Lasers
A prospective, randomized study from Brazil's Anelise Wallau, MD, and her co-workers found custom PRK with mitomycin-C to have some advantages over custom LASIK for patients with compound myopic astigmatism.
In the study, the surgeons randomized 88 eyes of 44 patients with a minimum estimated ablation depth of 50 µm to receive PRK with intraoperative 0.002% mitomycin in one eye and LASIK in the fellow eye. The average preoperative spherical equivalent refraction for the patients was
-3.92 ±1.6 D, and the average ablation depth was 71.89 ±14.31 µm.

Postoperatively, all the PRK eyes re-epithelialized within five days. At six months, 95 percent of all patients achieved 20/20 or better uncorrected acuity in both eyes. All of the surface ablation eyes and 97 percent of the LASIK eyes saw 20/20 or better best-corrected. The average cycloplegic spherical equivalent refraction postop was +0.52 ±0.34 D in PRK eyes and +0.55 ±0.57 D in LASIK eyes. There was no significant haze in any of the PRK eyes during the follow-up period. The researchers found a statistically significantly higher amount of higher-order aberration in the LASIK eyes than the PRK eyes at the three and six-month follow-up points. On a subjective questionnaire, patients rated their vision as excellent in 67 percent and 58 percent of the PRK and LASIK groups, respectively.
Atlanta surgeon George Waring presented the latest data on the U.S. Food and Drug Administration trial of Nidek's topography-guided Custom Aspheric Treatment Zone (CATz) procedure.
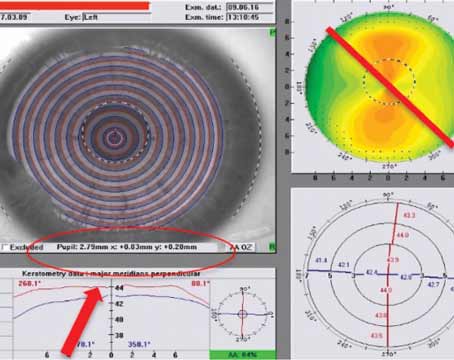
CATz operates by using Nidek's Optical Path Difference Scan imaging device to capture a topography of the eye. The data from the OPD Scan is used to create a shot file, which is transferred to the laser. The spherical and astigmatic corrections are completed using a scanning slit beam, while the irregularities are treated with a scanning spot. In the study, patients had from -0.5 to -7 D of myopia and up to -4 D of astigmatism.
Seventy-two eyes are now at the three-month follow-up point. All of the eyes are within 1 D of emmetropia and 93 percent are within 0.5 D. Eighty-three percent of the patients see 20/15, 86 percent see at least 20/20 and all patients see 20/40 or better. The postoperative uncorrected visual acuity is as good or better than the preoperative best-corrected acuity at the 20/12 and 20/16 levels, and no patients lost two or more lines of best-corrected acuity. There was a decrease in all subjectively reported visual symptoms, such as night-driving problems, except for ocular dryness, which increased in 2 percent of patients. Dr. Waring and his co-investigators will continue to follow a total of 145 patients.
Houston surgeon Stephen Slade presented the interim results of the FDA trial of Bausch & Lomb's Zyoptix wavefront-guided treatment of hyperopia and hyperopic astigmatism.
A total of 21 hyperopic patients (41 eyes) with an average spherical error of +1.98 ±1 D (range: 0.51 D to 4.47 D) and average astigmatism of +0.94 ±0.57 D (range: 0.21 D to 2.08 D) were available for their three-month follow-up.

The average manifest refractive spherical equivalent refraction decreased from +2.07 D to -0.23 D at one month and -0.14 D at three months. Seventy-five percent of the patients were within ±0.5 D of the intended refraction and 95 percent were within ±1 D. Seventy-one percent could see 20/20, 93 percent could see 20/25 and all patients were able to see at least at the 20/32 high-contrast acuity level. Eighty-four percent either gained a line or had no change in their best-corrected vision, 10 percent lost a line and 7 percent lost two or more lines. Eighty-eight percent of the patients reported being very or moderately satisfied, 12 percent were neutral and no one was dissatisfied. Dr. Slade says there were no treatment-related adverse events.
Lens Implants
Two surgeons provided data on the toric version of Staar's phakic Implantable Contact Lens. Munich surgeon Tobias Neuhann shared his six-year results with the implant, and David Tanzer, MD, of the San Diego Naval Medical Center, provided an update on the clinical trial of the lens.
Dr. Neuhann's study was composed of 84 eyes with myopia ranging from
-4 D to -14 D and regular astigmatism ranging from 1.5 D to
8 D. All of the eyes had anterior chamber depths of 2.8 mm or less and corneal diameters of 11 mm or larger.
Ninety-two percent of the eyes see 20/40 or better uncorrected and 39 percent have gained from one to four lines of best-corrected acuity. No eyes have lost any lines of acuity. Five of the lenses (5.9 percent) required readjustment to put them on the correct axis. One patient (1.2 percent) developed an intumescent cataract two weeks postoperatively that required removal. There were no cases of spontaneous ICL rotation, and the refraction stabilized on the fifth day postop. Dr. Neuhann says there were no halos, glare, regression or secondary glaucoma as long as the scotopic pupil diameter wasn't larger than the optic of the implant.
In Dr. Tanzer's report from the FDA toric ICL trial, 210 eyes of 124 patients received the lens. Preoperatively, patients had between
-2.38 and -19.5 D of myopia and from 1 D to 4 D of cylinder.
At the 12-month follow-up point, 83 percent of the eyes saw 20/20 or better uncorrected and 77 percent had a postop uncorrected acuity equal to or better than their preop best-corrected acuity. The average manifest refractive cylinder decreased from 1.93 ±0.84 D to 0.51 ±0.48 D, a change of 74 percent. While 21 percent of eyes had 1 D of astigmatism preop, 91 percent had 1 D or less after surgery. The mean manifest spherical equivalent refraction improved from -9.36 ±2.66 D to 0.05 ±0.46 D. The average best-corrected vision improved by 0.88 lines, with 76 percent of the eyes gaining one or more lines and 8 percent losing at least one.