Despite advances in various technologies, LASIK monovision remains the most popular option for eligible presbyopes. Surgeons say the key word is “eligible,” and stress that it’s important to select the right patients who are ready and willing to adapt to a new way of seeing the world. Here, several experienced refractive surgeons share their tips on how they evaluate patients’ eligibility for monovision, and take a look at what might be the next generation of monovision treatment.
Passing the Test
Surgeons say they take care in evaluating patients for monovision in order to increase the likelihood of success.
“If patients have used monovision with contact lenses, they’re usually great candidates,” says Deepinder Dhaliwal, MD, director of the cornea and refractive surgery service at the University of Pittsburgh Medical Center. “As presbyopes, it also depends on how particular they are about their vision. If it’s someone who doesn’t do a lot of close work, just reads casually, that type of thing, I think that’s a great candidate.” Dr. Dhaliwal prefers a monovision trial in the phoropter to a contact lens trial in most cases. “If they’re looking at the chart binocularly and don’t notice the blur in one eye, I think they’ll do very well, typically,” she says. “So I don’t always do a contact lens trial for every monovision candidate, because the nice thing is, if they end up hating monovision, I can always enhance them.”
Though surgeons differ a little on how they decide how much anisometropia to create with the monovision, they all agree that -1.5 D is probably the upper limit. “The amount of monovision I create is partly based on age,” says Ronald Krueger, MD, director of refractive surgery at the Cleveland Clinic. “If the patient is in his very early 40s, I’d do what I call half monovision, something like -0.75 or -1 D. If they’re in their later 40s or in their 50s, I’d do closer to -1.5 D. The -1.5 D level is about a focus of two feet, which is enough to give them enough mid-range vision to be comfortable and enough reading to get by.”
Monovision also involves a lot of chair time where the patient is made to understand the effects of the procedure. “One of the big things about success with monovision is that it requires a discussion with the patient about the fact that it’s not a static process,” says Edward Manche, MD, director of cornea and refractive surgery at Stanford University’s Eye Laser Center. “It’s a dynamic process that changes over one’s life. In their 50s, at -1.5 D of monovision, they’ll lose the near vision but preserve the intermediate and distance. So, for example, reading a menu in dim light will become increasingly difficult.”
|
Laser Blended Vision
Professor Dan Reinstein, MD, FRCSC, of the London Vision Clinic in the United Kingdom, developed a new approach which modifies monovision laser vision correction and was implemented by Carl Zeiss Meditec as a software upgrade called Presbyond Laser Blended Vision for the MEL 80 excimer. One of the laser blended vision’s main goals is to create a blend zone of vision between the patient’s eyes at intermediate focal distances.
“The challenge in treating presbyopia is to achieve good binocular vision at far, intermediate and near distances while also maintaining optical quality,” says Dr. Reinstein. “The well-established principles of contact lens monovision have been used in laser refractive surgery, but many of the limitations of contact lens monovision also affected laser refractive surgery-induced monovision. These limitations include loss of fusion due to anisometropia, poor intermediate vision, poor distance vision in the near eye, reduced binocular contrast sensitivity, and reduced—or even broken—stereoacuity.
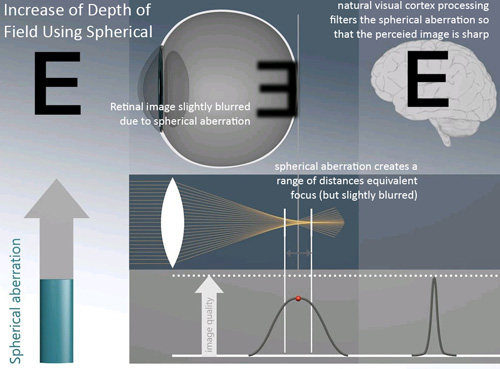
“Therefore, with Laser Blended Vision we incorporated another natural visual process—filtering of spherical aberration—to increase the depth of field in each eye and achieve good binocular vision at all distances,” Dr. Reinstein continues. “Introducing some spherical aberration disseminates the retinal focal point, meaning that there is a wider range of distances where the focus is equivalent, although slightly reduced, but the perceived image is still sharp due to the natural ability of the visual cortex to ‘process’ spherical aberration. This range is the depth of field and can be demonstrated by the better-than-expected distance vision in the near eye; the mean visual acuity is about 20/45 whereas 20/80 would be expected for -1.50 D.” He says that when this increased depth of field is combined with a micro-monovision (i.e., relatively lower degree of anisometropia), good near vision can be achieved with a functional level of uncorrected stereoacuity—provided that the patient has binocular function. Dr. Reinstein notes that too much SA, however, results in the visual cortex no longer being able to process it, resulting in quality of vision symptoms.
The typical candidate for Presbyond LBV is anyone who would be eligible for LASIK with the Carl Zeiss Meditec MEL 80 excimer and who passes the +1.5 D test.
For the LBV procedure itself, Dr. Reinstein considers a number of factors, including the patient’s age, accommodative amplitude, preoperative wavefront, tolerance of anisometropia and the amount of refractive error. “The software then combines these factors to generate an ablation profile with the aim of leaving the patient with an appropriate level of spherical aberration in order to maximize the depth of field without compromising contrast sensitivity, stereoacuity or night vision.”
In a study Dr. Reinstein performed using LBV, at one year, he reported that binocular uncorrected distance vision was 20/20 or better and uncorrected near vision was J2 or better in 95 percent of 136 myopic patients (≤ -8.50 D), 77 percent of 111 hyperopic patients (≤+5.75 D), and 95 percent of 148 emmetropic patients (within ±0.88 D). “The safety was the same as for standard LASIK, with no eyes losing more than one line of CDVA and contrast sensitivity was either the same or slightly better than preop,” he says.
Dr. Reinstein says the procedure works because it is based on the way our brain interprets retinal images. Says he, “The key to this approach was to base it on the natural mechanisms of spherical aberration processing and binocular fusion.”
REVIEW