Epithelial ingrowth may prove benign or become a real threat to good vision. Decisions about when and how to spring into therapeutic action are multifactorial, and there are several potential modalities from which to choose. Here, surgeons share their insights on when to intervene, and their preferred methods of banishing—and keeping out—epithelial ingrowth.
Jeffery J. Machat, MD, FRCSC, DABO, medical director of Nvision Eye Centers in Toronto and San Francisco, notes that surgeons saw much more epithelial ingrowth in the days of mechanical flaps than they do now. “Today, with femtosecond laser-created flaps, the incidence is about one-tenth what it used to be, or around 0.2 percent,” he says. “Most mechanical flaps are created with a blade with an angle of 26 degrees, as opposed to a more perpendicular side cut created with a femtosecond laser, usually about 75 to 110 degrees. This difference in architecture makes it far more difficult for epithelial cells to enter the interface of a femtosecond laser flap.”
Another reason that epithelial cells infiltrate femto-created flaps less often, according to Dr. Machat, is their firmer adhesion over time, although late enhancements still increase the risk. “If one performs an enhancement at 18 months or longer, then the risk of epithelial ingrowth will increase once again,” he explains. “For this reason, many surgeons have turned to PRK on the surface of the flap, to creating a side cut and then lifting the flap, or to cutting an entirely new flap.”
Bennie H. Jeng, MD, professor and chair of the Department of Ophthalmology and Visual Sciences at the University of Maryland School of Medicine, adds that LASIK flaps relifted and dislodged by trauma are another cause of ingrowth. “There are two main circumstances were we see epithelial ingrowth: One is after re-treatment; the other is after some traumatic event to the flap, where the patient is poked in the eye or something like that as late as 10 years or longer post LASIK. However it happens, if you relift the flap and put it back down, you’ll have a higher incidence of epithelial ingrowth,” he says.
When to Treat
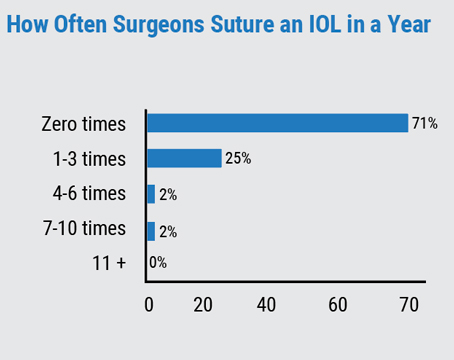
“The first thing to understand is that epithelial ingrowth will typically be noted at the slit lamp between one week and one month,” says Dr. Machat. One way to stage epithelial ingrowth is with Dr. Machat’s own grading scale, which ranks it from Grades 1 to 3.1 “If it is what I term Grade 1 ingrowth, you’ll simply see cells within 1 to 2 mm of the flap edge. As long as there’s a demarcation line, an area of scarring at the anterior edge of the epithelium, then we know that the epithelium will not grow any further. Grade 1 is usually just a very flat layer of epithelial cells that are noted incidentally near the flap edge. They just don’t progress, and no treatment is indicated,” he says. Grade 3 describes gray, necrotic geographic ingrowth and flap changes that include melting.
“You don’t go after it just because it’s there,” says Dr. Jeng. Let’s say somebody had LASIK redone about two years ago; they come in for follow-up and they have epithelial ingrowth. I might see them about three months later to make sure it hasn’t moved. I’ll also take a picture of it. But if it’s not causing any visual symptoms, then I don’t do anything. If it is extensive, or if it enters into the visual axis, then obviously it’s become a problem. If it’s progressing, or if it’s causing some overlying flap melting, then you have to lift it,” he says.
“Indications for treatment are: a symptomatic patient; a raised flap edge that is causing a foreign-body sensation; distortion of visual acuity; encroachment on the visual axis; induction of astigmatism, and asymmetrical glare,” says Dr. Machat. He warns that there are clear signs
 |
| A rolled LASIK flap edge can result from untreated epithelial cell ingrowth that advances in a line. Even after the ingrowth is treated, the change in flap architecture leaves a path for cells to re-enter. |
that demand immediate treatment. Grade 2 ingrowth “is where there is no demarcation line, and it looks like there’s a little peninsula of cells that comes in from the flap-edge margin. Often, the cells are vacuolated. They start to have a geographic appearance, almost like map dot dystrophy. These dead epithelial cells are the reason surgeons worry about epithelial ingrowth: They contain collagenase, which can then melt the corneal flap. So progressive ingrowth with no demarcation line, elevation of the flap edge, induced cylinder, changes on topography, dry spots, symptomatic glare, or necrotic cells should be treated on an urgent basis.”
Lift, Scrape, Seal
Once you’ve decided to treat, Dr. Machat and Dr. Jeng emphasize the importance of getting rid of all the cells and then approximating and securely re-sealing the flap to prevent their return. If you spot it early enough, says Dr. Machat, treatment can be very simple. “Sometimes, if it’s very minimal at the flap edge and you see necrotic cells, you can take a Sinskey-type spatula right at the slit lamp and just get those cells out from underneath the edge, and then use a dry spear and approximate the flap without taking the patient back to the laser suite. “It’s a nice technique because you can directly visualize what you’re doing through the slit lamp. However, you have to have a cooperative and steady patient.”
More often, however, “Treatment involves lifting the flap and scraping both the bed and the under-surface of the flap,” Dr. Machat continues. “I use a 64 Beaver blade (Beaver-Visitec; Waltham, Massachusetts), followed by dry surgical spears with copious irrigation,” says Dr. Machat. “Some surgeons will use PTK. In a dark room, epithelial cells will light up, and they should just do 5 μm [of PTK depth]. The key is to recognize whether the edges of the flap realign tightly,” he stresses. “If there is a rolled edge or a scalloped edge from corneal melt, a recurrence of epithelial ingrowth is far more likely. In these cases, tissue glue can be used; so can interrupted sutures.”
In addition to carefully debriding both the stromal bed and underside of the flap to get rid of all the cells, Dr. Jeng emphasizes that it’s critical to find their source. “You really want to see where these cells are coming in; generally they’re coming in from just one area under the flap. You have to look for that very carefully at the slit lamp. The key after doing this is that you have to suture the flap down: You have to—for sure—put a suture where the epithelium was coming in. I generally also do a few more around the flap,” he says. “If you do it right, the cells won’t come back. I really think that suturing it down is the main thing you have to consider; all the rest is sort of an adjunct.”
Although fibrin glue has also produced good results preventing significant recurrence of epithelial ingrowth in post-LASIK eyes after debridement,2 Dr. Jeng doesn’t use it to seal out the cells. “I think suturing is better,” he says. “I think a lot of people like the adhesive because it’s easy to use. But the tradeoff for easy is that it’s also easy for it to dislodge. If it doesn’t hold for long enough, you can still get ingrowth underneath. Adhesive is also very expensive.”
As an alternative to flap relift and debridement, some surgeons use a neodymium:YAG laser to eliminate symptomatic epithelial ingrowth after LASIK. YAG (0.6 to 0.8 mJ) photodisruption has been shown to significantly improve UCVA and astigmatism symptoms and topography in phakic, post-LASIK re-treatment eyes with Grade 2 to 3 ingrowth affecting visual acuity.3
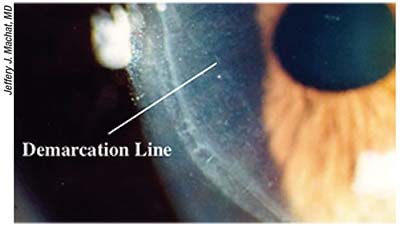
“Some surgeons, if they see an epithelial nest that was actually introduced
 |
| A neodymium-yttrium (YAG) laser can be effective for killing epithelial cells that have encroached on the visual axis. An eye immediately post YAG treatment is shown here, with bubbles over the targeted ingrowth. |
by the surgeon during treatment and not contiguous with the edge of the flap, use a YAG laser to kill the cells so they don’t grow,” says Dr. Machat, who adds, “I’ve never used that technique—I worry too much.”
“I find it very unsettling to YAG the cornea,” agrees Dr. Jeng. For epithelial ingrowth that’s infiltrating the eye through an opening other than a LASIK flap, such as a wound, however, he will consider changing up his strategy of debridement. “I might focally cryo the area,” he states. “If the ingrowth was severe enough, that’s something that I would consider, but then you’d kill off an area of the stem cells so that it can’t grow the epithelium.”
Repeat as Necessary
“I’m going to say this, and then I’m knocking on wood, but I’ve never had epithelial ingrowth recur after I’ve stitched the flap down,” says Dr. Jeng. “That said, just because it recurs, that doesn’t mean you have to intervene. But if it does recur, and if it does continue to progress, you have to relift it. Presumably, this would be at a point after you’ve already taken out your original set of sutures if you’re following the patient. I think that if you lift the flap again and go through the same steps, you can use any of the adjunctive methods you want. I’m not a huge fan of mitomycin-C, since I’m not really sure that it works. Isopropyl alcohol is more of a local thing that goes away once it’s done its job, so the epithelium will kind of grow back over it,” he says.
“We’re only about 80-percent effective in eliminating epithelial ingrowth once it’s occurred,” Dr. Machat estimates. “If you have to re-treat, then it’s about 80-percent odds again. Only if the ingrowth is very minimal, your first treatment can be around 98-percent effective; but if you let ingrowth progress to, say, Grade 3, then it’s only 80-percent effective.”
Epithelial cells that sneak under the LASIK flap, like unwanted guests you’ve politely shooed away, have some propensity to come back even after you make it clear they’re not welcome. “The biggest thing is that if you don’t treat rapidly advancing epithelial ingrowth that has no demarcation lines, or necrotic epithelial cells, the wall of cells that moves in can literally pull the flap edge underneath it, so it’s rolled,” says Dr. Machat. “I describe it to patients as similar to a worn-in walking path in a park or forest: That path has been created, and cells will grow back all over again.” With careful observation, clinical judgment and persistence, your patient’s LASIK flap needn’t be a gateway to rogue epithelial cells. REVIEW
Neither Dr. Machat nor Dr. Jeng reports any financial interests relevant to this article.
1. Machat JJ, Slade SG, Probst LE. The art of LASIK. 2nd ed. Thorofare, NJ: Slack; 1999.
2. Hardten DR, Fahmy MM, Vora GK, Berdahl JP, Kim T. Fibrin adhesive in conjunction with epithelial ingrowth removal after laser in situ keratomileusis: Long-term result. J Cataract Refract Surg 2015;41:1400-05.
3. Fuentes-Paez G, Soler Jr, T, Ddo, BS. Epithelial ingrowth: Visual acuity and astigmatism results one year after YAG laser treatment. J Clin Exp Ophthalmol 2015;6:5. http://dx.doi.org/10.4172/2155-9570.1000471. Accessed 25 April 2018.