Low-level astigmatism (0.25 to 1.25 D)is not an uncommon finding in eyes presenting for cataract surgery, and it represents a treatment opportunity.1 Correcting for nearly distortion-free vision may make patients even happier with their new IOLs. Here, experienced refractive cataract surgeons explain the importance of considering the role even slight astigmatism plays in visual outcomes, and share techniques for decreasing it as much as possible.
How Much is Treatable?
Robin Vann, MD, assistant professor of ophthalmology at Duke University and medical director of Duke Eye Center’s operating rooms, says that surgeons who ignore small amounts of astigmatism are missing out an a relatively easy avenue to patient satisfaction. “A lot of cataract surgeons seem to have this concept regarding astigmatism treatment, that they’ll be very selective about who they’ll start with. They’ll say things like, ‘I’m not going to offer this treatment to anyone with under two diopters of astigmatism.’ But I believe that’s really flawed thinking because the vast majority of American patients have low amounts of astigmatism; the majority has between one and two diopters. You’re essentially excluding an awful lot of patients if you hold off until people present with higher amounts of astigmatism,” he says.
“I generally try to get patients to have less than half a diopter of astigmatism if I can,” Dr. Vann explains. “Assuming they’re not myopic or hyperopic with spectacles or after surgery, most patients can tolerate up to a half-diopter of astigmatism, and in some cases 0.75, before they can’t read the 20/20 line. So that would be acceptable for most patients. While I’d love to make astigmatism zero in every case, we don’t yet have a tunable lens implant in our hands to make that goal realistic.” Dr. Vann notes that the RxSight lens, FDA approved in November 2017, is not yet commercially available.
Limbal Relaxing Incisions
Limbal relaxing incisions are a safe and straightforward astigmatism treatment option during cataract surgery.2 Complications such as infections are rare, although potentially serious.3,4 Both monofocal implantation with LRIs and toric lens implantation for low astigmatism can significantly improve mean uncorrected visual acuity, although torics may produce slightly better visual outcomes.5 Tal Raviv, MD, FACS, associate clinical professor of ophthalmology at the New York Eye and Ear Infirmary of Mount Sinai Icahn School of Medicine at Mount Sinai, and the founder and medical director of the Eye Center of New York, thinks torics are the best option. “We’ve learned more about astigmatism planning in the past half-decade than ever before. We know that toric IOLs are more accurate than LRIs, so we should use torics whenever possible,” he says.
“In my practice there are three reasons for patients to get LRIs instead of torics,” says Dr. Vann. “Number one is if their astigmatism isn’t great enough to warrant a toric lens implant. I have the Barrett Toric Calculator printed out as part of my biometry calculations for formulas: If it’s telling me not to put in the lowest-powered toric—a T2 [Alcon ReSTOR, 1 D of cylinder correction], for example, and the field is just blank, then the patient doesn’t qualify for a toric. I’ll think about doing LRIs to reduce their astigmatism when they’re greater than a half diopter but not high enough to warrant a toric.
“Another situation is where a patient unfortunately just can’t afford a toric,” Dr. Vann continues. “The third scenario is when the ocular surface of the eye makes it very difficult to get accurate readings. In those cases I may delay, or I may determine that I don’t want to be doing astigmatism management with torics in unusual eyes. Irregular astigmatism might be an example; or a patient with bad keratoconus or with dry eyes so severe that you can’t even do good biometry testing.” He also says that patients with irregularities to the contours of their eyes due to conditions such as Salzmann’s nodular degeneration and anterior basement membrane dystrophy may be poor candidates for toric lenses.
Although LRIs are simple and effective, Dr. Vann says that some patients become disappointed if they can’t try a toric IOL for astigmatism treatment, in part because new patients in his practice get an overview of the exciting premium and toric IOL technologies available. “Unfortunately, they may get all pumped and excited about these technologies, and then I’ve got to tell them, ‘Sorry, but I can’t use them in you.’ So sometimes you have to gently bring patients back to reality.”
Toric Tips
For patients who are good toric-IOL candidates, Dr. Raviv urges surgeons to correctly factor the astigmatism that any type of incision will induce into lens selection. “We haven’t been properly calculating surgically induced astigmatism in the past. Instead, we’ve just entered numbers such as 0.5 D for 2.75-mm corneal incisions,” he explains. “It turns out that the net vector induced astigmatism is quite randomly distributed, and best practice today is to calculate centroid surgically Induced astigmatism using Warren Hill’s SIA Calculator, or to simply use 0.1 D, which likely covers most temporal incisions from 2.2 to 2.6 mm.”
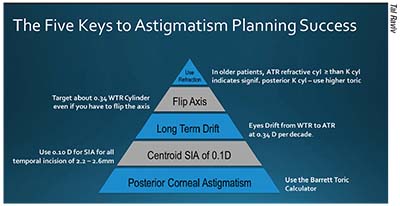 |
| Dr. Raviv has developed this visual aid to help surgeons remember keys to astigmatism management with toric IOLs, such as taking into account the tendency of astigmatism to drift from WTR to ATR at the rate of about 0.34 D per decade, and the importance of posterior corneal astigmatism in lens selection. |
Dr. Vann encourages patients with less than 2 D of astigmatism to consider torics if they can afford them. “I think that for treating astigmatism, the toric lens implant is a tried-and- true technology. There are now several publications demonstrating that toric lens implants tend to leave less residual astigmatism and provide better long-term vision. I think they work incredibly well,” he says.
“For astigmatism treatment at the time of cataract surgery, use toric IOLs whenever you can—roughly speaking, for with-the-rule astigmatism greater than 1.5 D and against-the-rule greater than 0.4 D,” recommends Dr. Raviv. He adds that it’s especially important to neutralize astigmatism to get good results with presbyopic IOLs. “Because most cataract patients are older, with high prevalence of against-the-rule astigmatism, I find that more than half of my presbyopia-correcting IOL patients get the toric version.”
Dr. Vann notes that a good workup is the foundation for good results, and that if your preoperative workup and measurements are uniformly thorough and comprehensive, you needn’t vary your workup too much for toric-lens patients. “For a very long time, we were very selective in how we did our preoperative testing, but in order to meet our volume demands while trying to offer all of our patients all of the services that they’re eligible for, we ultimately decided to simply do testing consistently across the board. So if somebody’s coming to me for a cataract evaluation, they’re going to get a standard set of tests,” he explains. “If their tests on the first pass aren’t up to snuff, I’m going to repeat the suspect testing; and if they have a lot of astigmatism, then that might include repeating not just the biometry, but also the topography. I do biometry and topography on just about everyone unless they have an incredibly small amount of astigmatism on the biometry testing, which we do before topography.
“It’s important to use a methodology that’s going to give you a high degree of accuracy,” Dr. Vann continues. “I use the Verion image-guided system so that I’ll have the reference vessels of the eye to determine where zero and 180 degrees are. We actually did a study that we haven’t published, that found a high degree of correlation of the Verion axis with the axis of my Lenstar (Haag-Streit). I use the Lenstar values to help me determine where to orient the toric lens implant, and the Barrett Toric Calculator. So if Barrett tells me axis 175, I program the Verion to show me where axis 175 is in the OR, and then put a mark on the cornea right at the start of the case. I’ve also had ORA [intraoperative aberrometry] for the past two years. I use it to help fine-tune the final alignment of the IOL, and in many cases it ends up being very similar, if not identical to, where the Barrett Toric Calculator axis is,” he explains, adding that ORA is his tiebreaker, provided that it’s capturing accurately. “In those cases, I will go wherever ORA tells me, even if it’s different from the Barrett Toric Calculator,” he says.
Dr. Vann stresses the importance of making sure that your intraoperative biometer is capturing accurately before you rely on its readings. “ORA is a diagnostic tool, not an interventional tool, so it just reads things and you have to interpret it. There are definitely situations where you’ll feel like it didn’t read correctly,” he says. “For example, I did surgery today, and I had a patient who was just too sleepy to fixate on the light, and so I was measuring the eye eccentrically, which was telling me that the readings from the machine were going to be inaccurate. I couldn’t trust what it was telling me, so I went with my preoperative alignment rather than what ORA told me in this case.”
Dr. Raviv emphasizes the need to account for posterior corneal astigmatism when selecting an IOL. “We need to overtreat against-the-rule astigmatism and undertreat with-the-rule astigmatism. He recommends the Barrett Toric Calculator, adding, “The Barrett has had better results than attempted direct measurements via Scheimpflug or LED light topography. Swept-source OCT posterior corneal astigmatism measurement, however, may prove to be even more accurate.”
Age-related Considerations
Dr. Vann says that patient age is an important factor in planning for astigmatism correction. “There have been quite a few publications that have come out in the past 10 to 15 years looking at astigmatism over time, and finding that there’s a general drift from with-the-rule astigmatism to against-the-rule, presumably due to constant blinking and gravity causing the cornea to sag a little over time,” he says. “So if somebody has half a diopter of astigmatism at age 50 that’s at axis 90, there’s a possibility that it can decrease towards the horizontal, towards 180, over the ensuing 20 or 30 years. If I’m operating on a relatively young patient, somebody under 70, I generally try to leave just a little with-the-rule astigmatism if I’m able to, to help counteract that drift over time.”
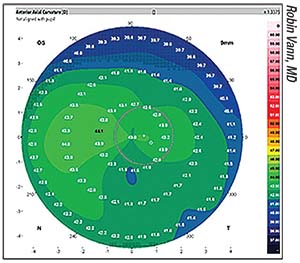 |
| OS topography. Corneal topography is an important component of preoperative workup for eyes with astigmatism. |
“Ken Hayashi, MD, PhD, has shown that eyes slowly drift from WTR to ATR,” notes Dr. Raviv.6 “The drift seems to be somewhere in the range of 0.34 D per decade, and should be kept in mind when selecting a toric power.” He adds that flipping the axis on a toric IOL is an acceptable way to make an allowance for the drift to ATR astigmatism. “Old advice about not flipping the axis on a toric IOL was a holdover from spectacle refracting advice, and doesn’t apply,” he says. “In fact, one should ideally target about 0.34 D of WTR either by flipping an ATR patient, or by undercorrecting a WTR patient to allow room for the natural drift.
“Also, old warnings about not paying attention to the refractive cylinder when planning a toric IOL—due to the assumption that it only represents ‘lenticular’ astigmatism—are wrong,” continues Dr. Raviv. “We know that the internal astigmatism also accounts for the posterior corneal cylinder. Older patients that have significant refractive ATR cylinder typically have high posterior corneal astigmatism and need a higher toric power than what’s obvious from looking at the anterior cornea alone. It’s not uncommon for a 78-year-old with a +2.00 -1.75 x 90 refraction and only 0.4 D of ATR corneal cylinder to require not just a toric, but a T4 (AcrySof; Alcon) or ZCT225 (Tecnis Toric; Johnson & Johnson Vision) to be properly corrected.”
Dr. Vann maintains that there’s little downside to revising one’s thinking on treating low-level astigmatism, because it takes no additional skill to treat compared to higher-order astigmatism, and it often results in happier patients. “If you’re going to get into this, you should always think of astigmatism every time you’re seeing someone for cataract surgery,” he says. “Don’t just wait for some value that’s around two diopters: You should always screen for 0.1, 0.3—it should always be part of your step-by-step analysis of a patient. When surgeons selectively filter, they can miss cases they could’ve treated with a toric lens implant.” REVIEW
Dr. Vann is a consultant to Alcon. Dr. Raviv is a consultant to Johnson & Johnson Vision, Ocular Therapeutix and Glaukos and Cassini.
1.Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cat Refract Surg 2009;35:70-5.
2. Budak K, Friedman NJ, Koch DD. Limbal relaxing incisions with cataract surgery. J Cat Refract Surg 1998;24:4:503-08.
3. Haripriya A, Smita A. A case of keratitis association with limbal relaxing incision. Indian J Ophthalmol 2016;64:12:936-7.
4. Haripriya A, Syeda TS. A case of endophthalmitis associated with limbal relaxing incision. Indian J Ophthalmol 2012;60:3:223-5.
5. Leon P, Pastore MR, Zanei A, Umari I, Messai M, Negro C, Tognetto D. Correction of low corneal astigmatism in cataract surgery. Int J Ophthalmol 2015;8:4:719-724.
6. Hayashi K, Hirata A, Manabe S, Hayashi H. Long-term change in corneal astigmatism after sutureless cataract surgery. Am J Ophthalmol. 2011;151:5:858-65.