Surgeons today have a number of corneal refractive procedures to offer and customize to patients’ needs or specific anatomic considerations. But, as surgeons know, more options also mean many more factors to consider when it comes to patient selection, from corneal measurements and co-existing pathology to lifestyle and personality.
Here, experts share how they select patients for LASIK, SMILE and PRK, and the key inclusion and exclusion criteria that help narrow down the options.
Assessing the Cornea
Candidacy for a corneal refractive procedure begins with a thorough screening to ensure that the patient isn’t at risk for ectasia, which can develop as a result of corneal biomechanical failure or external factors such as eye rubbing or laser vision correction itself. Beeran Meghpara, MD, co-director of the refractive surgery department at Wills Eye Hospital in Philadelphia, says the gold standard for ectasia screening is Placido-based corneal topography, which helps to identify subtle areas of inferior steepening, but a host of other complementary modalities is also key.
“Nowadays, we go beyond topography and employ tomography (Pentacam) as well to look for elevation changes in the anterior and the posterior cornea,” he explains. “Probably the newest modality we use is OCT epithelial mapping of the cornea, looking for areas of focal thinning. The corneal epithelium is remarkably uniform across the entirety of a patient’s cornea and among patients in the general population. Very small changes in epithelial thickness are risk factors for, or potential early signs of, keratoconus. These changes may show up earlier on epithelial mapping than on some other imaging modalities, so all of my patients undergo evaluation with all three.”
“The pachymetry, topography and manifest refraction are the three main factors I consider when screening patients, though there are many others to consider,” says John Odette, MD, in practice at Austin Eye in Texas. “When I’m trying to decide whether a patient is a good candidate for a procedure, I start by ruling out patients who have significant corneal risk factors, such as a cornea with irregular topography, a prescription that’s too high, and of course, a cornea that’s too thin.”
Kathryn M. Hatch, MD, director of the refractive surgery service and site director of Massachusetts Eye and Ear in Waltham carefully evaluates several factors when screening patients for laser vision correction. “On corneal topography and tomography, anterior and posterior corneal shape as well as the central corneal thickness are critical when screening patients,” she says. “Additionally, it’s important to assess for higher order aberrations and consider doing epithelial thickness mapping. “On Pentacam, I check for elevation changes and assess D-score, on the Belin/Ambrosio Enhanced Ectasia Display for keratoconus, which combines nine different keratometric indices and assigns a risk factor for keratoconus. It’s usually white when it’s normal, yellow when somewhat abnormal and red when clearly abnormal with an extremely high probability of keratoconus. Usually, if the number is less than 1.6, it’s safe; however, sometimes the D-score is white but one of the indices is red, and it might still look abnormal. You can’t base your decision solely off this score, of course. It’s important to look at the indices and the map itself for anything concerning on tomography.”
Enough Tissue?
Surgeons must consider the degree of impact that a certain laser procedure would have on the cornea. As in years past, many say they would avoid performing such surgery in patients who have corneas thinner than 500 µm preoperatively.
“LASIK involves the most corneal manipulation of the three procedures since a flap is created in addition to tissue removal,” says Dr. Meghpara. “With PRK, no flap is created, so less cornea is affected and treated. With more residual cornea, the biomechanical strength of the cornea is potentially greater compared with LASIK. However, creating this epithelial defect has its associated downsides, such as pain in the immediate postoperative period, a very low risk of haze and a longer healing time. SMILE’s impact on the cornea is somewhere between the two. The incision is smaller than in LASIK, and no epithelial defect is created. SMILE usually creates less discomfort than LASIK and more rapid visual recovery than PRK.”
There’s ongoing debate about the best way to measure residual cornea, says Dr. Odette. Some surgeons go by residual stromal bed thickness while others go by the percentage of corneal tissue altered; many consider both. “I tend to lean toward residual stromal bed thickness, where potential candidates will have at least 300 µm,” he says.
Dr. Meghpara agrees. “Everyone has their own cut off as far as what the residual stromal bed thickness should be,” he says. “The traditional number in the literature is 250 µm, but many surgeons including me are more conservative and like to have at least 300 µm of residual stromal bed thickness.
“With PRK and SMILE, this amount is whatever amount of stroma is left over,” he explains. “With LASIK, we have to take into account the flap thickness as well as how much stroma is removed as a result of the treatment because the flap no longer contributes to the biomechanical strength of the cornea afterwards.”
The percentage of tissue altered is a ratio of the amount of cornea altered (flap thickness plus ablation depth) divided by the total preoperative central corneal thickness. “If it’s greater than 40 percent,” Dr. Meghpara says, “then the procedure will increase the risk of ectasia. Generally, a patient with a PTA greater than 40 percent is a poor candidate for any of the treatments.”
Selecting a Procedure
After corneal testing comes the question: What would you do in this patient? “Most patients who come into the clinic for a refractive surgery consultation are probably candidates for multiple procedures and would do fine with a number of them,” says Dr. Meghpara. “Trying to explain the different options and which one is best for their lifestyle and recovery goals is the challenge. It’s a lot easier if a patient would clearly do better with one option compared with another.”
Experts say that LASIK is often the go-to procedure due do its safety and excellent visual outcomes. The treatment is approved for up to -12 D of myopia, up to +6 D of hyperopia and up to 6 D of astigmatism in patients over the age of 18. Many surgeons, however, prefer to wait until patients are in their mid-20s after their prescription has stabilized.
“LASIK has an amazing track record with very good results,” Dr. Meghpara says. “In fact, among the general public, LASIK has become synonymous with any sort of laser vision correction procedure. Even if a patient didn’t have LASIK—maybe they had SMILE or PRK—they’ll probably still tell their friends that they had LASIK. If someone’s a good candidate for LASIK, that’s generally the direction we’ll go in.”
“The vast majority of the time, 20- to 40-year-olds are great candidates for LASIK,” Dr. Odette says. “Low to moderate myopes tend to be the best population, even if they have some mixed astigmatism. High myopes and hyperopes tend not to do as well with keratorefractive procedures, on the other hand.”
“When a patient comes for a refractive surgery evaluation and they fit all the parameters of LASIK, we really don’t have a conversation about other procedures because LASIK is typically the safest and most predictable procedure with the fastest healing,” says Steven M. Silverstein, MD, an assistant professor of ophthalmology at the University of Missouri Kansas City Medical School and in practice at Silverstein Eye Centers in Kansas City.
 |
| An ink mark placed at the LASIK flap edge helps to ensure good flap realignment. (Courtesy Uday Devgan, MD) |
Lifestyle Factors
Of course, LASIK isn’t suitable for every patient. In addition to a too-thin cornea, certain lifestyle factors may rule out the option of LASIK due to concerns about flap complications. In these cases, PRK is often preferred. The procedure is approved to treat between -1 and -12 D of myopia, with up to 4 D of astigmatism, and between +1 and +6 D of hyperopia, with up to 4 D of astigmatism in patients over age 18.
“I consider work and recreational activities to be two of the most important aspects to ask patients about because that’s where people spend the majority of their day,” says Dr. Odette. “Activities such as contact sports, boxing and mixed martial arts, and certain careers such as construction, are risk factors for flap dislocation. If a patient has a high risk of being poked in the eye, a flap procedure might not be the best option.”
Dr. Meghpara agrees, adding that professional athletes, police officers and individuals in the military are also unlikely to be suitable LASIK candidates for this reason. “We steer these individuals away from LASIK because of concerns that such activities could dislocate the flap,” he says. “PRK or SMILE may be better options.”
Recovery and Safety
“Choosing a refractive procedure for a patient requires a comprehensive approach,” Dr. Hatch says. “I go through an algorithm in my head each time, taking into account many different aspects, from personality and lifestyle to ocular anatomy.
“I like to think about LASIK and SMILE as one group and PRK in its own category from a healing perspective,” continues Dr. Hatch, who has been offering SMILE since its FDA approval. “Recovery is an important aspect of surgery to consider, and patients also really like the idea of a smaller incision. So, if a patient is a candidate for all three techniques, I usually offer SMILE as a first choice and always double consent for LASIK as well, so that in the rare situation that we can’t complete SMILE, we can convert to LASIK. I also use similar criteria for SMILE as for LASIK. The patient must be a good candidate for LASIK in order to offer them SMILE.
“I don’t believe SMILE is replacing LASIK or excimer lasers,” she adds. “I view it as an additive procedure that will help grow refractive surgery in general and allow surgeons to offer comprehensive refractive surgery procedures to patients.”
“LASIK has the quickest recovery time, so if a rapid recovery is important to the patient, and they’re a candidate, then LASIK may be the best option,” Dr. Meghpara says. “SMILE is next, and PRK has probably the slowest healing or visual rehabilitation time, but relatively speaking, it’s probably the safest of the three procedures. We have to assess where the patient falls on the scale of convenience versus safety. All three surgeries are very safe, but if we want to stack the deck in favor of safety, then PRK may be the best choice.”
“When safety is a principal factor, as far as not creating ectasia, then PRK and sometimes SMILE may be the only options,” Dr. Silverstein says. “That being said, patients generally prefer to heal and return to activities of daily living as quickly as possible, which is why LASIK remains the most popular refractive procedure we offer.”
SMILE’s treatment indications were expanded a few years ago to allow correction up to -10 D of myopia and up to 3 D of astigmatism for patients 22 and older. Dr. Silverstein says, “The SMILE procedure is equally beneficial for people with mild to moderate nearsightedness and mild to moderate astigmatism but there’s typically less opportunity or availability to access that particular machine or laser, with the excimer laser used for LASIK and PRK being much more widely available.”
“For the most part, anyone who’d be a good candidate for PRK would be a good candidate for SMILE,” Dr. Meghpara says. “The reason I would choose to go with SMILE is that the vision recovers more quickly and there’s less postoperative discomfort. That being said, SMILE isn’t some magic procedure that can be done on everybody. If someone isn’t a good candidate for PRK, then they really shouldn’t be a candidate for SMILE either.”
Managing Expectations
Educating patients to ensure they have realistic goals is an important part of the refractive surgery journey. Dr. Hatch says that “sometimes managing patient expectations and setting them appropriately is the most difficult part.”
“Usually, after we get testing done, and after speaking with the patient, I can make a very good recommendation,” Dr. Odette says. “But once in a while, patients disagree and want something else done, so we have a discussion to figure out why they might want a procedure that may not be the best fit for them, and then figure out whether we could actually do that procedure safely.
“For particular type-A personalities,” Dr. Odette adds, “you need to have a little caution because sometimes these patients won’t like an outcome despite its being quite good.”
“Personality is a significant factor,” says Dr. Silverstein. “We have a very careful conversation and a sign-off by the patient about realistic expectations, including the potential need for glasses for certain activities, especially reading and night driving in the presbyopic demographic. The patient has to know that they may still require glasses when driving in inclement weather, for example, even after a successful corneal-based refractive procedure. If their expectations can’t be appropriately maintained, they may not be a candidate for any refractive procedure.”
Ensuring older patients understand these visual compromises can be difficult, experts say. “This is a conversation that I have even with patients in their late 30s and early 40s who may need reading glasses within the next five years,” says Dr. Hatch. “Many times, patients will say they don’t need readers, or they already wear contacts, but won’t realize their contacts have a little bit of mini monovision. I find that once we actually put the prescription into the patient’s eyes, it most certainly increases the need for readers. Even when we tell patients again and again, it’s still hard for them to grasp because right now, they don’t need readers. It’s important for them to understand the progressive nature of presbyopia. It’s not a conversation you can hurry.”
Considerations and Contraindications
As with any surgical procedure, it’s important to ensure the risks don’t outweigh the benefits. Potential candidacy for LASIK, PRK and SMILE can be narrowed down beyond corneal parameters, lifestyle and age when medical and medication history—both ocular and systemic—are taken into consideration.
Here are some situations that raise a few red flags:
• Progressive corneal thinning. If a patient has any degree of keratoconus or pellucid marginal degeneration, they’re not a candidate for corneal refractive surgery.
“A patient with forme fruste keratoconus may still proceed with careful discussion and if their vision easily corrects to 20/20 preoperatively,” Dr. Silverstein says. “You can still successfully achieve full correction in mild to moderate refractive cases with minimal risk of surgically induced ectasia. In forme fruste keratoconus, SMILE may be the best option for corneal stability postoperatively. Of course, a lens-based procedure would mitigate the risk of corneal ectasia in these patients, as would an ICL.”
He adds, “In a patient with topography demonstrating against-the-rule astigmatism in a sagging mustache pattern, I’d recommend against all corneal refractive procedures.”
Some surgeons have tried adding simultaneous cross-linking to corneal refractive surgery in order to reduce the risk of iatrogenic ectasia. A review of the current literature on simultaneous accelerated crosslinking reported that this treatment is effective for myopia but it’s still unclear whether the additional crosslinking step reduces ectasia incidence.1
Dr. Silverstein says he doesn’t perform corneal cross-linking on these patients before a procedure. “First of all, the results of cross-linking aren’t predictable enough, and the long-term effects of cross-linking, as it pertains to refractive procedures and keratoconus isn’t known. I’ve successfully performed LASIK or PRK in forme fruste keratoconic patients many times without the development of ectasia over the last 25 years.”
• Dry eye. Dry eye can occur after any corneal refractive surgery, but it may be more severe if the patient has preexisting dry eye. Of the three corneal refractive procedures, LASIK carries the greatest risk for postoperative dry eye, with reported incidences of 94.8 percent, 85.4 percent and 59.4 percent of patients experiencing symptoms at one day, one week and one month, respectively.2
“Severe dry eye is a marked contraindication, and probably our second biggest worry after ectasia,” says Dr. Odette.
“Patients with poorly controlled dry eye shouldn’t undergo any sort of laser vision correction or corneal refractive surgery unless they receive good, aggressive treatment for it,” agrees Dr. Meghpara. “For patients with a little bit of dry eye or mild dry eye that’s well controlled, we’d potentially avoid LASIK, as SMILE or PRK might be a better option for them.”
Surgeons say that it’s important to wait for the ocular surface to stabilize before performing a procedure. “I’ll treat lid margin disease and ocular surface disease aggressively for six weeks and then reevaluate,” Dr. Silverstein says. “We want to get good, accurate measurements and keratometry before proceeding.”
• Epithelial basement membrane dystrophy. EBMD affects the anterior cornea and may cause recurrent corneal erosions and lead to decreased vision. LASIK can worsen the condition.
Dr. Hatch says it’s important to perform a careful slit lamp evaluation to rule out EBMD. “This condition often has a subtle presentation and requires careful examination in every patient,” she explains. “I always check the cornea with fluorescein to assess for the negative staining pattern in addition to assessing the tear film.”
“In patients with EBMD, I typically recommend PRK,” she says. “EBMD can be easily missed and also cause problems preoperatively, intraoperatively and postoperatively, so we need to be very good observers of the epithelium.”
• Stromal neovascularization. Corneal neovascularization is a common complication of keratitis and occurs in a number of other pathologies, often leading to decreased visual acuity. “Caution should be used in patients with deep stromal neovascularization, especially when it involves more than one quadrant of vessels,” Dr. Silverstein says.
• Significant corneal scarring. “Patients with significant scarring involving the central visual axis who don’t correct to 20/20 may not be good candidates for refractive procedures,” says Dr. Silverstein. “Other poor candidates may include those with significant interior stromal scarring from EBMD or those with significant Salzmann’s dystrophy. If the visual axis is uninvolved, which is usually not the case in these two situations, SMILE may be an option.”
• Corneal guttata. “If a patient has stable, mild to moderate dystrophy with one to two or more corneal guttae, they could undergo successful LASIK, PRK or SMILE,” Dr. Silverstein says. “However, patients with three or more guttae with any element of endothelial pathology or corneal swelling shouldn’t have a corneal-based procedure.”
• Prior radial keratotomy or LASIK. “If a patient has had RK, I lean toward PRK because I don’t like to make a flap into RK incisions,” Dr. Odette says. “I know many doctors who’ve successfully made flaps into old RK incisions, so I know it can be done, but it’s not my favorite approach. Doing PRK over an old LASIK flap can be problematic as well, with epithelial hyperplasia. There’s no perfect answer on what to do with prior LASIK—do you lift the flap and risk epithelial ingrowth, or do you do PRK over the top? Neither is perfect, unfortunately.”
• Prior corneal graft. Dr. Odette says he prefers not to perform corneal refractive procedures over corneal grafts. “I have done a couple PRKs over corneal grafts, but it’s very rare. There’s a risk for graft rejection, so I really lean away from that and don’t recommend it.”
• Retinal disease. Dr. Silverstein says it’s important to perform a fully dilated posterior segment exam when screening patients for refractive surgery. “If a patient has significant macular disease, such as macular scarring or soft fluid drusen from macular degeneration, significant diabetic retinopathy or history of vascular occlusive disease (beyond a mild branch retinal vein occlusion in the past, greater than six months prior with a return to 20/20 vision), these patients should be counseled against refractive procedures, not because of safety concerns but because they’ll achieve a less than desired visual outcome.”
• Glaucoma. Refractive surgery poses some risks for glaucomatous eyes. During LASIK flap creation, the elevated eye pressure may damage the optic nerve. Additionally, postoperative steroid use, especially after PRK, runs the risk of a patient developing steroid-induced glaucoma. Experts say that SMILE or PRK may be safer for glaucomatous eyes since no flap is involved. Refractive surgery that thins the cornea may also lead to underestimation of IOP on Goldmann applanation tonometry.
• Pregnancy and lactation. “Pregnancy and nursing are contraindications for refractive surgery because the patient’s prescription or refraction changes postoperatively,” Dr. Meghpara says.
These changes in the eye’s refractive index are thought to be caused by hormonal changes that cause fluid retention in the cornea3 or by an increase in lens curvature that leads to a myopic shift.4 “Patients should wait at least six months from when they delivered their child and three months after they stop nursing to undergo a procedure,” he says.
• Systemic diseases. Autoimmune conditions are often listed among the considerations or contraindications for corneal refractive surgery because their immunosuppressive treatments may hinder the body’s healing responses. Examples include Sjogren’s syndrome, type-1 diabetes, systemic lupus erythematosus and rheumatoid arthritis.
“I’d be very hesitant to perform a corneal procedure on a patient being treated for rheumatoid arthritis,” Dr. Silverstein says. “Not necessarily a diagnosis of rheumatoid arthritis but being treated systemically for it would be a contraindication.
“Patients who are on systemic treatment for thyroid eye disease need to be consulted about the significance of dry eye caused by LASIK,” he adds. “Having abnormal anatomy, where the cornea isn’t properly covered and protected, would exclude a patient from corneal refractive procedures.”
“Some surgeons consider many autoimmune diseases as red flags or contraindications,” Dr. Odette says. “I consider them mild contraindications because many patients with autoimmune diseases are asymptomatic and do quite well with refractive surgery, though I know that that’s debated.”
“If a patient with an autoimmune condition is well controlled and their dry eye is similarly well controlled, I might avoid LASIK and do SMILE or PRK instead,” Dr. Hatch says. “These procedures may have less drying potential and risk for dry eye.”
Non-LVC Candidates
Patients who aren’t candidates for corneal refractive surgery still have options. In addition to intraocular lenses, experts say implantable collamer lenses or a refractive lens exchange are options:
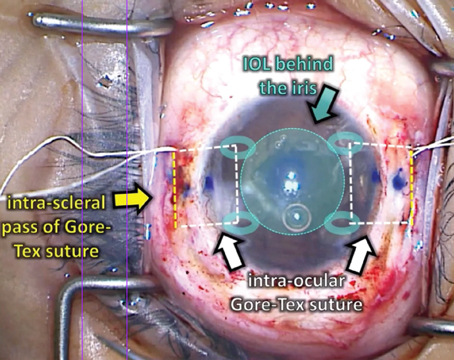
• Implantable collamer lenses. The EVO ICL (Staar) is an artificial lens made of collagen and plastic that’s suitable for patients with moderate to high myopia under the age of 50 who don’t have cataracts. The lens is implanted between the natural crystalline lens and the iris. Experts say ICLs may be good options for patients with more severe dry-eye disease.
“Now that we have the EVO ICL, we have more options for patients who have corneal pathology or who may not be the best laser vision correction candidate,” Dr. Hatch says. “It’s a one-step procedure with no need to perform peripheral iridotomies.”
Dr. Silverman says, “An ICL may be the best option for patients who have significant nearsightedness (greater than 6 D) with mild to moderate astigmatism, and for whom a corneal-based procedure isn’t appropriate—perhaps due to corneal pathology such as Salzmann’s nodules, which can recur even after removal.”
• Refractive lens exchange. Experts say that depending on the patient’s age and anatomic considerations, a refractive lens exchange with or without femtosecond laser assistance may be a good long-term option.
Dr. Silverstein explains, “For patients in their 50s or older who are presbyopic with mild or greater cataract, this option offers the potential for multifocal lenses that give more range of vision or the Light Adjustable Lens, which can be adjusted after implantation and appropriate corneal healing in order to achieve high postoperative accuracy and predictability in the final refractive outcome.”
“Now that we have such advanced IOL technologies, I think it’s even more important that we approach the patient with a comprehensive refractive mentality,” Dr. Hatch says. “When we see patients 50 and older, for example, with moderately high amounts of refractive error including hyperopia, myopia and astigmatism, we should talk to them about refractive lens exchange. Patients should know there are many different options for treating their presbyopia in addition to their other refractive errors.
“When I have patients come in who are in their 50s—even if they’re not interested in a refractive lens exchange and don’t have signs of lens changes yet—I still always ask questions about their vision when they drive at night or in inclement weather,” she continues. “I ask whether it’s challenging and whether they’ve noticed any increased difficulty. These are very early indicators that some lens-based changes are happening. I tell these patients, ‘If we do laser vision correction on you, this won’t improve. In fact, your vision may stay the same or get worse.’
“This can be a determining factor for those with early lens changes,” she says. “We may want to advise patients to wait until their cataract develops more. Or, if the patient is really excited or ambitious about having their vision corrected, then doing a refractive lens exchange in older patients may be the best way to go.”
Dr. Hatch says she doesn’t generally consider performing a refractive lens exchange in a patient under 50. “Patients who are in their forties still have accommodation and attached vitreous, so I tend to wait until they’re a bit older,” she explains. “That said, I do think we have to approach patients from a comprehensive mentality and explain all the possible options, even those that might open up down the road, and even if you don’t offer refractive lens exchange. We also need to make sure they understand the implications of having had prior laser vision correction at the time of cataract surgery. The impact the laser has on their cornea can affect what implant technology we might be able to offer them at the time of cataract surgery due to the shape change of the cornea. Keratometry shape, as we know, is so critical in the IOL selection.
Dr. Meghpara is a consult for Zeiss and Johnson & Johnson Vision. Dr. Hatch is a consultant for Alcon, Zeiss and Johnson & Johnson Vision. Drs. Silverstein and Odette have no related financial disclosures.
1. Lim EW and Lim L. Review of laser vision correction (LASIK, PRK and SMILE) with simultaneous accelerated corneal crosslinking—Long-term results. Curr Eye Res 2019;44:11:1171-1180.
2. Sharma B, Soni D, Saxena H, et al. Impact of corneal refractive surgery on the precorneal tear film. Indian J Ophthalmol 2020;68:12:2804-2812.
3. Ebeigbe JA, Ebeigbe PN, Ighoroje AD. Ocular changes in pregnant Nigerian women. Nigerian J Clin Pract 2011;15:298-301.
4. Yenerel NM and Küçümen RB. Pregnancy and the eye. Turk J Ophthalmol 2015;45:5:213-219.