When you’re faced with a patient with a history of keratoconus and multiple failed surgical procedures, it can be easy to get discouraged when thinking of all the possible pitfalls and difficulties. One’s inclination might be to advise the patient that nothing more can be done. I’m here to tell you that, with the right attitude and approach, you can help even the most difficult patient. In this article, I’ll discuss how I approach difficult cases, personalities and situations, in theory and with some case examples.
Attitude & Empathy
More than 70 percent of my practice is seeing second opinions and unhappy patients with complications. I take them on despite their complexity, skepticism and demanding nature and strive to have the right attitude and empathy when treating them. For surgeons who ask about how to approach difficult cases, I tell them I don’t differentiate between simple and complex cases; in my mind, every eye I operate on is precious, so I never let my guard down, from diagnosis to performance. You must be committed to safely taking each patient’s eye to its best vision potential.
Have a Full Toolbox
To help me approach difficult cases, I’ve developed a surgical system called KLEAR (Full Spectrum Kerato-Lenticulo-Refractive surgeries). As the name implies, KLEAR involves a mélange of refractive, corneal and lens procedures, including staged and combined techniques. Since these patients’ problems can have many “moving parts,” properly planning the steps for them can be a challenge; in fact, KLEAR combines a group of personal surgery algorithms I’ve nicknamed the Gulani Planning System. This method takes a holistic approach to the visual system, individually tailored to each eye’s particular problems.
For the procedures I plug into this algorithm as needed, I’ve developed a surgical approach called “Plastique,” which is composed of “Corneoplastique” for cornea; “LaZrPlastique” for laser vision techniques and “LenzOplastique” for lens-based surgeries, including cataracts. Within Plastique is a mindset of a commitment to fight for each patient’s best vision potential. This includes not just fixing the problem at a basic level (like repairing a broken leg and giving the patient a cane), but instead striving for actual improved visual function (instead of needing a cane, the patient can eventually go running after the surgery). I also try to do this in the least interventional and most aesthetically oriented way possible, allowing the patient to enjoy a comfortable surgical and post-surgical experience. This, of course, makes it a bigger challenge, and my work becomes more difficult. In the end, however, it’s worth it.
Following are a sampling of cases that show my particular approach in action.
Case 1
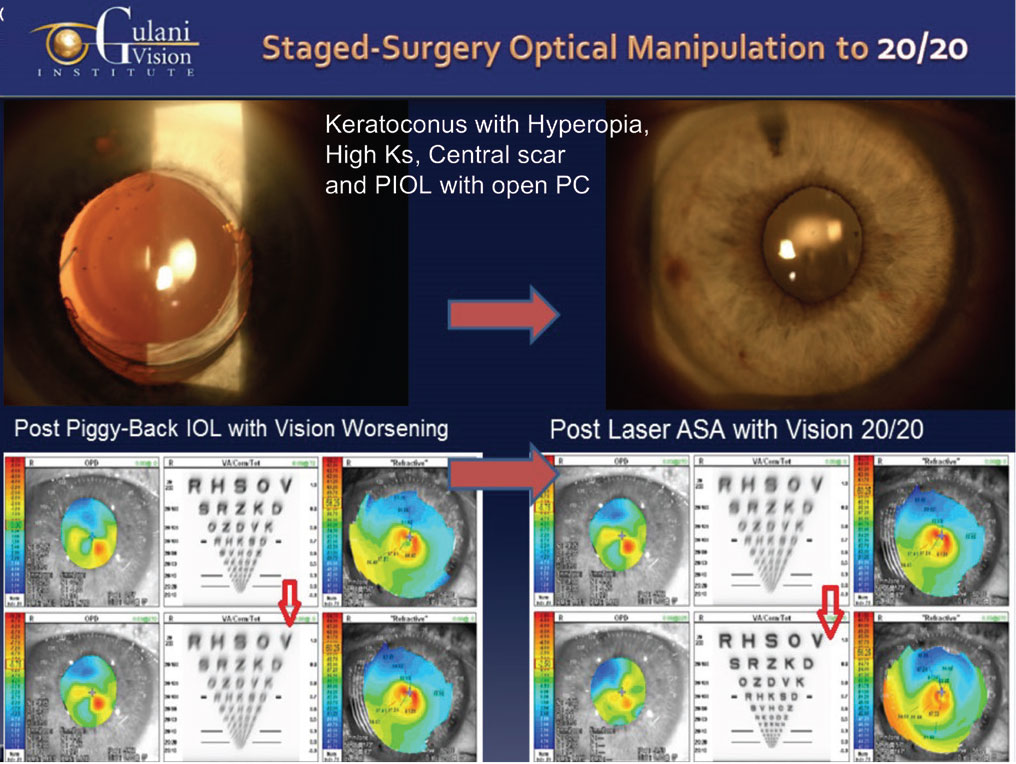
This 74-year-old with keratoconus underwent premium cataract surgery, and his surgeon performed a YAG capsulotomy. The patient was left with hyperopia, presbyopia, an anterior superficial scar and high keratometry; he was miserable, because his vision was 20/200. This patient also happened to be a pilot.
 |
|
Figure 1. A 74-year-old with keratoconus presented with hyperopia, astigmatism and central scarring. (See Case 1) Dr. Gulani first made the patient myopic with a piggyback lens, followed by myopic refractive surgery six weeks later. |
Many excellent eye surgeons he consulted told him that his surgeon had made a mistake, that they would approach his case by first removing this “wrong” lens implant and then attaching a new, scleral-supported lens implant (stitched/glued/iris-supported, etc.) since the posterior capsule was open. Now, none of these able surgeons was wrong, but here’s where my attitude and empathy differ (surgical acrobatics does not translate to vision artistry): Removing this lens implant and stitching a new lens implant with vitrectomy won’t bring the patient to unaided 20/20 vision.
The patient was facing many vision issues: astigmatism, farsightedness, and central scarring. For all of these to be corrected, I needed to perform myopic laser surgery. However, he was hyperopic. Keeping the Plastique mindset of going the extra mile, my first thought was: How do I make him myopic?
Because of his steep keratometry (due to keratoconus), he had a deep chamber, and he already had a lens in place (with open posterior capsule), so I put a piggyback lens in and made him myopic. He was then myopic with astigmatism, central scarring and high keratometry. Six weeks later, upon determining stability, I performed myopic laser refractive surgery. The patient ended up 20/20-plus uncorrected—he actually had 20/15 vision—and he got his pilot’s license back.
This also shows the patient’s trust, because I made him worse in the first stage in order to then move forward to my goal (keeping the two procedures minimally interventional, brief, painless, topical and aesthetically pleasing).
Case 2
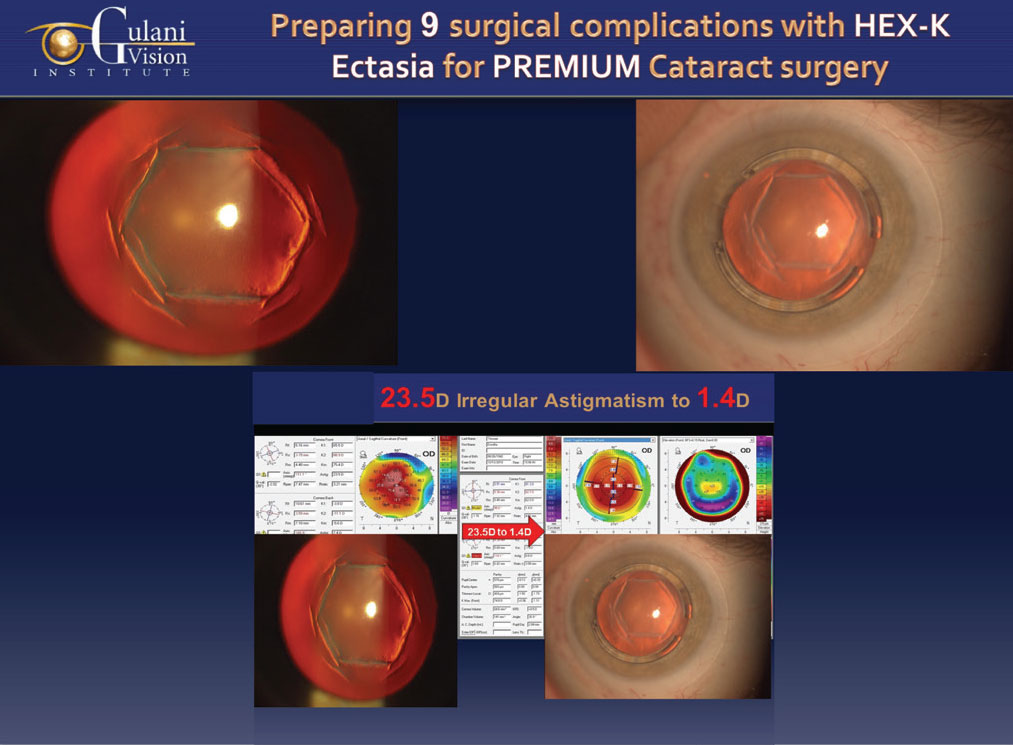
An 80-year-old female patient presented with a history of hexagonal keratotomy, the opposite of radial keratotomy, performed nearly 30 years ago. As some may recall, with Hex-K, the surgeon makes hexagonal-shaped cuts on the cornea. Unfortunately, we now know that this procedure destabilizes the entire cornea and, as a result, this patient wound up with 23.5 D of irregular astigmatism and keratometry of 89 D. She also had cataract, Fuchs’ dystrophy and thyroid exophthalmos. She was told nothing could be done except for corneal transplant and lens surgery.
 |
|
Figure 2. Patient with Hex-K and 23.5 D of irregular astigmatism (Case 2), was brought to 1.4 D after Intacs surgery. |
My goal, however, was to get her to 20/20. Taking into account her vision issues and related anatomical challenges, I first implanted Intacs around the hexagonal cuts. I did this confidently, yet carefully; if I came too close to the center, I’d tear into the cuts and perforate the cornea and if I went too peripheral, I’d be hitting the sclera. Having successfully inserted both the rings to “hug” the destabilized, ectatic corneal area inside the hex cuts, and having achieved my titratable central circular corneal reflex, I immediately cross-linked the cornea to make this effect permanent.
Four months later, I confirmed corneal stability and measurability. The procedure brought the irregular astigmatism down from 23.5 D to 1.4 D. I proceeded with cataract surgery with a toric IOL implantation, and brought her vision to 20/25. Fortunately, these two surgeries were brief, painless and aesthetically pleasing, and she now has visual freedom.
Case 3
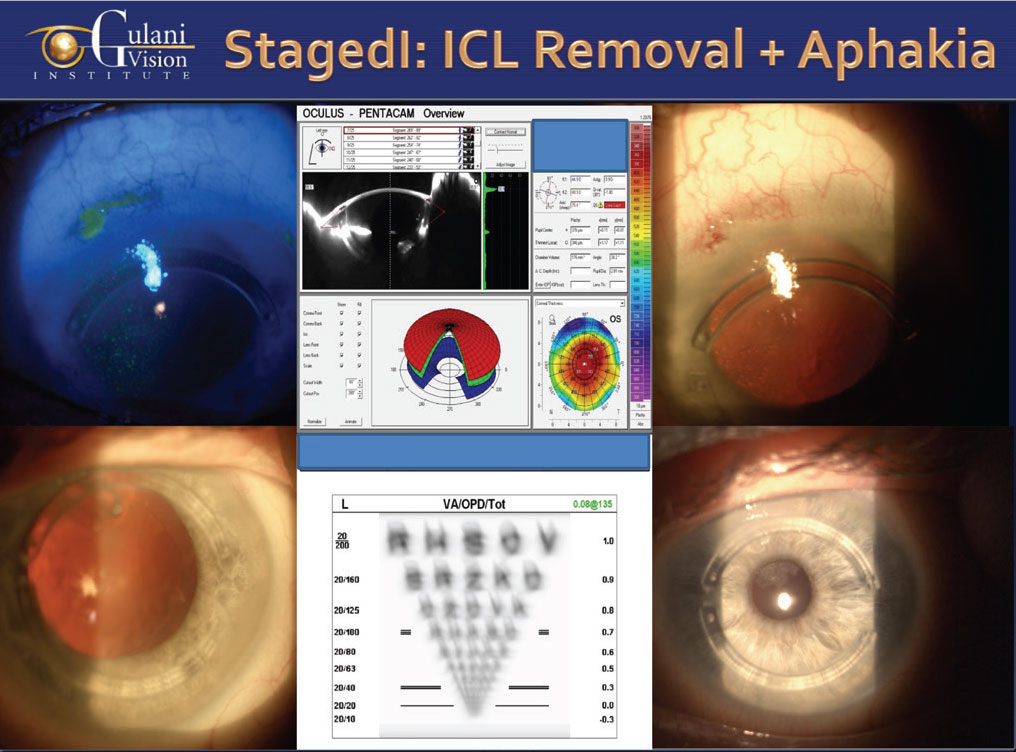
A 60-year-old male with keratoconus and a corneal scar came to me after 12 failed procedures. Among the 12 surgeries were Intacs, multiple corneal cross-linking procedures, PTK, PRK and ICL (the last being an example of a well-meaning surgeon who actually confuses the patient’s optics).
 |
|
Figure 3. After 12 failed procedures, this patient with keratoconus came to Dr. Gulani, who performed LaZrPlastique to remove his corneal scar, followed by removal of his cataract and ICL and implanting a toric IOL. (Case 3) |
The first step I did was LaZrPlastique on his corneal scar. This is a proprietary surface laser technique where I improve scars in a refractive mode. This removed his scar and made the cornea measurable. Because he also had a cataract and an ICL in the eye, I removed the ICL and the cataract, leaving him aphakic with an empty capsular bag (since I wasn’t confident his corneal measurements were good enough for an accurate IOL implantation). I measured his refraction the next day (using the Mackool-Gulani modified aphakic refraction technique) and, a week later, with full confidence, implanted a toric IOL. This brought him to 20/20 uncorrected.
Case 4
This next case shows how my thought process works. A 60-year-old man traveled to me with a history of radial keratotomy and a corneal transplant. He had since developed a cataract and also had high irregular astigmatism of 8 D and 20/200 vision. With this combination of procedures in his history, surgeons were hesitant to treat him any further.
However, it’s important to not let the difficulty level change your mindset about the patient. Fortunately, his cornea, no matter how astigmatic it was, was at least measurable. I went straight inside the eye and worked on the cataract and got him to 20/25. I did this through my LenzOplastique method in which I don’t just think about the cataract, I use cataract surgery as a vehicle to manipulate the optics and cancel the corneal abnormality. His postop topographical astigmatism was still around 8 D, but he could see 20/25 unaided and was thrilled with his outcome.
Case 5
This next case was a surgeon himself, with a history of a 20+ cut RK, a full-thickness, central blinding scar, more than 15 D of irregular astigmatism and cataracts. Vision was 20/400 uncorrected. And here’s the “best” part: Both eyes had this same complexity.
His team of ophthalmologists referred him to me. Even though his cornea was completely unmeasurable, I still didn’t want to do a full transplant and deprive him of his active lifestyle as a surgeon and golfer, so I performed my Corneoplastique-based, manual lamellar keratoplasty through the intersecting RK cuts to remove just the top layer of the scar. I then implanted a lamellar donor cornea without going inside the eye. Seventeen months later, I performed sutureless cataract surgery using a toric premium lens implant (LenzOplastique; lens-based surgery to optically cancel corneal anatomical complexities). As always, despite the complexities, I used only topical anesthesia without a sedative, and he saw 20/25. With the lamellar technique, the astigmatism went from 15.1 to 1.9 D, and the toric IOL treated the remaining cylinder. I repeated the same approach for the second eye, with similar results.
Case 6
This 73-year-old female was referred to us with poor visual outcomes following premium cataract surgery with multifocal lens implant followed by YAG laser capsulotomy. Her surgeon, in an effort to correct the hyperopic surprise, performed multiple PRK surgeries and caused a corneal scar. She was relegated to a corneal transplant with lens implant exchange along with vitrectomy by many surgeons she consulted. When she arrived I noted her vision issues and planned my least interventional, yet still “Plastique,” approach.
I first proceeded with LaZrPlastique to refractively clear the corneal scar to make the cornea measurable and stable. We then implanted a piggyback IOL in the same eye using LenzOplastique principles, which resulted in a 20/25 visual outcome.
These everyday cases at our institute are examples of how having a spectrum of techniques and technologies and, more importantly, a good attitude and empathy for each and every patient, enables you to handle the most complex refractive, corneal and premium cataract surgical failures or complications. Even if you have to go in reverse first, and then sideways, you’ll eventually end up going forward and enhancing the patient’s outcomes. Don’t be apprehensive about stepping out of your comfort zone and only doing things “by the book.” Also, don’t focus on surgical acrobatics that deprive patients of 20/20 unaided vision. I have numerous patients flying to me, disgruntled that their surgeons were happy with a smooth topography, clear corneal transplant or well-centered secondary lens implant while the patient was suffering from less-than-optimal vision.
To use a metaphor from the culinary world: Focus on the “vision recipe,” not just one ingredient (lens implant). I want my colleagues to use their ingredients, tools and recipes to take every patient—from the simple to the complex—to great vision and become master chefs.
Dr. Gulani is the founder of Gulani Vision Institute in Jacksonville.




