The Extent of the Problem
Ocular and periocular injuries can cause significant morbidity. The United States Eye Injury Registry has reported that periocular injuries occur in 5 percent of all serious injuries, with the majority involving the canaliculi (81 percent) and/or eyelids (70 percent). Not surprisingly, many of these injuries occur in children (23 percent) and teens (18 percent). Nearly half of periocular or ocular injuries (40 percent) occur in the home, most commonly from a blunt object (31 percent), and more than half (60 percent) of those with eyelid involvement have an underlying globe injury. A study performed by the National Center for Health Statistics estimated that more than 2 million eye injuries occur annually in the United States and about 90 percent of them are considered preventable.
Canalicular injuries result from penetrating injury or blunt trauma 54.2 percent and 45.7 percent of the time, respectively. Cadaver studies have showed that when a force is applied to the lateral canthus or malar eminence (as commonly occurs with a fist), lacerations will occur in the medial canthus because the medial canthal complex is weakened as it splays around the lacrimal drainage system. Such medial canthal injuries are frequently associated with laceration of the lacrimal drainage system (upper/lower canaliculus, common canaliculus, lacrimal sac). Of note, these lacerations often hide within the normal and complex three-dimensional anatomy of this area, and aren’t suspected by the clinician because the blunt trauma occurred more laterally.
You should also maintain a high suspicion of canalicular involvement in lacerations medial to the puncta and secondary to dog-bite injuries. Canalicular laceration mandates primary repair. If not clearly evident, perform probing and irrigation of the lacrimal system to definitively confirm or rule out a canalicular laceration. (See Figure 1) A visible probe within the soft tissue laceration confirms the presence of canalicular injury. If probing can’t be performed because of poor cooperation, then exploration in the operating room under anesthesia is indicated. A detailed anatomic description of the periocular structures is beyond the scope of this paper. However, a brief overview of the lacrimal drainage anatomy for quick reference is provided in Figure 2 on pg. 52.
Initial Assessment
The following steps are crucial for obtaining the correct diagnosis:
• Evaluation and history. Eyelid injuries frequently occur in the context of serious systemic or neurologic trauma. Severe head or facial injury often camouflages or supercedes occult ocular injuries, leading to a delay in diagnosis and therapy. A complete ocular examination is recommended in all patients with facial or head injuries once the patient is otherwise stable.
Begin the evaluation with a complete history that includes pointed questions about the injury, including its mechanism, timing and location.
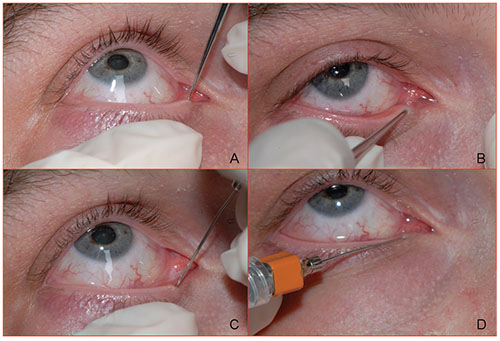 |
| Figure 1. Probing and irrigation. After application of topical anesthesia, the clinician inserts a pediatric punctum dilator into the punctum vertically with a gentle rotating motion while applying lateral traction to the lower eyelid (A). The clinician turns the dilator horizontally and gently advances it, further dilating the punctum and proximal canaliculus. The dilator is then removed (B). Next, either a #00 Bowman probe or, as shown here, a straight lacrimal cannula attached to a syringe, is passed into the canaliculus, first vertically and then horizontally. Once again, it’s critical to maintain lateral traction on the lid to prevent bunching of soft tissue. The examiner advances the cannula along the length of the horizontal canaliculus until bone (a hard stop) is felt (C). The cannula is pulled back slightly and irrigation is performed to confirm that nasolacrimal drainage is intact. If at any point the physician identifies the tip of the probe or cannula, a canalicular laceration is present (D). |
Suppress the urge to begin the ocular examination with obvious clinical findings such as a lid laceration; instead perform a complete ophthalmic examination. During the ocular adnexal exam, avoid placing any pressure on the underlying globe until you’ve definitively ruled out globe injury. Note all the details about the lacerations, including the location, depth and any fat protrusion through the eyelid (which is an indication of orbital penetration). Any injuries to the medial canthus, even if trivial in appearance, raise the likelihood of canalicular involvement and necessitate probing and irrigation of the lacrimal drainage apparatus. This is especially common following periocular dog bites, which almost invariably lacerate one or more canaliculi.
To begin the probing procedure, administer topical ocular anesthetic (proparacaine, tetracaine or viscous lidocaine). Despite this maneuver, many patients will still experience discomfort during P&I, so you should warn them of this possibility. You then dilate the punctum with a pediatric punctum dilator and begin probing with a #00 Bowman probe or straight lacrimal cannula. Pass the probe vertically for 2 to 4 mm, and then rotate it horizontally toward the nose. Gentle lateral traction on the eyelid facilitates advancement of the probe.
• Imaging. Isolated eyelid lacerations with an otherwise normal ophthalmologic exam don’t necessitate imaging, with several caveats. If you suspect a penetrating foreign body, perform computed tomography; avoid plain films, since they simply expose the patient to radiation without offering any detail as to the specific anatomic location of the foreign body. If you suspect a wooden foreign body, alert the radiologist to use the correct CT window setting, since wood is notoriously difficult to image. Magnetic resonance imaging may sometimes be helpful as adjunctive imaging in this situation, but should not be used as the primary imaging modality in trauma. A poor history also lowers the threshold for orbital imaging; this is especially important when evaluating children, who may be hesitant to admit to the true mechanism of injury with their parents listening nearby. Weigh the use of CT in children to exclude the possibility of occult foreign body against the risks of serial radiation exposure in the pediatric age group. If CT is indicated, match the protocol to the patient’s age. Finally, it’s important to remember that neither CT nor MRI are very sensitive for ruling out globe rupture (especially if no globe deformity is noted) and in no way supplant examination by indirect ophthalmoscopy or surgical exploration.
Surgical Intervention
If your exam and P&I reveal damage that requires surgery, here are the main points to keep in mind:
• Anesthesia. Canalicular injuries, frequently from assaults and dog bites, are generally isolated to the inferior canaliculus. Although there is controversy as to the relative importance of the lower versus upper canaliculus, be sure to repair any canalicular injury unless the patient decides otherwise. The timing of the canalicular repair is no longer guided by the historic recommendation of six hours; successful repair five to seven days after injury is certainly achievable, but repair should proceed in a timely manner. We recommend repair within 48 to 72 hours.
Although canalicular lacerations very proximal
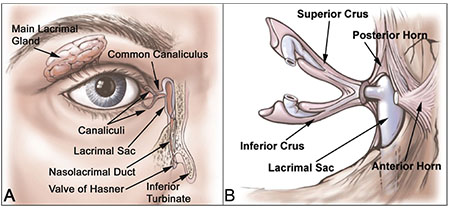 |
| Figure 2. Lacrimal drainage anatomy: The complete lacrimal drainage system is shown, along with the main lacrimal gland. Note that the nasolacrimal duct opens at the valve of Hasner in the inferior meatus, under the inferior turbinate near the floor of the nasopharynx. The middle turbinate (not shown) is located just medial to the lacrimal sac and is encountered frequently during dacryocystorhinostomy, but plays no role in canalicular laceration repair (A). Medial canthal anatomy: Note how the anterior and posterior horns of the medial canthal tendon splay around the lacrimal sac to fuse with the periosteum of the anterior and posterior lacrimal crests, respectively. The main reparative vector of the medial canthal tendon should be aimed toward the posterior lacrimal crest to prevent medial ectropion (B). |
In addition to the anesthesia induction, nasal packing around the inferior turbinate at the start of the case with three oxymetazoline-soaked ½” x 3” neurosurgical cottonoids (“neuro patties”) will shrink the nasal mucosa and facilitate retrieval of the silicone tube stents.
• Surgical repair. Begin repair of canalicular lacerations with copious irrigation and removal of particulates. If systemic antibiotics are indicated, such as for contaminated wounds, the maximum benefit is seen with administration within three hours of the original trauma. Generally, cephalexin is used, although penicillin V should be considered when an animal bite is known or suspected. Perform the standard prep with antiseptic solution; the use of povidone iodine solution is preferable to other preparations, since it is minimally toxic to the ocular surface.
Before you perform any debridement, explore the wounds and determine the proper positioning of tissue. Frequently, what appears to be significant tissue avulsion and loss is simply due to tissue retraction and edema. Because of the high tissue vascularity, it’s uncommon to have to significantly debride the eyelids; however, any frankly necrotic tissue should be removed.
Exploration of an injured canaliculus is often frustrating, especially when the injury occurs deep within the medial canthal complex close to the lacrimal sac. (See Figure 3A) During exploration, many of the canthal tendon fibers convincingly mimic the cut edge of the canalicular mucosa. Several surgical maneuvers increase the likelihood of finding the distal canaliculus and minimize the risk of creating false passages that cause further injury to the soft tissue. First, the surgeon should avoid using an excess amount of local anesthetic infiltration. This is one reason why the authors have a low threshold for canalicular repair under general anesthesia, in which case no local anesthetic infiltration is used. Second, use cotton-tipped applicators for any exploration of the deeper soft tissue injury. The use of rake retractors and toothed forceps should be limited to skin retraction alone. The use of forceps during deeper soft tissue exploration results in further splaying and distortion of the medial canthal complex. Finally, the surgeon must resist the temptation to pass a Bowman probe in an impatient and haphazard fashion into soft tissue that looks like it might be the canaliculus. A gentle, blunt exploration, although more time consuming initially, will increase the likelihood of successful identification of the distal canaliculus.
Once you’ve identified the distal canaliculus, pass a #00 Bowman probe medially into the canaliculus and lacrimal sac. Successful passage will result in a hard stop as the probe reaches the bony lacrimal sac fossa abutting the medial wall of the sac. A soft stop typically indicates that you’ve made a false passage. If you create a false passage, remove the Bowman probe and perform additional exploration. If, instead, you achieve a successful hard stop, rotate the Bowman probe about 90 degrees along the superior orbital rim while maintaining gentle medial pressure against the lacrimal sac. As the probe rotates over the superior orbital rim, gently push it against the rim with the index finger of your other hand. Apply gentle pressure inferiorly with the probe as it passes the 45-degree mark, feeling for the nasolacrimal duct with the probe’s tip. The nasolacrimal duct is usually accessible to the Bowman probe somewhere between the 45- and 90-degree rotation of the probe. While you’re doing this, be sure to avoid applying vigorous force to avoid false passage into the nose. Once the probe enters the nasolacrimal duct, advance it gently just until it hits the floor of the nasopharynx. Additional pressure will simply force the probe more posteriorly in the nasopharynx.
At this juncture, remove any nasal packing. Pass a second, larger Bowman probe through the ispilateral naris beneath the inferior turbinate into the inferior meatus. This can either be done using direct visualization with a nasal speculum or endoscope, or alternatively, simply by feel—the authors’ preferred method. It’s important to remember that the nasolacrimal duct exit in the inferior meatus is located low and lateral within the nasal cavity. A tendency to look for the tip of the probe too superiorly and medially is common and should be avoided. A metal-on-metal scraping of one probe against the other indicates successful passage into the nasolacrimal duct.
Pass one end of the bicanalicular tube through the punctum of the involved eyelid and pull it out through the proximal cut end of the canaliculus. (See Figure 2B) While appropriate soft tissue retraction is performed by the assistant, gently back the Bowman probe out of the distal canaliculus and replace it with the stented tube, which you then pass into the lacrimal sac and down the nasolacrimal duct as just described. Then, externalize the stent and tube from beneath the inferior meatus and naris using any of a variety of methods,
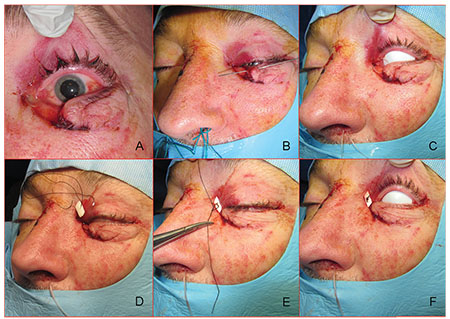 |
| Figure 3. Surgical repair: Avulsion of the medial canthal tendon with an associated canalicular laceration from a dog bite (A). Passage of a Bowman probe confirms canalicular involvement. Once the distal segment of the canaliculus is identified, the physician passes the Crawford stent through the proximal canaliculus and then into the distal canaliculus and lacrimal sac (B). The entire lacrimal drainage system has been successfully intubated and both tubes have been externalized from the left naris (C). Repair of the medial canthus: A double-armed 4-0 silk suture on large needles has been passed through the pericanalicular orbicularis oculi muscle and externalized (D). The physician ties the suture over a foam bolster made from the suture packing material (E). Final appearance (F): The medial canthal suture is removed in seven to 10 days. |
With the canalicular system identified and intubated, further soft tissue repair ensues. (See Figure 2C) Some surgeons will proceed with a meticulous—and admittedly frustrating—reapproximation of the canalicular mucosa with a fine suture, despite little evidence in the literature that this improves outcomes. We follow the recommendation of Robert Kersten, MD and Dwight Kulwin, MD, who advocate repair of the pericanalicular orbicularis oculi muscle, anticipating that the stented canalicular mucosa will heal adequately once reapproximated. One common technique we use to correctly reproduce the vectors of the medial canthal tendon (medial and posterior) is to pass a double-armed suture with large cutting needles around the pericanalicular orbicularis proximally, then distally, and continue the suture arc to skive along the periosteum medially, exteriorizing the sutures through the lateral nasal skin. (See Figures 3D and E) We then tie the sutures over a bolster and remove them a week later. (See Figure 3F) This avoids the need to tie a deep knot within the soft tissue of the medial canthal tendon. Typically, eyelid margin sutures are unnecessary. The scleral shell, which was placed over the eye at the start of the procedure, is removed before tying the tube to prevent tube migration. The final step is to place a hemostat at the level of the naris with gentle tension on the tube, cut off the stents, and tie the tube with one square knot, essentially forming a loop. The surgeon gently releases the hemostat and the tube retracts into the nasal cavity.
Complications
The overall success of canalicular repair is generally reported to be about 90 percent or higher. However, patients with canalicular lacerations can have epiphora even with careful repair. Epiphora after repair is likely more common with stent loss, stent extrusion, eyelid malposition or if no stent was placed; these issues can be avoided by individualizing the correct venue for repair (minor procedure room vs. operating room), choosing the correct anesthesia (field block vs. general anesthesia), and staffing by a surgeon experienced in canalicular laceration repair. Early, appropriate diagnosis and treatment can avoid or minimize many complications from canalicular injuries.
Other complications can also occur due to the initial injury and the wound- healing process. The relatively thin and complicated anatomy, coupled with the highly dynamic function of the eyelids, can lead to unique complications including eyelid malposition, eyelid margin notching, infection, scarring and lagophthalmos.
Eyelid injuries require a detailed examination of the globe and ocular adnexa prior to canalicular laceration repair. When performing lid laceration repair, your first priority should be to provide adequate protection for the ocular surfaces. When indicated, perform exploration of the adnexa, especially the lacrimal drainage system and the levator aponeurosis. Be sure to repair all canalicular lacerations whenever possible to minimize the risk of epiphora and other suboptimal outcomes.
Dr. Murchison is the director of the Emergency Department, and Dr. Bilyk is an attending surgeon on the Oculoplastic and Orbital Surgery Service, at Wills Eye Hospital. They also provide care at Wills’ Skull Base Division of the Neuro-Ophthalmology Service.
References
1. Dortzbach RK, Angrist RA. Silicone intubation for lacerated lacrimal canaliculi. Ophthalmic Surg 1985;16:10:639-42.
2. Hawes MJ, Segrest DR. Effectiveness of bicanalicular silicone intubation in the repair of canalicular lacerations. Ophthal Plast Reconstr Surg 1985;1:3:185-90.
3. Jordan DR, Ziai S, Gilberg SM, Mawn LA. Pathogenesis of canalicular lacerations. Ophthal Plast Reconstr Surg 2008;24:5:394-8.
4. Kersten RC, Kulwin DR. “One-stitch” canalicular repair. A simplified approach for repair of canalicular laceration. Ophthalmology 1996;103:5:785-9.
5. Linberg JV, Moore CA. Symptoms of canalicular obstruction. Ophthalmology 1988;95:8:1077-9.
6. Long JA, Tann TM. Eyelid and lacrimal trauma. In: Kuhn F and Pieramici DJ, eds. Ocular Trauma. New York, N.Y.: Thieme, 2002: 373-382.
7. Murchison AP, Bilyk JR. Canalicular repair: An analysis of variables affecting success. Ophthal Plast Reconstr Surg 2014;30:5:410-4.
8. Reifler DM. Management of canalicular laceration. Surv Ophthalmol 1991;36:2:113-32.
9. Savar A, Kirszrot J, Rubin PA. Canalicular involvement in dog bite related eyelid lacerations. Ophthal Plast Reconstr Surg 2008;24:4:296-8.
10. U.S. National Center for Health Statistics’ Health Interview Survey data. Centers for Disease Control and Prevention website: http://www.cdc.gov/nchs. Accessed 29 March 2010.
11. United States Eye Injury Registry. www.useironline.org Accessed 29 March 2010.
12. Wulc AE, Arterberry JF. The pathogenesis of canalicular laceration. Ophthalmology 1991;98:8:1243-9.
13. Murchison AP, Matthews A, Bilyk JR. Specific issues in pediatric periocular trauma. In: Black EH, Nesi FA, Gladstone, G, Levine MR, Calvano CJ, eds. Smith’s Ophthalmic Plastic Surgery, 3rd ed. New York, NY: Springer, 2011.



