To the Editor:
In the July 2018 Review article “The IOL In the Sulcus: When, Why & How,” a suggestion was made that placing a single-piece acrylic IOL with haptics in the sulcus in an optic capture configuration (lens optic captured posteriorly through an intact capsulorhexis with haptics positioned in the sulcus) may be an acceptable option. As surgeons that frequently deal with complications of cataract surgery on referral we all have seen serious complications arise from single-piece acrylic IOL haptics that have been placed in the sulcus. These issues include iris chafing, pigment dispersion, chronic inflammation, cystoid macular edema, glaucoma and, ultimately, loss of vision. We all agree that efforts should be made to avoid placing the haptics of a single-piece acrylic intraocular lens in the sulcus, and that to do so intentionally places patients at unnecessary risk that could be avoided with use of an appropriate three-piece lens (or a lens designed for sulcus placement). The haptics of single-piece hydrophobic acrylic lenses should be positioned behind the anterior capsule rim to prevent a high risk of complications.
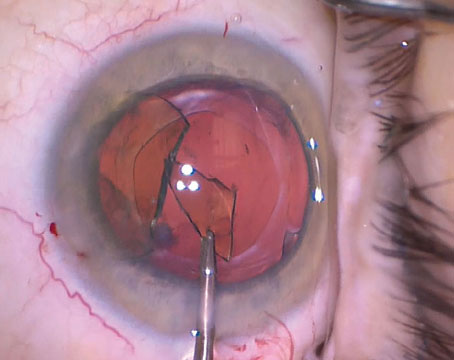
In the article, the optic capture configuration suggested by Dr. Grayson, with the lens optic prolapsed behind the intact anterior capsule rim and the haptics in the sulcus, may help to stabilize the lens against dislocation, but the lens haptics remain in the sulcus where they may contact the iris pigment epithelium and cause problems. In models of optic capture performed by one of this letter’s authors (Dr. Ouano), prolapsing the optic posteriorly behind the anterior capsule pushes the lens haptics to a more anterior position where they might inflict even more damage. When posterior capsule support is lacking, if the haptics don’t remain in the sulcus the entire singlepiece lens may dislocate into the vitreous. We ask surgeons to consider having an appropriate backup lens option available in cases where there may be risk of damage to the posterior capsule and loss of the option of in-the-bag placement for a scheduled single-piece acrylic lens. Optic capture of such lenses with the haptics in the sulcus isn’t an acceptable option.
Signed,
Steven Safran, MD, Dean Ouano, MD, Sadeer Hannush, MD, Mark Gorovoy, MD, Jason Jones, MD, Michael Snyder, MD, Thomas Oetting, MD, and Greg Ogawa, MD
References:
Chang DF, Masket S, Miller KM, et al; ASCRS Cataract Clinical Committee. Complications of sulcus placement of single-piece acrylic intraocular lenses: Recommendations for backup IOL implantation following posterior capsule rupture. J Cataract Refract Surg 2009;35:8:1445-58.
Uy HS, Chan PS. Pigment release and secondary glaucoma after implantation of single-piece acrylic intraocular lenses in the ciliary sulcus. Am J Ophthalmol 2006;142:2:330-2.
LeBoyer RM, Werner L, Snyder ME, et al. Acute haptic-induced ciliary sulcus irritation associated with single-piece AcrySof intraocular lenses. J Cataract Refract Surg 2005;31:7:1421-7. Hong Y, Sun YX, Qi H, Zhou JC, Hao YS. Pigment dispersion glaucoma induced by the chafing effect of intraocular lens haptics in Asian eyes. Curr Eye Res 2013;38:3:358-62.
Mohebbi M, Bashiri SA, Mohammadi SF, et al. Outcome of singlepiece intraocular lens sulcus implantation following posterior capsular rupture during phacoemulsification. J Ophthalmic Vis Res 2017;12:3:275-280.
Micheli T, Cheung LM, Sharma S, et al. Acute haptic-induced pigmentary glaucoma with an AcrySof intraocular lens. J Cataract Refract Surg 2002;28:10:1869-72.
Vasavada AR, Raj SM, Karve S, et al. Retrospective ultrasound biomicroscopic analysis of single-piece sulcus-fixated acrylic intraocular lenses. J Cataract Refract Surg 2010;36:5:771-7.
Dr. Grayson responds:
I agree completely that sulcus placement of a one-piece acrylic IOL without anterior capsulotomy capture should never be performed, for all the reasons discussed in the article and then reiterated in the letter. I also agree that sulcus placement with onepiece IOL capture in a capsulotomy that’s irregular, decentered or larger than 5 mm should never be performed. Also, one-piece sulcus placement with IOL capture in short axial length eyes with decreased chamber depth and limited clearance between the posterior iris and the anterior capsule shelf shouldn’t be performed.
Sulcus placement of a one-piece acrylic with anterior capsulotomy capture can be performed in eyes with a longer axial length and a clinically evident deep anterior capsular shelf with respect to the posterior iris surface. There must also be a well-centered capsulotomy less than 5 mm, optimally created by a femtosecond laser. Most important, there should be a clinical consideration about the approach that would afford the patient the best visual rehabilitation outcome. I absolutely don’t advocate routinely placing onepiece acrylics in the sulcus as a backup when in-the-bag placement isn’t possible.
I’ve successfully implanted two Symfony IOLs in the sulcus with IOL capture. Both were myopes with deep chambers and adequate distance between the posterior iris and the anterior capsule. Both were second-eye surgeries. One was a Symfony toric. From the clinical perspective, using a three-piece Tecnis in this second eye surgery wouldn’t give the patient the best multifocal result, since the optical design of the Symfony is very different from the Tecnis. Blending different add power Tecnis IOLs in the same patient can work well, though, and is common since the optical design of the lenses are similar. In the toric Symfony patient, placing a spherical Tecnis three-piece ZMB00 would result in a different multifocal visual experience in addition to a lack of clarity from residual astigmatism. Corneal astigmatic cuts had been already placed by a femtolaser, but only for the residual astigmatism not fully corrected by the toric IOL. These cuts could be augmented, but would leave visually significant uncorrected astigmatism. If monofocal three-piece IOLs were used, the visual systems could be potentially disrupted by having one Symfony eye and one monofocal eye, especially when neuroadapting to any night-vision issues.
I realize that two patients isn’t a large enough series to advocate a change in practice. My discussion was simply to point out that given certain clinical circumstances and surgical situations, one-piece acrylic IOLs can be placed in the sulcus with anterior capsule capture. With more than one year of follow-up, both patients have done well, with excellent vision and none of the complications described.
Signed,
Douglas Grayson, MD