 |
This month, the e-mailed survey was opened by 992 of 7,605 subscribers to Review’s e-mail service (13 percent open rate); of those, 57 shared their responses.
To get a sense of where you stand in the IOL landscape, read on.
Monofocal Lenses
These are the lenses that surgeons say they use for most of their cases. When choosing them, they look for things like ease of use, consistency and a reliable lens material.
Fifty-four percent of the surgeons say they use the Alcon IQ Aspheric IOL for most of their cases, while 31 percent prefer the J&J Vision Tecnis one-piece lens. Six percent use the B+L enVista, 4 percent like the B+L SofPort AO, 2 percent prefer the B+L Akreos AO and 2 percent like the Hoya iSymm/iSert.
“I like that the Alcon IQ unfolds slowly,” says Connecticut surgeon Kevin Dinowitz. “Acrylic is less likely to cause inflammation or interfere with silicone oil retinal procedures. It gives consistently excellent outcomes.”
“The lens is very quiet in the eye,” avers an AcrySof IQ surgeon from Nevada. “Glistening and reflections are a little bothersome to patients.” A California surgeon also uses the Alcon lens for most of his surgeries, saying, “Cons: yellow color; glistening. Pro: It’s very easy to insert.”
On the Tecnis side, Bruce Cohen, MD, of St. Louis says he prefers it because it “works well, has no glistenings, is easy to load and inject and has great optics.” Lee Yasgur, MD, of Cherry Hill/Voorhees, New Jersey, agrees, saying, “The Tecnis offers ease-of-insertion, and it’s pre-loaded to avoid twists, kinks and minimize hand motion: KISS [Keep It Simple, Stupid].” Rishi Kumar, MD, of Louisville, Kentucky, says he likes the Tecnis best because it’s “pre-loaded, clear, one-piece and has no vacuoles.”
“The Bausch + Lomb enVista uses a high-quality optic and has no glistenings,” argues another surgeon. A surgeon from Ohio prefers the B+L SofPort AO partly due to its versatility: “It’s aspheric, compatible with use in the sulcus, with minimal dysphotopsia,” he says. “It allows me to order one lens, as it is also my sulcus backup.”
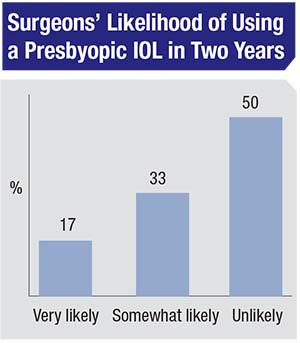
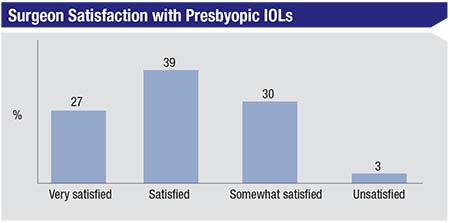
Presbyopic Lenses
Surgeons also discussed the presbyopic lenses they use, how many they implant per month
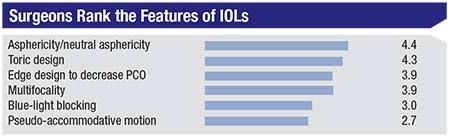 |
| Surgeons on the survey ranked IOL features in terms of their usefulness using a numerical scale that ran from 1 (least useful) to 6 (most useful). The average scores are shown. |
The option chosen by most surgeons was the Symfony, at 23 percent (average number implanted per month: 2.7; average charge: $2,262). The AcrySof aspheric ReSTOR 2.5 D was next, at 22 percent (average number implanted: 2.6; average charge: $2,505). The third most popular option was the AcrySof aspheric ReSTOR 3 D, at 8 percent (average number implanted: 3.2; average charge: $2,607). The rest of the field broke down as follows:
• AcrySof ReSTOR Toric 2.5: 6 percent (avg. no. implanted: 2; avg. charge: $2,769);
• Tecnis 2.75 D Multifocal: 5 percent (avg. no. implanted: 2.75; avg. charge: $1,899);
• Tecnis 3.25 D Multifocal: 5 percent (avg. no. implanted: 4; avg. charge: $2,300);
• AcrySof ReSTOR Toric 3 D: 5 percent (avg. no. implanted: 2; avg. charge: $2,761); and
• Crystalens AO: 3 percent (avg. no. implanted: 2.7; avg. charge: $2,167).
Surgeons shared the reasons they like certain presbyopic lenses, as well as what areas could use some improvement.
Louisville’s Dr. Kumar explains why he likes the Symfony: “It has fewer halos,” he says, “and you don’t have to be so exact with the refractive outcome. However, refraction adjustment after surgery like that used by the light-adjustable IOL would be great.” Ron Glassman, MD, of Teaneck, New Jersey, agrees up to a point. “It has less glare than older multifocals,” he says, “but not zero.” A surgeon from California says he likes the Symfony, but is a bit disappointed in its near vision. “Make a higher-add component, if feasible,” he says.
Baltimore surgeon Ismail Shalaby uses the Alcon Aspheric ReSTOR 2.5 a lot, commenting, “Results are good with the Alcon lens, and the toric platform is excellent with minimal or no rotation. Patients haven’t reported nighttime issues.” Dr. Dinowitz often uses the Aspheric ReSTOR 2.5, but says there’s always room for improvement. “There’s still a learning curve involved,” he says, “and needing the perfect candidate limits the number of candidates. The need to implant both eyes to even know how it will work is a risk.” Cherry Hill’s Dr. Yasgur says that, in his experience, “Any minus correction left in the the Symfony causes spiderweb haloes, and all Alcon lenses cause ‘diamond-eye’ light reflexes that patients’ family members do not like to look at.” Jonathan Adler, MD, of Bradenton, Florida, who says he often uses the Alcon Aspheric ReSTOR 3 D, shares his lens wish list: “A lens that
 |
Toric Lenses
Fifty-eight percent of surgeons say they regularly use toric lenses, and shared their views on these lenses’ pros and cons.
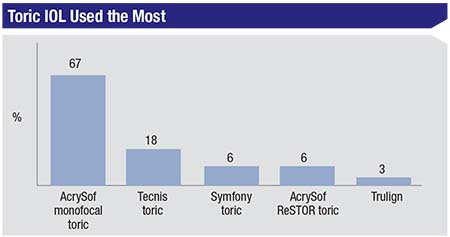
In terms of the toric IOL the surgeons say they use the most, 67 percent say they use the AcrySof monofocal toric. Eighteen
 |
“The [AcrySof monofocal toric] is easy to implant and rotate, but the translucent markings are difficult to visualize and align in larger myopic eyes,” says Dr. Dinowitz. “You can’t focus the cornea and the markings at the same time in the larger myopic eyes and have to focus on one plane.” A New York surgeon likes using the AcrySof monofocal toric, saying, “I like the stability and refractive predictability.” He adds, however, “Its maker could improve the ease of insertion at the proper axis.” A surgeon from Michigan says he likes the “larger range of options for astigmatism,” offered by the AcrySof toric, but says it could use “improvement in prevention of lens rotation.”
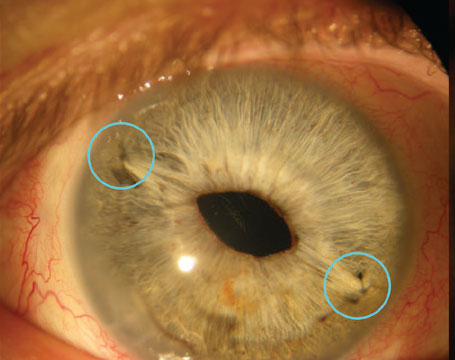
Lens Complications
Unfortunately, lens implantations don’t always go as smoothly as hoped, so surgeons also shared their thoughts on suturing and explanting IOLs.
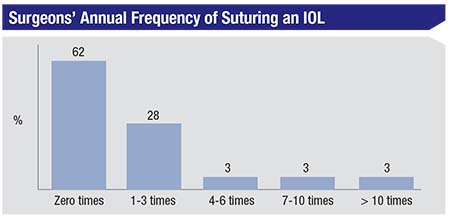
Most respondents (62 percent) say they don’t find themselves suturing an IOL in order to properly fixate it; 28 percent say they have to suture-fixate a lens 1-3 times throughout the year; and 3 percent each say they have to suture a lens 4-6 times, 7-10, or more than 10 times in a year.
Surgeons explained why this suture fixation was necessary. “Dislocation/decentration of the IOL within the capsular bag,” says a surgeon from Utah. “Also, poor zonular/capsular support. I use a ciliary sulcus suture.” An ophthalmologist from Virginia says the reason is often “lack of good capsule or iris support,” and that he usually uses a pars plana suture. One surgeon, who says he sutures IOLs more than 10 times a year, says the most common reason is “subluxation after years of
 |
In terms of explantations, surgeons’ reasons for doing it in the past 12 months vary. Steven Stiles, MD, of Tarzana, California, says he explanted a lens because the “lens power was way off.” Baltimore’s Dr. Shalaby explants lenses due to “nyctalopia in the older multifocal IOLs.” Dr. Dinowitz had to take a lens out because the patient was a challenging case, citing “the wrong IOL power in a keratoconus patient.” In 2017, Dr. Yasgur had to explant a lens 15 years after it was first implanted, the culprit being “subluxation due to pseudoexfoliation.” Dr. Cohen says he explanted lenses on two occasions. “One was for the wrong power in an extended-depth-of-focus lens, and the other was a multifocal case in which the patient didn’t tolerate glare.”
Other reasons that respondents provided for explants on this year’s survey include: uveitis; multifocal issues; instability; dysphotopsias; glare/halo and positive photopsias; and patient dissatisfaction with a multifocal or EDOF lens. REVIEW