For years, surgeons have been casting about for an intraocular lens solution that would give their patients a wider range of vision. The latest technology approved in the United States aimed at this goal is trifocal lenses and, according to our current e-survey of cataract surgeons, it’s intrigued physicians to the point at which a good number of them say they’re either using them currently, or are willing to give them a try in 2021. Whether this interest will endure or is just a function of the immediate “bounce” a new technology gets simply by being new, only time will tell.
This is just one of the findings from this year’s e-mail survey on IOL preferences. This time around, 9 percent of the 12,258 recipients on Review’s e-mail list opened the message, and 75 surgeons took the survey. To read about your colleagues’ impressions of trifocal IOLs, as well as other lens technologies, read on.
Presbyopia-correcting Lenses
As mentioned earlier, surgeons are on the lookout for new options for presbyopic lenses.
The most popular option on the survey, with 67 percent of the surgeons choosing it, is the Alcon PanOptix Trifocal (non-toric) (average number implanted per month: 2; average charge/eye: $ 2,790). The PanOptix Trifocal Toric was next, at 59 percent (average number/month: 4.7; average charge: $3,347). The Tecnis Symfony extended-depth-of-focus IOL and the Symfony Toric were next, each chosen by 30 percent of the respondents (average number implanted/month: 6.6; average charge/eye: $2,594). The Tecnis MF +3.25 D (2.8 lenses implanted per month with an average charge of $2,500) was next, chosen by 18 percent of the surgeons. Ten percent of respondents say they use the Crystalens AO (average number/month: 2; average charge/eye: $2,798).
Forty-five percent of the surgeons say they’re “satisfied” with their presyopia-correcting lens, 38 percent say they’re “very” satisfied, 12 percent are somewhat satisfied and 6 percent are unsatisfied.
One surgeon who uses the PanOptix says, “The optics are the best available but it still has undesirable side effects.” A surgeon from Alabama says the PanOptix gives “Good spectacle independence with minimal patient complaints/dissatisfaction.” A California surgeon says the lens affords him, “Excellent range of vision, distance, intermediate, near…Very happy patients. It still has some nighttime halo issues like all multifocals.”
“The PanOptix is providing good vision at all distances,” says a surgeon from North Carolina. “But [to improve it] I [would] decrease glare.” A surgeon from Missouri feels similarly, saying, “The lens’s rings sometimes give glare.” A Rhode Island surgeon also says there’s some room for improvement. “My current [PanOptix] patients get good uncorrected distance and near vision,” he says. “But it could be improved by changing material, e.g., Clareon.”
“[PanOptix] gives good overall good range of vision up to 18 inches,” says a surgeon from Michigan. “I would like fewer halos.”
Another surgeon says he “still can’t predict perfectly which patients may be unhappy with glare/halos.”
For the surgeons who currently use the Symfony for most of their premium, presbyopia-correcting IOL cases, they say they’re satisfied with the results, for the most part.
“Excellent quality of vision is maintained, and rings and halos are minimal,” says one surgeon. “The lens is tolerant of residual refractive error and, with proper patient education and selection, these are very happy patients.” One surgeon from Texas says he has “no issue with IOL material, glistenings, etc.” Ron Glassman, MD, Teaneck, New Jersey, says the Symfony yields “few dysphotopsias, but weak reading.” A surgeon from Washington agrees, saying, “It could use improvement in very-small-print near vision.”
Hazard, Kentucky, ophthalmologist Syam Reddy primarily uses the Symfony, but says, “Not all the patients are happy. Sometimes I do not get the ‘Wow’ response.”
 |
In the Crystalens camp, a surgeon from Colorado says, “The lens doesn’t accommodate 3 D, but it’s the best overall for optical quality and contrast.”
To try to optimize their results with presbyopia-correcting IOLs, 24 percent of the respondents say they “mix and match” lenses (i.e., they use a different lens in each eye of the patient in an effort to have one lens make up for the shortcomings of the other).
“I’ll mix the toric version with the non-toric version—but both are the same platform,” says Abram Geisendorfer, MD, of Quincy, Illinois.
William Lipsky, MD, of Houston, says, “I most often [combine] the ZKB00 and ZLB00, sometimes with a ZXR00. Now that the toric versions are available, it might be ZLB00 with ZCB00 or a ZXT.”
A surgeon from Iowa is thinking along the same lines when he says, “[I combine] the Tecnis Symfony and Tecnis MF +3.25 D. These lenses balance each other’s strengths/weaknesses well.”
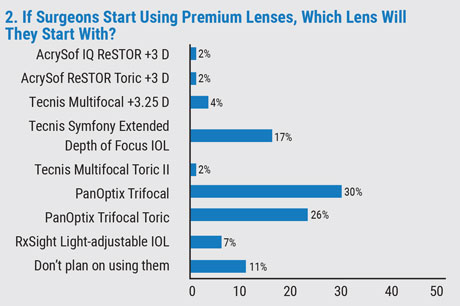
Looking down the road, as alluded to earlier, a good size portion of the respondents who don’t currently implant premium lenses say the lens they’re interested in trying is the PanOptix (30 percent) or PanOptix Toric (26 percent). Seventeen percent of the surgeons say they’d try the Symfony and 6 percent will give the RxSight light-adjustable IOL a try. Eleven percent of surgeons, however, don’t plan on using presbyopia-correcting lenses.
One surgeon from California says she’s thinking of giving the PanOptix a try. “It supposedly gives good vision at intermediate and near,” she says.
“The PanOptix gives the best range of vision plus toric correction,” says Jonathan Macy, Los Angeles, laying out the reasons he would give the lens a try.
Teaneck’s Dr. Glassman is eyeing the Symfony. “It stays clear, and [poses] the least risk,” he says. One surgeon says he’s considering implanting the Tecnis multifocal 3.25 D because it seems to have “few long-term issues.”
Eschewing today’s technology, some surgeons are looking ahead to the approvals of lenses currently in development. “Indeed [I’d use] a Synergy IOL [Johnson & Johnson Vision],” says one surgeon. Another physician simply says he’ll use “The Vivity [Alcon].”
One surgeon from California, though, representing the 6 percent who don’t want anything to do with presbyopia-correcting IOLs, says, “[With presbyopia-correcting IOLs] there are too many patients who are unhappy after paying a lot of money.”
Bread-and-Butter: Monofocals
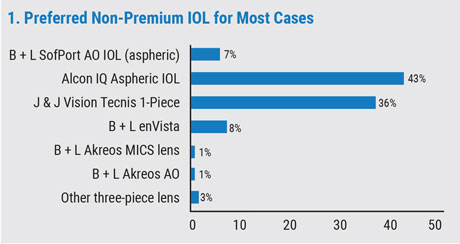
Though premium IOLs are an intriguing wrinkle in IOL design to discuss and speculate about, the lenses surgeons use for most of their cases are monofocal IOLs.
This year, the two most popular monofocal lens choices on the survey are the Alcon IQ Aspheric (43 percent) and the Johnson & Johnson Vision Tecnis 1-piece (36 percent). The Bausch + Lomb enVista was next, chosen by 8 percent of surgeons.
 |
“I like the long-term success, stability and visual results [of the IQ Aspheric],” says St. Louis’ Richard Wieder, MD. “I dislike [the] mild issues with glistenings.” A surgeon from Michigan says he likes “the yellow tint, stability, asphericity and controlled unfolding…. I don’t like the lack of a pre-loaded version.”
“I like the better visualization around the edge of the optic if the patient needs subsequent pars plana vitrectomy,” says a surgeon from South Carolina. A surgeon from Washington adds that, “I like how it slowly opens in the eye giving me time for perfect positioning.”
A surgeon from Texas says he prefers the Tecnis 1-piece for its “ease of use, no glistenings, predictable results, excellent quality of vision and minimal dysphotopsias in my experience—‘20/Happy’ patients!” Regarding the Tecnis, another surgeon says, “Like: super clear optics. Don’t like: aberrations; sticky haptics (i.e., haptics stick to the IOL and routinely need manipulation to deploy).”
Toric IOLs
 |
Surgeons have more options for alleviating patients’ astigmatism than ever before. Here are their current favorite modalities:
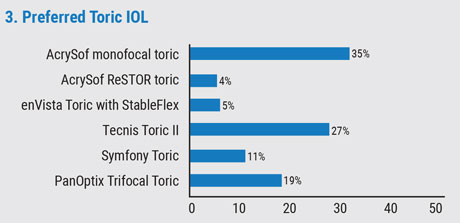
In the study, 35 percent of the surgeons prefer the AcrySof monofocal toric. Next is the new Tecnis Toric II, at 27 percent. The PanOptix Trifocal Toric is the preferred toric IOL for 19 percent of the respondents, and the Symfony Toric was chosen by 11 percent. The rest of the results appear in graph 3.
A Michigan surgeon who uses the AcrySof monofocal toric says, “This toric IOL using the ORA [intraoperative aberrometry] is very predictable in my hands.”
“The Tecnis Toric II works well, with almost no rotation, gives great results and very predictable outcomes,” says a surgeon from Texas.
A surgeon from Florida literally has a love/hate relationship with the AcrySof monofocal toric. “I hate glistenings,” he says, “but I love the lens stability.”
Phakic IOLs
Only 16 percent of the surgeons on our survey say they implant phakic IOLs, and all of them use the Staar Visian ICL (available in both toric and non-toric versions). Though they appreciate the benefits the lenses bring to select patients, they say there’s room for improvement, as well.
“When they work, they’re very good,” says Dr. Lipsky. “But I can’t wait for the improved version with fenestrations to eliminate PIs.” Another surgeon says, “They’re a great choice for patients who can’t opt for corneal refractive surgery.” Atlanta’s Trevor Woodhams, MD, sees both the advantages and limitations of the devices, saying, “It’s a good technology, but too expensive for patients. They’re excellent for high myopes and ‘funny’ corneas. They’re still too difficult to size prospectively, however.”
Managing Problems
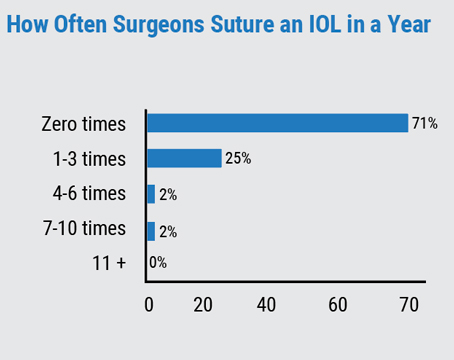
Surgeons also weighed in on the nature and frequency of dislocated IOLs that require suturing.
Over the span of a year, 63 percent of the respondents say they never have to suture an IOL, 29 percent say they have to suture one to three lenses, 5 percent suture four to six and 3 percent suture seven to 10.
One surgeon says the main reason for suturing is often “previous surgery leaving questionable capsular/zonular integrity,” and he sutures the lens either to the iris or the sclera with intrascleral haptic fixation. A surgeon from Virginia says, “I only suture an existing, dislocated lens, usually to iris.” Dr. Lipsky uses the Yamane technique. “[The suture location is the] iris, mostly for dislocated IOLs,” he says. “I use the Yamane technique without a suture most often.” REVIEW