Over the past decade or so, advancements in customized LASIK with guidance from topography or wavefront optimization/topography integrations have achieved outcomes that were previously rare. Surgeons who have mastered the techniques involved in both procedures are getting excellent results. Despite this, only a fraction of refractive surgeons have fully embraced the technology. We spoke with a few surgeons who swear by this segment of LASIK and asked about their experiences and what their peers should know before diving in.
What’s Available
It’s important to note the variations of customized LASIK treatments that are on the market today and how their outcomes stack up.
• Contoura Vision, Alcon. FDA approved in 2015, Contoura is a topography-guided LASIK treatment for patients with myopia and myopia with astigmatism.1 Contoura uses Alcon’s WaveLight Allegretto Wave Eye-Q or WaveLight EX500 Excimer Laser Systems in concert with the WaveLight Topolyzer Vario Diagnostic Device. In the FDA trials, 68.8 percent of patients achieved 20/16 or better UCVA at three months postop, and 31.6 percent achieved 20/12.5 or better.2
• iDesign 2.0 Refractive Studio, Johnson & Johnson Vision. Approved by the FDA in 2018, iDesign integrates topography with its wavefront-guided technology and is approved for myopia, hyperopia and mixed astigmatism.3 In one study, 74.1 percent of eyes undergoing wavefront-guided LASIK in conjunction with the iDesign aberrometer achieved UDVA of 20/16 at three months.4
• EC-5000 Advanced Vision Excimer laser system (NAVEX), Nidek. This system comprises the Quest M2/EC-5000CX, OPD-Scan III and Final Fit custom ablation software and was FDA approved for the correction of myopia, hyperopia and astigmatism in 2013. In the FDA trials, 48.8 percent of eyes treated for myopic astigmatism had a UCVA of 20/16 or better at three months.5
When it comes to evaluating topography-guided LASIK vs. other methods, there are some differences that may sway a surgeon to choose one over the other. In a meta-analysis6 comparing topo-guided LASIK with wavefront-optimized LASIK, there were no significant differences in the ratio of UDVA of 20/20 or better, or 20/16 or better; however, topo-guided had a higher proportion of postop manifest refractive spherical equivalent within ±0.5D of target and fewer surgically induced higher order aberrations, spherical aberrations and coma when compared to wavefront. On the other hand, topo-guided LASIK requires a bit of additional chair time to work the patient up, which some practices see as a disadvantage.
Either method chosen will result in better outcomes than older, non-wavefront-optimized LASIK, says Robert Maloney, MD, a cataract and refractive surgeon in Los Angeles. “What matters is giving our patients the best possible uncorrected vision we can give,” Dr. Maloney says. “We know from work done by Steve Schallhorn, MD, in which he looked at the correlation between patient satisfaction and uncorrected vision. He found that for each line of uncorrected vision, patient dissatisfaction doubles. So patients who are 20/15 uncorrected tend to be extremely happy. Patients who are 20/20 tend to be very happy, 20/25 pretty happy, 20/30 not so happy, 20/40 not happy. So we know that it’s really important to give people the maximum uncorrected vision and it’s very clear that the way we get there is by customizing the treatment to the patient.”
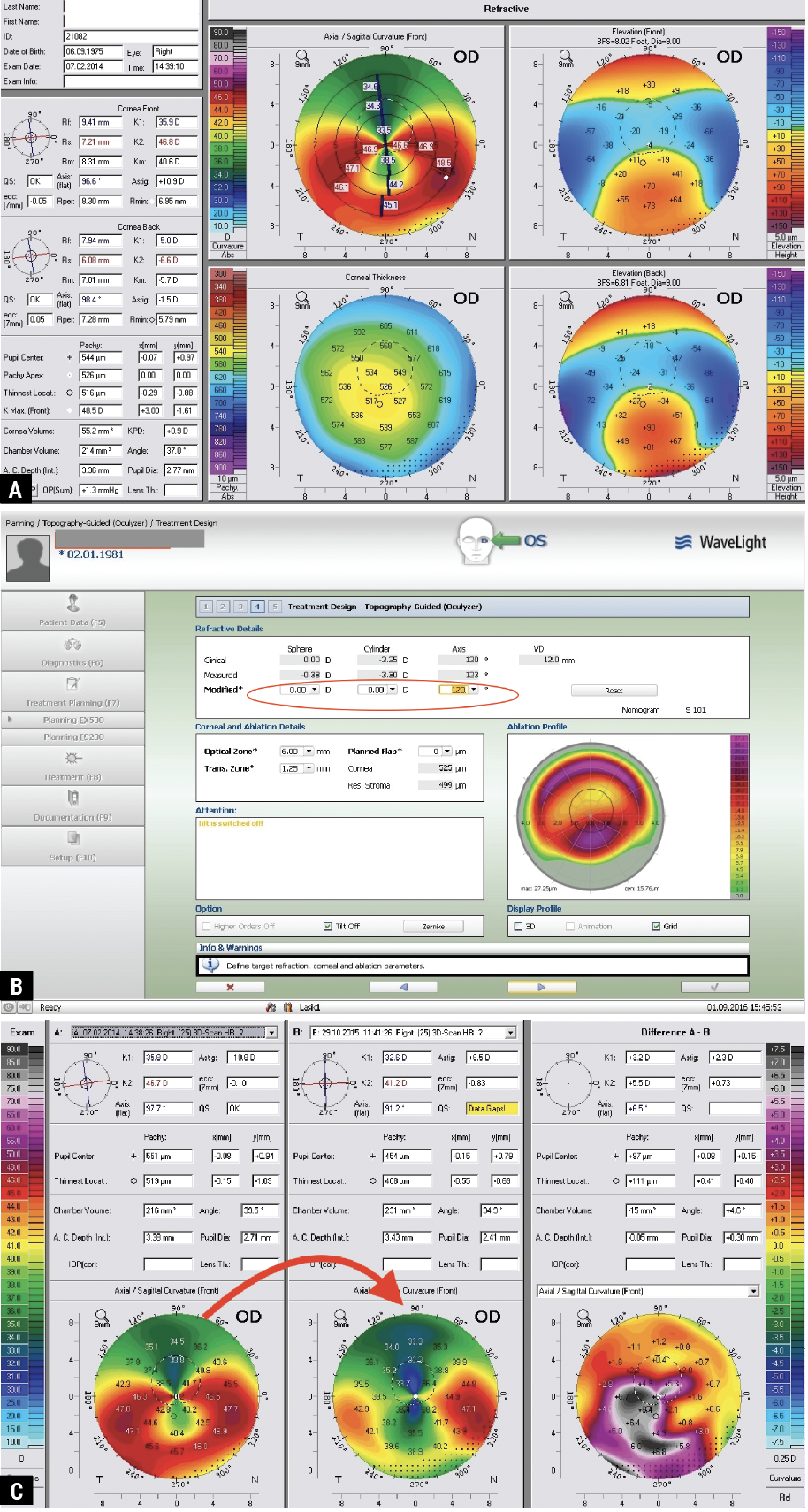 |
| This case from A. John Kanellopoulos, MD, is a 39-year-old with oblique keratoconus (and not pellucid as shown on the pre-Athens Protocol CXL Pentacam) (A). Shown is the EX500 excimer treatment plan for topography-guided surface ablation (B), followed by the difference preop (left) and postop (middle), and the combined topo-guided ablation with CXL (right) (C). (All images: A. John Kanellopoulos, MD). |
Early Adopters’ Experiences
While surgeons in the United States may still be mulling over whether they should invest in topography-guided LASIK, refractive surgeons in Europe have been using it for 20 years, though mainly for irregular corneas, which many surgeons think topography-guided is uniquely suited for. A. John Kanellopoulos, MD, who practices in Greece and is a professor of ophthalmology at NYU Medical School, says topo-guided LASIK was introduced to the European Union as a means to treat irregular corneas.
“We evolved the use of this technology as an enhancement in LASIK cases with outstanding results in visual function improvement for patients who were contact lens-intolerant,” says Dr. Kanellopoulos. “We applied it to irregular eyes such as keratectasia, keratoconus and post-refractive ectasia, and we were the first team to combine cross-linking with topo-guided treatments in what is now known as the Athens protocol.
“It was soon after that we realized the advantages of topo-guided treatments for naive myopic and hyperopic eyes as our data showed, for normal conical eyes, topo-guided offers the advantage of reshaping the cornea to become symmetric to the visual axis,” he continues. “Although most normal corneas function well, even that slight correction is able to offer gains in lines of vision, along with the correction of the refractive error.”
Mark Lobanoff, MD, a private practice refractive surgeon in Minneapolis, admits he always felt a bit jealous that surgeons in Europe had access to this technology. “Topo-guided LASIK was a repair procedure for patients who had off-center ablations or, in the case of some of the early excimer lasers which had very small optical zones and led to a lot of glare at night, or patients who had scars or irregular corneal topography,” says Dr. Lobanoff. “They could fix the patients who were struggling after LASIK but we couldn’t.”
Alcon initially wanted to conduct an FDA study on irregular eyes, says Dr. Lobanoff, but the FDA insisted it be first proven safe on virgin, healthy eyes. “To Alcon’s amazement, they had some of the best results ever seen after LASIK surgery,” he says. “An incredibly high percentage could see 20/20 or better. And so Alcon said, ‘We never thought about using this technology for standard, regular treatments.’ And so they branded it Contoura and released it in the United States. Immediately there were problems.”
Dr. Lobanoff was one of the first to introduce topo-guided LASIK in the United States and although some patients did well, a lot of them were ending up 20/25 or 20/30—a big difference from the 20/16 or better noted in the FDA results.
“I called up my mentor R. Doyle Stulting, MD, from Emory University (who ran the FDA study) and asked why my results weren’t as good as the study’s,” recalls Dr. Lobanoff. “And he said, ‘Mark, you have to understand the FDA study was a safety study, so no fewer than three cornea experts looked at every patient’s corneal topography before they were let into the study, and only corneas that were absolutely perfect were allowed in.’ In the FDA study, they treat off the patient’s manifest refraction. In the real world, patients have topographic irregularities in their cornea and if you treat on the manifest refraction, you get results that aren’t as good. A lot of doctors tried to come up with ways to treat it that made more sense—they all failed. And so after three or four attempts, Alcon was about to give up on the technology.”
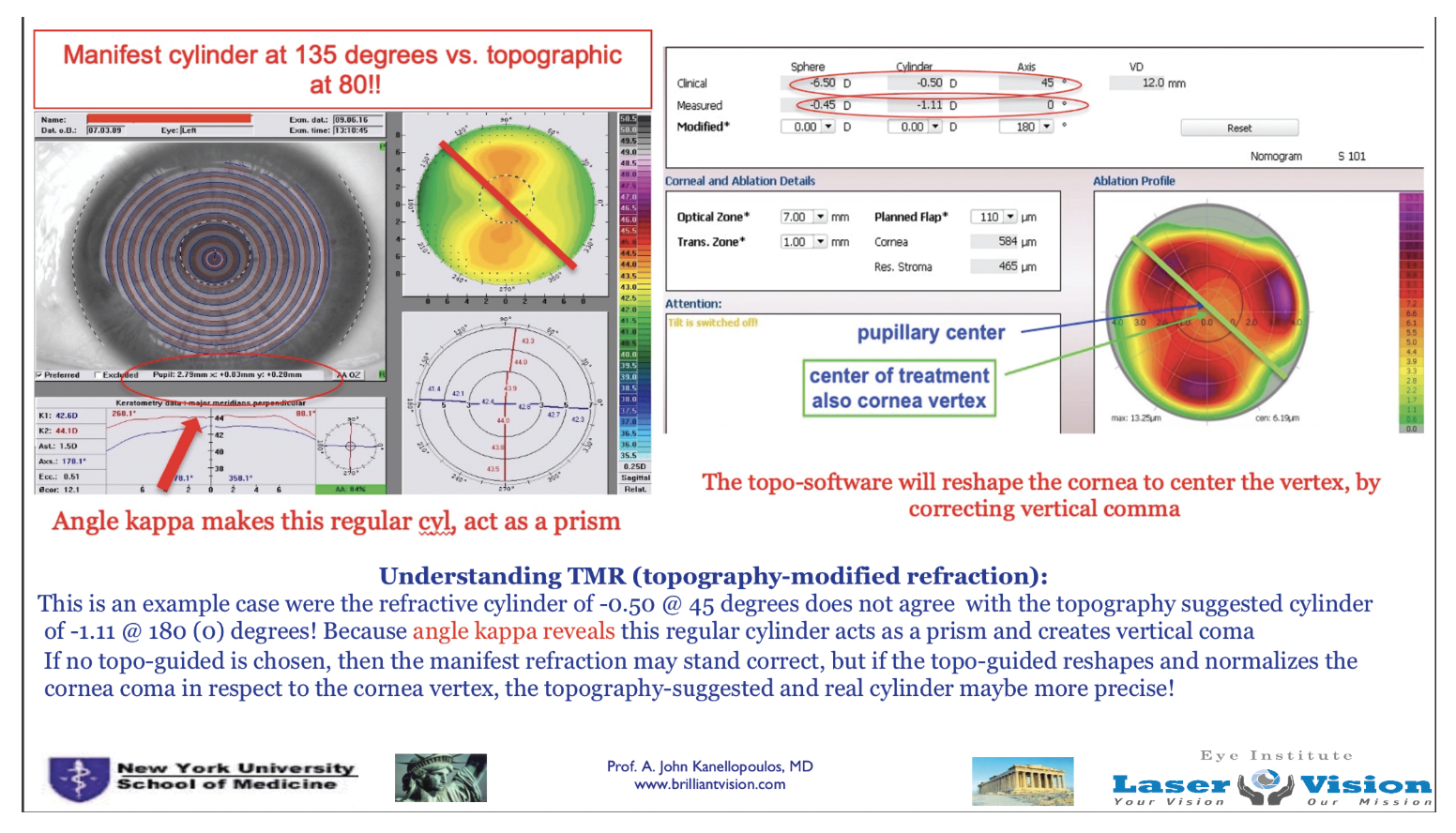 |
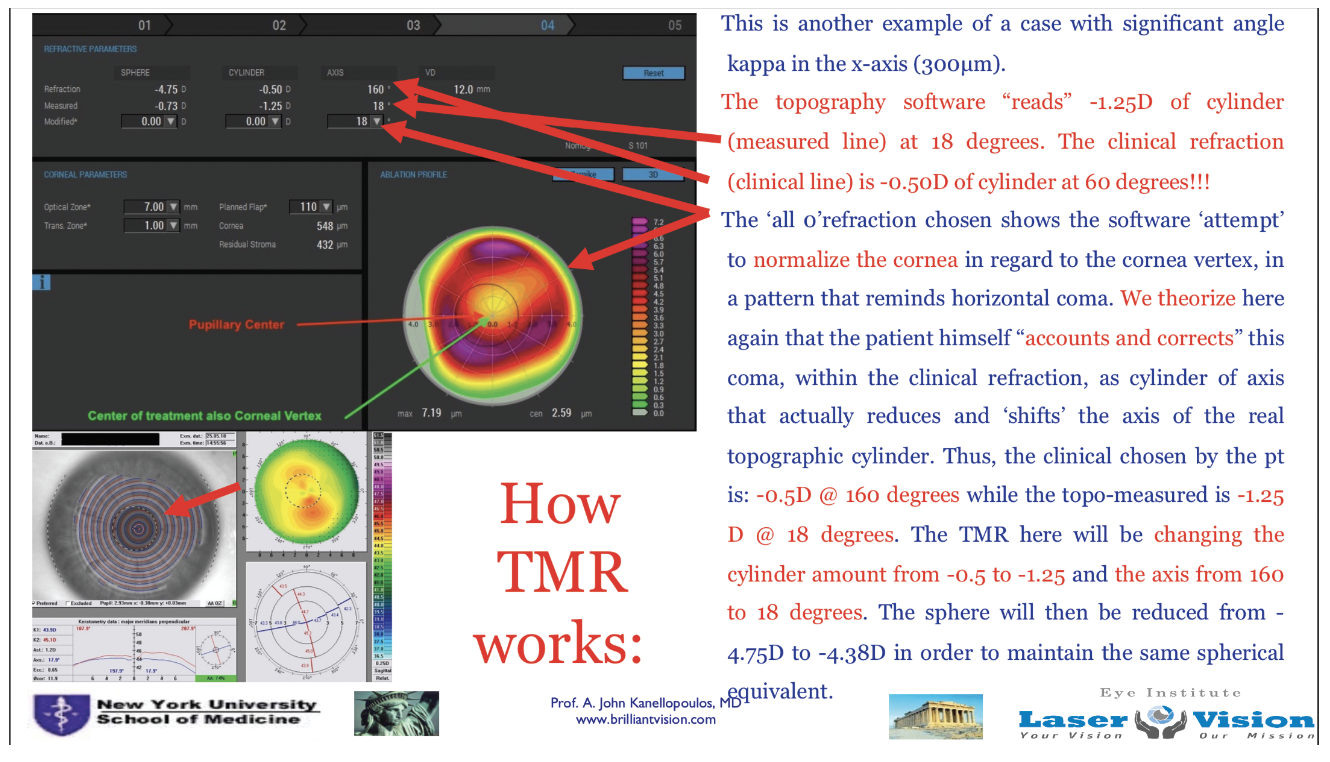
| An explanation of how angle kappa in a naive myopic astigmatic eye can be addressed with topo-guided LASIK that will normalize the otherwise-considered normal corneal astigmatism in regard to the cornea vertex (visual axis). |
Dr. Lobanoff developed a software platform—Phorcides—which is modeled off of geographic imaging software used by cartographers. The software creates vectors for any raised topographic feature, as well as for anterior and posterior corneal astigmatism and internal lenticular astigmatism, and an algorithm presents the best treatment. A retrospective analysis7 (which Dr. Lobanoff co-authored), compared outcomes of eyes treated using the manifest refraction vs. those treated with an ablation profile suggested by Phorcides. In the latter group, significantly more eyes had 20/16 or better UDVA (62.5 percent compared to 41.3 percent). Alcon now recommends using Phorcides (which is free to surgeons) on its Contoura platform.
Some surgeons may have been left with a bad taste in their mouth after the initial Contoura rollout, continues Dr. Lobanoff. “I’d tell them to take a second look. Have an open mind,” he says. “Just like technology improves every year, this has improved dramatically since the early days. And it’s faster, easier and far more accurate than when they may have tried it the first time.”
Dr. Maloney says much has advanced in wavefront technology, too, since he began using it in the clinical trials over 20 years ago. “We first had the WaveScan system and the iDesign 1, and now we’re on the iDesign 2 system, which is a really superb wavefront analyzer,” he says. “It measures more than 1,000 points. It’s very easy to capture and much of the planning is done automatically, so it makes wavefront treatments easy to do. We’ve seen huge improvements there.”
 |
| Research conducted by A. John Kanellopoulos, MD, suggests using topography-modified refraction as opposed to the subjective manifest refraction to achieve best outcomes. |
On- and Off-label Candidate Screening Tips
There are certain criteria to keep in mind for customized LASIK treatments, say experts. Both topo-guided and wavefront-guided/topo-integrated are approved for normal corneas; however, they can also be used off-label to treat certain irregular corneas.
“Wavefront is approved for treating low, moderate and high degrees of myopia and astigmatism,” says George O. Waring IV, MD, FACS, who practices in South Carolina and uses the iDesign. “The laser also performs very well for mixed astigmatism and select cases of hyperopia and hyperopic astigmatism or compound hyperopic astigmatism, however, more and more we’re treating hyperopia with intraocular lens-based solutions.”
He agrees this technology can be very powerful in an abnormal cornea, to an extent. “There are varying philosophies on this,” says Dr. Waring. “Some have had excellent experience using this technology in abnormal corneas. An advantage of the high-definition wavefront is that it allows you to more reliably capture irregular corneas. In our experience we tend to defer the treatment to the manifest in the irregular cornea and often are focused more on treating the lower-order aberration if it can improve their uncorrected visual acuity. That’s our typical practice pattern, even with the standard treatment focused on the lower-order aberrations in the irregular cornea. We do feel that although there’s emerging work that’s very promising in therapeutic topography-guided treatments for highly aberrated corneas, there’s also promising work using the wavefront-guided system for these as well. These are difficult cases that are often multi-step and require careful informed consent and multiple visits.”
Dr. Lobanoff says image capture is important before proceeding. “You have to capture a quality topography image (on Contoura) with the Vario Topolyzer, a device from Alcon,” he says. “Some patients have really high brows or sometimes patients have really deep-set eyes or something prevents you from getting a good topography image. Well, if you don’t have a good topography image, you can’t treat topographically. The Contoura is only FDA approved for myopia and myopia with astigmatism, so patients who are hyperopic or have really high myopia above a -9, you can’t use Contoura. Otherwise, I feel every patient benefits from this. Every patient in our clinic who’s a potential candidate gets this.”
But going back to its roots, continues Dr. Lobanoff, Contoura was first used in Europe for repair procedures. “This is off-label here because in the FDA study they only treated perfect eyes,” he says. “But it’s really powerful for treating patients who maybe had LASIK in the early days where tracking systems weren’t available or microkeratomes left scars or small ablation zones. We can fix a lot of these patients who had complaints from the early days of LASIK and can make them better.”
The biggest tip is to start with normal, regular virgin eyes. “First, understand the technology, get used to the results and how you work patients up and then, once you gain confidence with it, start tackling more challenging cases,” Dr.
Lobanoff says.
“The iDesign 2.0 has a full-gradient topographer that captures over 1,200 x and y slopes, as well as a wavefront aberrometer, so the individual patient’s topographic data is used to vertex wavefront-guided data from the pupil to the corneal plane; it also takes into account cosine compensation,” says Dr. Waring. “This is high-definition wavefront-guided—not topographically guided—but it’s topographically registering the high-definition wavefront, so that gives an extraordinary amount of precision for whole-eye optics that it accounts for, which can treat subtle irregularities, such as coma, in ways that can be difficult to do or can’t be done with other technologies.”
Pearls for Using the Technology
These experts shared their pearls and caveats for these customized procedures.
• Accounting for accommodation. Dr. Waring most often hears instances of surgeons with early over-corrections due to not accounting for accommodation. “The technology has internal mechanisms and accommodative fixation targets that account for this, but even then the technicians need to make sure that the ocular surface is pristine and well-lubricated,” Dr. Waring notes. “Number two, that they have the appropriate pupil size and correct registration landmarks, and number three, that the patient understands how to look through the fixation targets to account for accommodation. They can also minimize accommodation by having patients count backwards from 100 in their head, as well as minimize the use of accommodative effort around the time of perioperative planning, for example, minimizing cell phone use in the waiting room, and also minimizing wait-time altogether. We are meticulous about our wavefront captures.”
He continues, “The iDesign 2.0 also generates qualitative metrics in terms of the validity of the scans, and makes recommendations on the highest fidelity of captures as well. All of these matter in your screening process and it’s all part of our training with our technicians.”
• Nomograms. For this reason above, a good nomogram is necessary. “It’s important with the wavefront-guided system to use a nomogram because the current system tends to overcorrect slightly so you need a nomogram to reduce the overcorrection,” says Dr. Maloney.
“For a wavefront-guided myopic astigmatism [with the iDesign] for example, we cut back on our spherical ablation a set amount, which is a normal process in a physician adjustment that’s derived from your outcomes,” says Dr. Waring. “This is important when you onboard any laser but it’s particularly important with the iDesign to account not only for the differences in each laser, but also to account for mild overtreatments that are multifactorial in etiology, including accommodation during the wavefront capture and also the ablative characteristics of a custom wavefront-guided excimer treatment.”
• Topography-modified refraction. Manifest refraction has long been the norm for laser vision correction, but the introduction of topo-guided technology has demonstrated the ways in which measured refraction can influence outcomes for the better. As published by Dr. Kanellopoulos, topography-modified refraction8 is an adjustment of the amount and axis of astigmatism treated, suggesting that it preemptively bypasses the lenticular astigmatism bias in young myopic eyes and may compensate for some amount of corneal astigmatism and corneal coma generated by angle kappa, therefore leading to superior outcomes in topo-guided myopic LASIK, as stated in the study.
• Cyclorotation. “The EX500 excimer laser, which is a descendent of the original 400 IQ excimer laser, has shown the ability of adjusting for the inevitable cyclorotation of all eyes,” Dr. Kanellopoulos says. “When the patient goes from standing to supine, the eyes rotate towards the nose, so the right eye rotates clockwise the left eye rotates counter-clockwise for a miniscule number of degrees, but sometimes it could be as high as 9 degrees. Thus, correcting astigmatism, especially in topo-guided treatments, becomes very essential to be adjusted for that eventual cyclorotation.”
• Epithelial mapping. Dr. Kanellopoulos says he has long argued the values of documenting the naive state of the virgin cornea for any customized treatment. “For close to 15 years now, as a prerequisite, we’ve used epithelial mapping to establish that,” he says. “If epithelial mapping shows irregularity, we’d avoid using customized data that rely on cornea imaging because this would transfer the noise of the measurement on to the customized treatment. Also, if there’s a significant deviation of the manifest refraction cylinder amount and axis from that suggested by the topography, confirmation from tomography needs to take place because the perceived curvature of the cornea may not actually be an average of -6 and may interfere with what the refraction topography is measuring. Thus, in any case where the surgeon decides to employ our popularized topo-modified refraction (mentioned above) in their topo-guided treatments, confirmation of the amount of and axis cylinder by tomography needs to take place.”
What the Future Holds
Even with the excellent outcomes published across multiple studies, customized LASIK with topo-guided technology hasn’t seen the uptake one would expect. Dr. Lobanoff avers that some surgeons might just be comfortable with the results they’re already getting with normal wavefront-guided excimer lasers, which have seen advancements of their own. “When you’ve got something that’s giving you good results, and you’ve done it for 20 years and you feel comfortable with it, it’s hard to get out of your comfort zone,” he says.
“I think the real benefit of the technology is the power of the diagnostic and the outcomes that can be realized,” says Dr. Waring. “There’s been a positive adoption rate for topography-guided treatments, however, many users don’t routinely use the topographic treatment aspects of the technology, largely due to the requirement for the additional time and effort for diagnostic workup for both the patients and the staff. However, the outcomes are excellent. All have their nuances and considerations and therapeutic laser refractive surgery is an art and a science that not only requires the right technology, but also the right approach and still represents a very relatively small amount of the market of refractive surgery in the United States. This is an emerging area of interest and research to help many patients in need.”
Competition in the refractive surgery arena is only going to get tighter as newer technologies are introduced. Dr. Kanellopoulos believes ray-tracing will be the next frontier in customized LASIK, but says it remains to be seen if it will be adopted globally.
Dr. Maloney is excited about the possibilities. “I think LASIK will continue to improve incrementally with the new laser systems, and I expect we’ll get a better version of SMILE,” he says. “We’ll have new IOL designs coming that will make refractive lens exchange even better. So, I think, while refractive volume is down lately because of the presumed recession, I’m extraordinarily optimistic about the future. My vision is that someday I’ll be in a museum with my grandchild and he’ll tug on my pant leg and point to an object, ‘What’s that, Grandpa?’ And I’ll say, ‘Those are eyeglasses.”
Dr. Lobanoff is a consultant for Alcon and the CEO and owner of Phorcides. Dr. Kanellopoulos is a consultant for Alcon. Dr. Maloney is a consultant for Johnson & Johnson Vision and holds equity in RXSight. Dr. Waring is a consultant for Johnson & Johnson Vision.
1. Alcon introduces Contoura Vision as first personalized LASIK procedure at American Academy of Ophthalmology Annual Meeting. Nov. 16, 2015. https://www.alcon.com/media-release/alcon-introduces-contoura-vision-first-personalized-lasik-procedure-american-academy. Accessed Nov. 20, 2023.
2. FDA Clinical Trials. Allegretto Wave Eye-Q Addendum Procedure Manual T-CAT Topography-Guided Treatments. http://www.accessdata.fda.gov/cdrh_docs/pdf2/P020050S012d.pdf. Accessed Nov. 20, 2023.
3. Johnson & Johnson Vision Launches Next Generation of Personalized LASIK Treatment, iDESIGN Refractive Studio Now Available. Sept., 6, 2018. https://www.jjvision.com/press-release/johnson-johnson-vision-launches-next-generation-personalized-lasik-treatment-idesign. Accessed Nov. 20, 2023.
4. Shetty R, Matalia H, Nandini C, et al. Wavefront-guided LASIK has comparable ocular and corneal aberrometric outcomes but better visual acuity outcomes than SMILE in myopic eyes. J Refract Surg 2018;34:8:527-532.
5. FDA Clinical Trials. Topography-Assisted Lasik Treatment For Nearsightedness (Myopia) With Astigmatism, Nidek EC-5000 Excimer Laser System. https://www.accessdata.fda.gov/cdrh_docs/pdf/P970053S011d.pdf. Accessed Nov. 20, 2023.
6. Cheng SM, Tu RX, Li X, Zhang JS, Tian Z, Zha ZW, Ruan KW, Yu AY. Topography-guided versus wavefront-optimized LASIK for myopia with and without astigmatism: A meta-analysis. J Refract Surg 2021;37:10:707-714.
7. Lobanoff M, Stonecipher K, Tooma T, Wexler S, Potvin R. Clinical outcomes after topography-guided LASIK: Comparing results based on a new topography analysis algorithm with those based on manifest refraction. J Cataract Refract Surg 2020;46:6:814-819.
8. Kanellopoulos AJ. Topography-modified refraction (TMR): Adjustment of treated cylinder amount and axis to the topography versus standard clinical refraction in myopic topography-guided LASIK. Clin Ophthalmol 2016;3:10:2213-2221.