperatively was 20/171 and was 20/162 three months postoperatively. Mean BCVA changed from 20/44 preoperatively to 20/47.
MRSE improved by 0.94 D and manifest cylinder remained unchanged. Topographically, Kmax flattened by 0.91 D. None of the outcomes reached statistical significance. Similarly, Seq eyes, showed no significant changes in UCVA (improved from 20/175 to 20/153) and BCVA (improved from 20/36 to 20/28). MRSE improved by 0.68 D, but failed to reach statistical significance. Manifest cylinder remained unchanged as did topographically measured mean Kmax. No significant differences between Sim and Seq cohorts were observed. The optimal method and timing of Intacs combined with CXL remains to be elucidated with further follow-up, the group says.5197
A study in Athens, Greece, also looked at Intacs and CXL in 12 keratoconus cases. All cases had undergone Intacs implants six to 32 months previously and were then treated with CXL. Following PTK (50 µm, 6.5 mm diameter), the eyes underwent UVA-induced CXL after the administration of 0.1% riboflavin drops. The mean follow-up was 1.6 years (r: one to four years). The mean values were: UCVA: 0.3 preop, 0.4 postop; BSCVA: 0.4 preop, 0.5 postop; spherical equivalent: -2.25 D preop, -2.00 D postop; mean keratometry: 45.5 D preop, 44.5 D postop; total pachymetry: 445 preop, 425 postop; endothelial cell count: 2,750 preop, 2,700 postop. None of the cases developed signs of ectasia progression within the follow-up period.
The group concludes that CXL appears to be a safe and effective adjunctive treatment in preventing ectasia in eyes that had previously had Intacs implantation.5200
Long-term results provide further evidence that CXL is effective in arresting progressive post-LASIK ectasia, say surgeons in Switzerland and Italy. Twenty-five eyes with topographically documented progressive post-LASIK ectasia received standard treatment of riboflavin 0.1% following epithelial abrasion and then irradiation with UVA light. The eyes were monitored for a minimum of 36 months.
At 36 months after cross-linking, mean BSCVA had significantly (p<0.05) improved from 0.46 ±0.25 to 0.69 ±0.22 (decimal scale). Sixty-three percent of the eyes had gained more than two lines of BSCVA at the same follow-up. Also, 21 percent had achieved a BSCVA of 1.0, while only 16 percent had attained 0.6 or worse. Mean SE refraction had improved from -3.77 D to -1.96 D. Mean cylinder was lowered from -2.79 D to -2.16 D. Topography maps exhibited markedly reduced steepest points as early as four months following treatment, as well as stability of keratometry readings. Mean central corneal thickness decreased significantly (p<0.05) from 439 ±43 µm prior to cross-linking to 421 ±40 µm at 36 months. Similarly, mean thinnest point pachymetry showed a significant decrease from 431 ±45 µm to 411 ±45 µm during the follow-up period. While mean SE and mean corneal coma decreased during the three years, the differences were not statistically significant when compared with the preoperative data. The parameters used to monitor the action of cross-linking on kerectasia show results very similar to those obtained when treating progressive keratoconus, the group says.5204
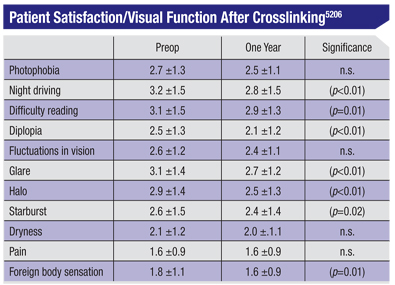
Also from New Jersey comes a report showing that at one year after crosslinking treatment, patients note subjective improvement in a number of visual symptoms. The study included 107 eyes of 76 patients who underwent CXL for keratoconus (n=71) or ectasia (n=36) in a prospective, randomized controlled trial. Patients completed a subjective questionnaire concerning their visual symptoms, administered preoperatively and at one year. Patients ranked symptoms on a scale from 1 (none) to 5 (severe). Improvements in maximum keratometry (Kmax) and BCVA were correlated with each of the subjective visual symptoms.
Preoperative to one year changes in symptoms appear in the table above.
All other changes at one year failed to reach statistical significance. There was no significant difference between the keratoconus and ectasia subgroups. There was a weak, but significant, association between the change in Kmax, and the change in night driving (r=0.3, p<0.01), pain (r=0.2, p=0.04), and foreign body sensation (r=0.3, p<0.01) ratings. There was no association between the change in BCVA and the change in any of the questionnaire ratings at one year.5206
Keratoplasty
Surgeons at the Cleveland Clinic and Case Western Reserve University describe a novel enzymatic technique that facilitates the separation of Descemet’s membrane from the stroma without affecting endothelial cells viability. This technique may be useful for deep anterior lamellar keratoplasty (DALK) and Descemet’s membrane endothelial keratoplasty (DMEK) procedures, they report.
Seven fresh human pairs of corneoscleral donors were mounted on an artificial anterior chamber with Optisol medium filling the endothelial side. Seven received an intrastromal injection of 2.5 mg/ml Collagenase type 2 in BSS followed by an injection of air into the stroma after incubation. The contralateral eye, without any enzymatic or air treatment, was used as a control.
Histological examination of the separated Descemet’s membrane and underlying endothelial cells showed a healthy appearance after collagenase incubation and when evaluated as isolated Descemet’s membrane sheets. Trypan blue evaluation of the separated Descemet’s flat mounts demonstrated a mean viability of endothelial cells following collagenase incubation of 89.7 percent (r: 82.1to 94.1 percent) compared to a mean viability of 91.2 percent (r: 87.5 to 92.7 percent) in the control group (p=0.1; not statistically significant).793
Patients who underwent Descemet’s stripping endothelial keratoplasty (DSEK) for Fuchs’ corneal dystrophy subjectively report satisfaction with their visual function, according to a Duke University study.
Patients at Duke University Eye Center who have undergone DSEK in at least one eye for Fuchs’ corneal dystrophy between 2005 and 2010 were eligible; 113 out of 250 eligible subjects (45.2 percent) consented to participate in the study. Subjects were asked to fill out the NEI’s Visual Function Questionnaire-25, which consists of 25 questions plus 14 optional questions that measure the dimensions of self-reported vision health status for people with chronic eye diseases. Score calculations were carried out according to a set VFQ-25 algorithm, with 100 being the best possible score and 0 being the worst possible score.
The average age was 72.1 years; 89.4 percent were Caucasian; 8.2 percent were African American; 2.4 percent did not record a race; 64.7 percent were female. Out of a total best possible score of 100, DSEK patients reported an overall VFQ score of 82.3. They reported a general health score of 69.9 and a general vision score of 76.4. Scores for near activities versus distance activities were similar at 78.5 versus 79.6. The score for activities related to social functioning was 92.5. Patients’ emotional well-being as affected by visual symptoms received a score of 79.2. Patients’ ability to fulfill daily roles received a score of 79.9, while their ability to function independently received a score of 88.8. Driving ability received a separate score of 72.4. Patients reported a score of 93.4 for color vision and 83.0 for peripheral vision.749
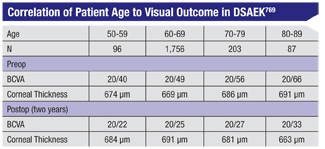
Researchers in Oregon and California stress the importance of controlling for patient age with regard to visual outcomes, following their study of patients with Fuch’s endothelial dystrophy who underwent Descemet’s stripping automated endothelial keratoplasty (DSAEK).
The retrospective review included 563 eyes of patients with visually significant Fuchs’ endothelial dystrophy with or without cataract. Eyes with other vision-limiting ocular comorbidities were excluded. All eyes received DSAEK surgery with or without cataract surgery using a single operative technique. (See Table, above.) One-way ANOVA testing was significant at all time points with respect to vision and patient age (p<0.005).
On average, patients aged 80 to 89 had BCVAs two lines worse than patients aged 50 to 59 at two years postoperatively. Both ANOVA testing and the Pearson correlation support a direct relationship between patient age and logmar BCVA at all time points, pre- and postoperatively. Possible explanations for worse visual acuities in older patients include more advanced corneal pathology, decreased capacity for blur recognition, or the presence of subclinical visually significant retinal pathology. Similar corneal thicknesses amongst all groups pre- and postop suggest that the discrepancy is not likely due to differences in corneal pathology.769
Noting that patients who suffer from Fuchs’ endothelial dystrophy have a decreased contrast sensitivity threshold and that removal of endothelial guttata by DSAEK surgery has also been demonstrated to decrease intraocular light scatter and improve contrast thresholds, investigators at Denmarks’ Aarhus University conducted a comparison of different visual qualities in patients who had undergone DSAEK surgery in one eye while having untreated Fuchs’ in the other eye.
They enrolled 32 eyes of 16 patients with bilateral Fuchs’ endothelial dystrophy who had DSAEK surgery performed in one eye. Visual acuity at 100 percent contrast and contrast sensitivity as evaluated by a modified simulation of the Freiburg Acuity and Contrast Test, FrACT, was measured in both eyes of each patient.
Snellen VA improved in treated eyes from 0.67 ±0.35 (SD) before surgery to 0.42 ±0.21 after surgery (logMAR units; p=0.038). In eyes with untreated Fuchs’ dystrophy visual acuity was 0.48 ±0.13. In a pair-wise comparison, there was no difference in Snellen visual acuity between treated and non-treated eyes (p=0.39). Contrast sensitivity was significantly better in DSAEK treated eyes compared with untreated eyes. Mean logCS in DSAEK treated eyes was 1.06 ±0.26 compared with a mean logCS of 0.85 ±0.15 in untreated eyes (p=0.016). All patients reported a subjective improvement in vision from before to after DSAEK surgery.
Despite improved contrast sensitivity in the DSAEK operated eyes, the absence of any difference in visual outcome with standard Snellen VA implies that subjective visual improvements caused mainly by an improved ability to discern contrast can be undetectable with standard Snellen BSCVA, the group suggests.758
According to a group at Devers Eye Institute, Portland, Ore., the average endothelial cell loss following DSAEK surgery in Fuchs’ endothelial dystrophy patients remains relatively stable up to two years postoperatively. There is a subsequent gradual decline in ECD after two years which is observed at least through postoperative year four. The prospective, noncomparative, interventional case series included 439 eyes undergoing DSAEK surgery for Fuchs’ endothelial dystrophy. Postoperative donor endothelial cell density was assessed at six months (n=439), 12 months (n=360), two years (n=230), three years (n=115), and four years (n=36) and compared with preoperative eye bank measurements.
The average and standard deviation percentage ECD loss at six months was: 24.9 ±16.1 percent; at 12 months 25 ±16.1 percent; at two years 25.7 ±16.6 percent; at three years 32.4 ±18.8 percent; and at four years 40.2 ±21.7 percent.768
A retrospective analysis at the University of Texas Southwestern Medical Center, Dallas, centered on factors associated with DSAEK graft dislocation. Over five years of DSAEK for patients with corneal endothelial cell dysfunction, the researchers studied the preoperative corneal donor data including preoperative storage time and endothelial cell count, as well as surgical technique employed, corneal incision size and postop graft thickness and graft size, and they collected data up to one year postop.
The dislocation rate over five years was 25 percent. The central corneal thickness during the last visit was 668.7 ±99.8 µm (p<0.0001); the mean grafts size was 8.3 ±0.5 mm; the mean preoperative endothelial cell count in the grafts was 2,533 ±190 cell/mm; and the mean preoperative storage time was 5.2 ±3 days There was no statistically significant correlation among graft dislocation and CCT, graft size, preoperative storage time and endothelial cell count, and the authors conclude that these were not associated with increased graft dislocation after DSAEK.747
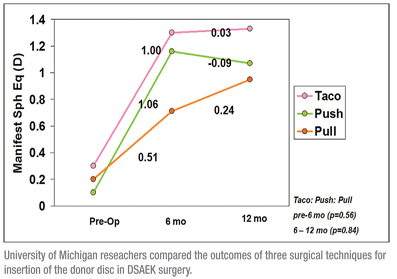 Another retrospective study, this one at the University of Michigan, compared the outcomes of three surgical techniques for insertion of donor discs in patients undergoing DSAEK between 2007 and 2009. Surgical techniques of four surgeons were reviewed; they included forcep-assisted pulling and needle-assisted pushing of the donor lenticule, and forcep-assisted insertion of a 60-40 folded donor lenticule (taco). Preoperative clinical characteristics, surgical technique, postoperative complications, visual acuity, manifest spherical equivalent and cylindrical correction were recorded. One-hundred eyes of 100 patients underwent DSAEK with 51 receiving the taco, 19 the push technique and 30 eyes receiving the pull techniques. There were no differences in BCVA at six months and one year postoperatively (p>0.25). The BCVA improved significantly in the first six months postop in all three groups with no significant change from six months to one year postop. A statistically significant hyperopic shift of 0.86 D was observed, with no difference in the shift across the three groups (p>0.5). There was no significant astigmatic change at any time point (p>0.3). A comparison of postop complication rates revealed a similar donor dislocation rate of 19 percent among all three techniques (p=0.61) (See Figure, above). All three techniques were deemed equally effective at all postop time points with similar VA outcomes. The techniques result in a similar hyperopic shift and are astigmatically neutral. Additionally, dislocation rates are similar amongst the three techniques.744
Another retrospective study, this one at the University of Michigan, compared the outcomes of three surgical techniques for insertion of donor discs in patients undergoing DSAEK between 2007 and 2009. Surgical techniques of four surgeons were reviewed; they included forcep-assisted pulling and needle-assisted pushing of the donor lenticule, and forcep-assisted insertion of a 60-40 folded donor lenticule (taco). Preoperative clinical characteristics, surgical technique, postoperative complications, visual acuity, manifest spherical equivalent and cylindrical correction were recorded. One-hundred eyes of 100 patients underwent DSAEK with 51 receiving the taco, 19 the push technique and 30 eyes receiving the pull techniques. There were no differences in BCVA at six months and one year postoperatively (p>0.25). The BCVA improved significantly in the first six months postop in all three groups with no significant change from six months to one year postop. A statistically significant hyperopic shift of 0.86 D was observed, with no difference in the shift across the three groups (p>0.5). There was no significant astigmatic change at any time point (p>0.3). A comparison of postop complication rates revealed a similar donor dislocation rate of 19 percent among all three techniques (p=0.61) (See Figure, above). All three techniques were deemed equally effective at all postop time points with similar VA outcomes. The techniques result in a similar hyperopic shift and are astigmatically neutral. Additionally, dislocation rates are similar amongst the three techniques.744
A study based in Los Angeles finds that femtosecond-enabled keratoplasty, or FLEK, offers faster visual recovery and better long-term outcomes in keratoconus patients compared to those that had the mechanical penetrating keratoplasty. The retrospective comparative surgical case series included 126 keratoconus patients (137 eyes); 56 patients (66 eyes) underwent FLEK, and 60 patients (71 eyes) had traditional blade trephination PKP. Follow-up ranged from three to 12 months.
Best-spectacle corrected VA was significantly better as early as three months (p=0.001), and even at 12 months of follow-up (p=0.007) in the FLEK group. Visual recovery to driver’s-license vision after three months was significantly better in the FLEK group (p<0.001). Topographic astigmatism was better in the FLEK group, but the difference between the two groups reached significance only at three months (p=0.001). Postoperative complications noted were not different between the groups. At 12 months, after all sutures had been removed in both groups, the topographic astigmatism in the FLEK was less but not statistically significantly different from the mechanical PKP group.3375
Dry Eye, Tears
Of interest to users of the TearLab osmometer, a study at the University of Applied Sciences, Olten, Switzerland, confirms that film osmolarity values vary significantly, depending on where precisely within the tear meniscus the tear film sample is collected. Hyperosmolarity of the tear film is recognized as a key feature of dry-eye syndrome and considered to be its single most accurate objective diagnostic test. With application of the TearLab, nanoliter volumes of tear fluid can now be measured with the same analytical performance as laboratory osmometers.
To determine the dependence of the chip position in a liquid meniscus during sample collection, three different angle positions (70°, 90° and 120°) of the Tearlab chip towards to the horizontal glass slide were analyzed. For each angle, 10 measurements were carried out. To evaluate repeatability, tear osmolarity measurements were carried out independently in 13 healthy subjects by two different examiners.
Osmolarity values varied significantly by 8.9 mosm/l with different angle positions of the TearLab chip (p<0.001). At 90°, osmolarity was 314.4 ±7.0 mosm/l compared to 323.3 ±5.4 mosm/l at 120°. Inter- and intra-examiner variability were found to be considerable.The differences found depending on where precisely within the tear meniscus the tear film sample was collected may, in part, account for the considerable inter- and intra-examiner variability found in this study. For accurate and reliable osmolarity measurement, this technical challenge during the tear sample collection should be addressed, the authors write.3797
Another study at two U.S. and two Chinese universities assessed the variation of tear osmolarity and its relation to tear meniscus volume in dry-eye patients and healthy controls.
In this pilot study, 10 clinically diagnosed dry-eye patients (four males and six females, age 36 ±12 yrs.) and 10 normal subjects (five males and five females, age 27 ±7 yrs.) were enrolled. The tear meniscus volume was measured with ultra-high resolution optical coherence tomography and tear osmolarity was measured using the TearLab Osmolarity system. Both measurements were conducted every two hours from 8:30 a.m. to 4:30 p.m. Diagnosis of dry eye was based on signs and symptoms (OSDI >12 and TBUT <10 seconds or Schirmer <5 mm).
At screening, the OSDI score was 37 ±20) in the dry-eye group, which was significantly higher than that in the healthy group (3 ±3, p<0.01). The average osmolarity was 299.8 mOsms/L ±11.5 for dry-eye patients and 296.6 ±13.3 for normals. Over the course of eight hours, the osmolarity score of a single individual varied from 6 to 43 in the dry eye group (mean variation 18.6, ±12.8 and from 8 to 35 in normals (mean variation 20.2, ±8.7). Differences in total tear volume as measured by OCT were found between two groups at the last three time points (p<0.05). No correlations were found between tear meniscus volumes and tear osmolarity in any of these two groups (r was 0.03 for dry eye group and -0.005 for healthy group, p>0.05).
Based on the TearLab recommended cut-off for determining dry eye (308), the tear osmometer may under-diagnose dry eye, the authors say.3795
An interesting finding regarding dry-eye diagnosis results from work at Ora Inc., Andover, Mass. The researchers note that the blinking lid is the driving phenomenon governing the maintenance of the tear film and that the action of a “squeeze blink,” a direct, conscious blink in which the eyelids exert pressure on each other, has been shown to increase the thickness of the tear film. They hypothesized that a squeeze blink could result in expression of meibomian glands and greater stability of the tear film.
In a sample population of eight dry-eye subjects selected by symptomatology and fluorescein corneal staining, the subject was asked to perform a squeeze blink and the tear film was examined using fluorescein videography. The subject’s tear film was examined for one minute pre- and post-squeeze blink.
A reduced tear-film breakup time was observed immediately after the squeeze blink. In all cases, the squeeze blink was followed by three to five full blinks with low inter-blink intervals. Mean TFBUT decreased from 7.1 seconds in the minute prior to squeeze blink to 1.02 seconds post-squeeze blink (p=0.010). This acute response was followed by a return to mean TFBUT of 6.99 seconds (p=0.040).
The reduction in tear-film breakup time appears to be largely the result of local variations in the tear-film distribution, they say. Recovery and improvement of a uniform and stable tear film occurred several blinks after the squeeze blink, suggesting that over expression of the meibomian glands may have adverse immediate effects on tear-film stability and no lasting benefits. The results show the need for caution when comparing natural blink to directed blink activity in a diagnostic setting.3725
Another study, a collaboration between French and U.S. researchers, highlights one of the inherent challenges in randomized, clinical trials for dry-eye drugs: Although a poor concordance between dry-eye signs and symptoms has been recognized in the literature, improvement in both signs and symptoms is an expected outcome in such trials investigating new dry-eye treatments.
The research was based on a six-month, Phase III, multicenter, randomized, controlled, double-masked trial of NOVA22007 (cyclosporine 0.1% ophthalmic cationic emulsion, Novagali Pharma) administered once daily versus its emulsion vehicle in 492 patients with moderate to severe dry eye (grade 2 to 4 corneal fluorescein staining, CFS, on the modified Oxford scale). The primary objective of the study was to demonstrate superiority of NOVA22007 on both a dry-eye sign (mean change in CFS) and dry-eye symptoms (mean change in global score of ocular discomfort using a visual analog scale, VAS). (Each if the investigators reports a commercial relationship with Novagali Pharma.)
Statistically significant improvements in CFS were observed at one, three and six months in treated patients. Despite noticeable improvements in the mean VAS score from baseline, no statistically significant difference was observed compared to the vehicle at six months. Analysis revealed considerable variability in VAS score across the range of CFS scores, highlighting the poor correlation between DED signs and symptoms. At month six, 56 percent of patients showed improvement in both CFS and VAS scores.
Paradoxically, 15 percent of patients showed worsening on the VAS despite improvement in the CFS score and 18 percent showed improved VAS scores in the presence of no change or worsening of the CFS score. This discordance between dry-eye signs and symptoms in patients with moderate to severe dry-eye disease underscores the regulatory challenge of simultaneously achieving statistically significant outcomes for both dry-eye signs and symptoms in randomized, controlled clinical trials evaluating pharmacologic therapies, the authors say.3821
Pharmaceuticals
Paradoxically, 15 percent of patients showed worsening on the VAS despite improvement in the CFS score and 18 percent showed improved VAS scores in the presence of no change or worsening of the CFS score. This discordance between dry-eye signs and symptoms in patients with moderate to severe dry-eye disease underscores the regulatory challenge of simultaneously achieving statistically significant outcomes for both dry-eye signs and symptoms in randomized, controlled clinical trials evaluating pharmacologic therapies, the authors say.3821
Pharmaceuticals
Short-term topical bevacizumab therapy effectively reduces the severity of corneal neovascularization without local or systemic adverse effects, according to a collaboration between Boston and Washington, D.C. researchers.
Twenty eyes of 20 patients with stable corneal NV were treated in a prospective, open-label, noncomparative study, with 1% topical bevacizumab for three weeks, and followed up for 24 weeks. The main efficacy outcomes measured were neovascular area (NA), the area of the corneal vessels themselves; vessel caliber (VC), the mean diameter of the corneal vessels; and invasion area (IA), the fraction of vessel incursion in the cornea.
Compared to the baseline visit, the NA showed statistically significant improvement at week six (mean=27.9 percent, p=0.007), which was three weeks after stopping the medication, and the VC at week 12 (mean=30.8 percent, p=0.006), which was nine weeks after the treatment of study drug. By week 24, the mean reductions were 47.5 percent (SD, 37.5 percent) for NA, 36.2 percent (SD, 44.1 percent) for VC, and 20 percent (SD, 42 percent) for IA. The decreases in NA and VC were statistically significant (p<0.001 and p=0.003, respectively), but IA was not (p=0.06). No significant change was noted in visual acuity or central corneal thickness. Topical bevacizumab was well-tolerated with no adverse events.
The authors point out that statistically significant reductions in NV parameters are evident well after termination of therapy. Although the efficacy is delayed, it remains stable at least beyond early time points.6399
Another group at two centers in London, England, conducted what they call the first randomized, placebo-controlled trial to evaluate the effectiveness of subconjunctival bevacizumab in eyes with a recent onset of corneal NV.
Thirty patients with progressive corneal NV present for less than six months resulting from various underlying conditions received subconjunctival injection of bevacizumab 2.5 mg in 0.1 ml every four weeks for a total of three injections. The placebo arm (15 patients) received one subconjunctival injection of 0.1 ml normal saline on the same schedule. All patients received their allocated treatment with no losses to follow-up.
Corneal new vessel area reduced 36 percent (r: +40 to -92 percent) in those patients receiving bevacizumab versus an increase of 90 percent (r: +1,394 to -58 percent) for those allocated placebo (p=0.007). There were three adverse events, two epithelial defects (one patient in each arm) and one severe corneal graft rejection with extensive (+1,384 percent) neovascularisation (placebo arm). Excluding this patient, the placebo group had a mean reduction in new vessels of 3 percent, but still a significant difference from the treatment arm (p=0.036).
Conjunctival injection site vessel size reduced from baseline to three months in both arms (bevacizumab -2.2 percent, placebo -0.8 percent) and the groups were similar with regards to changes in BCVA, central corneal thickness, IOP and endothelial cell counts. Further studies are needed to confirm this effect and optimum treatment regime, the group suggests.6410
Subconjunctival bevacizumab treatment was also assessed in a retrospective, non-comparative study in New York. The chart review included 19 eyes from 19 patients with corneal NV who had been treated with subconjunctival bevacizumab 1.25mg/0.05ml and followed up at one, two, three and six months. All neovascularization parameters, neovascular area, vessel caliber and invasion area, demonstrated improvement in 66 percent of the eyes treated with subconjunctival bevacizumab. Twenty-nine percent of eyes demonstrated no change in NV parameters while 5 percent of eyes progressed despite treatment. No local or systemic side effects were observed.6384
A case report from the University of Florida suggests another potential use for the drug: intracameral bevacizu mab in treating deep corneal NVsecondary to graft failure.
A 41-year-old male presented with corneal graft failure demonstrating deep stromal NV and central corneal opacity. He had a history of keratoconus for which he had undergone three prior penetrating keratoplasties in the affected eye. His BCVA was 20/400. The pupil could not be visualized. Clinical improvement did not occur despite therapy with 40 mg oral prednisone, hourly prednisolone acetate 1% eye drops, and a subconjunctival injection of bevacizumab (1.25mg). Subsequently, he was given two intracameral injections of bevacizumab (1.25 mg) spaced four weeks apart. Topical prednisolone acetate was continued. Slit-lamp photography and aqueous samples were obtained prior to and following intracameral injections. Aqueous samples were analyzed to detect concentration of vascular endothelial growth factor.
There was marked reduction in the corneal stromal NV and central opacification following two intracameral injections. The resultant clarity allowed the pupil and iris to be visualized and the patient’s vision improved to 20/200. Pre-injection VEGF level was 7.912 pg/mL, which increased to 9.308 pg/mL prior to the second injection. Clinical improvement in the case was not related to aqueous concentrations of VEGF which remained normal despite anti-VEGF therapy, the authors, say, suggesting an alternative mechanism of action.2006
Miscellaneous
Subconjunctival bevacizumab treatment was also assessed in a retrospective, non-comparative study in New York. The chart review included 19 eyes from 19 patients with corneal NV who had been treated with subconjunctival bevacizumab 1.25mg/0.05ml and followed up at one, two, three and six months. All neovascularization parameters, neovascular area, vessel caliber and invasion area, demonstrated improvement in 66 percent of the eyes treated with subconjunctival bevacizumab. Twenty-nine percent of eyes demonstrated no change in NV parameters while 5 percent of eyes progressed despite treatment. No local or systemic side effects were observed.6384
A case report from the University of Florida suggests another potential use for the drug: intracameral bevacizu mab in treating deep corneal NVsecondary to graft failure.
A 41-year-old male presented with corneal graft failure demonstrating deep stromal NV and central corneal opacity. He had a history of keratoconus for which he had undergone three prior penetrating keratoplasties in the affected eye. His BCVA was 20/400. The pupil could not be visualized. Clinical improvement did not occur despite therapy with 40 mg oral prednisone, hourly prednisolone acetate 1% eye drops, and a subconjunctival injection of bevacizumab (1.25mg). Subsequently, he was given two intracameral injections of bevacizumab (1.25 mg) spaced four weeks apart. Topical prednisolone acetate was continued. Slit-lamp photography and aqueous samples were obtained prior to and following intracameral injections. Aqueous samples were analyzed to detect concentration of vascular endothelial growth factor.
There was marked reduction in the corneal stromal NV and central opacification following two intracameral injections. The resultant clarity allowed the pupil and iris to be visualized and the patient’s vision improved to 20/200. Pre-injection VEGF level was 7.912 pg/mL, which increased to 9.308 pg/mL prior to the second injection. Clinical improvement in the case was not related to aqueous concentrations of VEGF which remained normal despite anti-VEGF therapy, the authors, say, suggesting an alternative mechanism of action.2006
Miscellaneous
The deep conjunctival fornices can be a site for prolonged sequestration of bacteria, causing recurrent infections. A group at Wills Eye Institute, Philadelphia, reports a series of five cases of giant fornix syndrome, a rare cause of chronic purulent conjunctivitis in the elderly. Removing the infected debris from the superior fornix and reconstruction of the upper eyelid may prevent the chronic persistent infection, they report.
The median age of the five female patients was 75 years (mean 80, r: 70 to 95). The median duration of eye symptoms before presentation was two years (mean 2.4, r: 1 to 4). Prior to referral, the chronic conjunctivitis was treated with topical antibiotics in all five cases and with additional dacryocystorhinostomy in one case. Floppy eyelids were present in two cases. The superior fornix was involved in four cases and the inferior fornix in one. Pseudomembranes and superficial punctate keratitis were seen in three cases. Diagnosis of giant fornix syndrome was made in all five cases. Conjunctival culture grew methicillin-resistant Staphylococcus aureus, Pseudomonas aerugenosa and Staphylococcus aureus in singular cases. Case 1 was treated with topical moxifloxacin; case 2 with topical vancomycin and repair of the upper eyelid; case 3 with topical besifloxacin; and case 4 with DCR and topical vancomycin. Case 5 was treated with reconstruction of the left upper eyelid. The median duration of follow-up was four months (mean 21.6, r: one to 84).1963
Investigators at several U.S. sites collected Internet responses from a November 2010 survey of members of the Cornea Society to assess treatment practices and opinions for treating recurrences of herpes zoster ophthalmicus. The survey presented the clinical scenario of a patient with signs of recurrent HZO (stromal keratitis and anterior uveitis). Respondents were highly divided over the efficacy of prolonged antiviral therapy to reduce chronic or recurrent disease. Most ophthalmologists are not recommending the zoster vaccine to patients with a history of HZO; however, respondents were uncertain whether or not the vaccine could reduce recurrences.
Of the 75 respondents, 85 percent were cornea specialists. In the recurrent HZO clinical scenario, the majority of respondents chose to treat with a combination of oral antiviral and topical steroid (67 percent). The most common choice of steroid and dose was prednisolone acetate 1% q.i.d. (51 percent). Among respondents who chose to treat with oral antivirals, 39 percent chose to treat for seven to 14 days, 16 percent for one year or longer, 16 percent for as long as steroids were being administered, and 15 percent some other duration. Fifty-six percent of respondents believed that prolonged acyclovir prophylaxis could prevent or reduce recurrent signs of HZO during the period of administration; 32 percent believed recurrences would be reduced after the period of administration. The majority of respondents said they are not recommending the zoster vaccine to patients with a history of HZO (66 percent), but 49 percent of respondents believed the vaccine could reduce recurrent signs or did not know. The majority (86 percent) of physicians reported treating recurrent or chronic cases of HZO in the last year.
The results of this survey demonstrate the need for further systematic study of treatment and prophylaxis for recurrent and chronic HZO, the authors conclude.1503
Research in Sweden may represent the first study to compare Bowman’s layer thickness in vivo and ex vivo in the same tissue samples. The group at Linkoping University says the work is important because there is very little data on Bowman’s layer thickness in vivo, and laser surgery done today is based on assumed Bowman’s layer thickness values. Additionally, correlation of Bowman’s layer morphology in vivo with light microscopy sections could help to identify signs of pathology in patients in the future by in vivo observation alone. They conclude that the thickness of BL depended on the method used, with the in vivo measurements generally yielding a larger value.
The study examined 17 consecutive corneal transplant patients preoperatively by in vivo confocal microscopy; 13 of 17 corneas were suitable for in vivo and ex vivo comparison. Seven of 13 of the prepared corneas had a uniformly thick BL in light microscopy and were selected for in vivo/ex vivo thickness comparison. BL thickness was measured between 4 to 12 times per cornea at various central locations by light microscopy. Five to seven IVCM scans through BL from each cornea were selected, from which BL thickness was measured by two observers. They compared the thickness of BL by the two methods. The remaining six of 13 corneas showed abnormal morphology in BL by light microscopy and were further characterized and compared with the IVCM images.
The mean BL thickness in a given central cornea ranged from 7.8 to 12.8 µm by light microscopy and from 10.4 to 14.2 µm by IVCM. BL thickness in vivo was significantly greater than in tissue sections (p<0.017). In the same cornea, in vivo BL thickness was significantly greater than ex vivo values in five of seven cases (p<0.016). No significant correlation, however, between in vivo and ex vivo thickness could be found in this small series. Of the six corneas with abnormal BL morphology, four had stromal cells, stromal tissue or scar tissue anterior to BL, three had focal absences, thinning or folding of BL, and one had an abnormal-appearing basement membrane by light microscopy. Interestingly, these morphologic findings were also observed in vivo, in an en face orientation.305
Dr. Afshari is an associate professor of ophthalmology at the Duke University Eye Center. She receives funding from Research to Prevent Blindness as well as the National Eye Institute.




