Dry eye affects millions of patients, and clinicians need to understand the signs and symptoms of the disease in order to help mitigate dry eye’s effects. Dry eye is difficult to define, which leads clinicians to categorize the disease as mild, moderate and severe for most cases. But there’s always underlying factors that go unrecognized which lead to ineffective treatment options for dry eye. “The key to dry-eye treatment is early identification, early intervention and prevention as much as possible,” says Christopher Starr, MD, an ophthalmologist at Weill Cornell Medicine in New York and a global ambassador for the Tear Film and Ocular Surface Society.
This article will examine various treatment options to help clinicians manage DED after identifying all signs and symptoms.
The Roots of Dry Eye
“Dry eye is an umbrella term. It includes different symptoms and signs all of which can be driven by various contributors,” says Anat Galor, MD, MSPH, an ophthalmologist at the University of Miami Health System in Florida.
The eye is affected everyday by many factors contributing to dry eye, which make it more difficult to define DED.
Initially, dry eye was defined as a disorder, instead of a disease, that lead to tear deficiency and tear evaporation, but this definition failed to describe any specific pathophysiologic basis.1 In the TFOS DEWS report, society members defined dry eye as a disease for the first time, but many clinicians interpreted this definition as primarily diagnostic criteria.1 The current TFOS definition for DED was described in the DEWS II report. It states that “Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.”1
“There has to be a balance of all the key components of the ocular surface, the tear film and various mechanisms, from sensation and corneal nerves to the brain with the trigeminal and the lacrimal functional unit of all the lacrimal glands and the accessory lacrimal glands, to the meibomian glands and the goblet cells,” says Dr. Starr. “All of these things need to be in tight homeostasis regulation.”
 |
At-Home Treatments
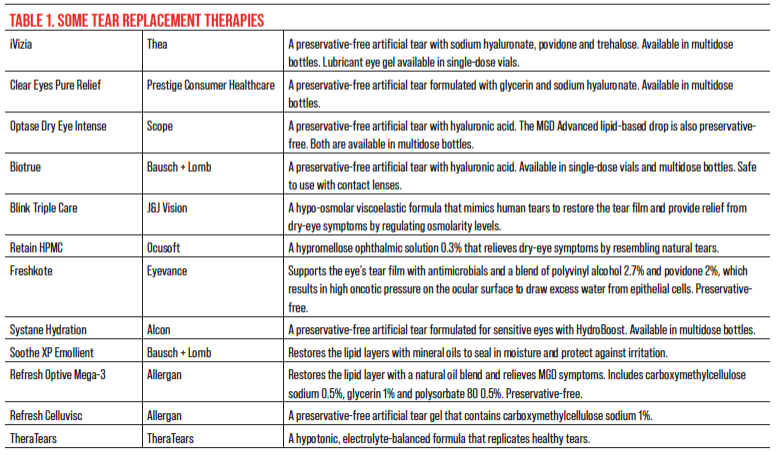
“No matter what’s causing symptoms, there are a few things individuals can do on their own before they seek care,” continues Dr. Galor. “These include buying tear supplements, marketed under the term artificial tears, that have various viscosities and different compounds.”
Over recent years, many preservative-free eye drops began making their way on the market. Each eye drop is a unique solution with different properties to help treat various symptoms of DED. “I don’t think there’s a right artificial tear supplement; it’s more what works for an individual person, finding the right composition and viscosity that improves symptoms and doesn’t blur vision,” says Dr. Galor. “The more viscous the artificial tear, the more likely it is to blur vision temporarily. We try to steer people away from preservatives like BAK that can have adverse effects on nerves and epithelial cells, but there are lots of great products out there for people to try.”
While artificial tears are useful, they aren’t always the best solution for all cases. “If a patient is having to use these eye drops eight times a day or more, they’d better switch to a gel form or ointment,” says Esen Akpek, MD, an ophthalmologist at Johns Hopkins Sjögren’s Center in Maryland. “We have the impression that instilling too many eye drops could be harmful to the ocular surface by washing the mucin and oil components of the tear film.”
Other ways to treat mild dry-eye cases include home remedies that are simple for patients to include in their daily regimen. “Warming up the eyelids is a tried-and-true over-the-counter maintenance therapy, and there are many ways of doing that from run-of-the-mill washcloths under warm water to microwaving potatoes and putting them in socks to tea bags,” says Dr. Starr. “There are more sophisticated methods. For instance, the Bruder company has something call the Bruder Moist Heat Eye Compress, which is a reusable, microwavable mask.”
“Another thing people can do on their own is recognize that symptoms and signs of dry eye can be driven by environmental contributors, so it’s important to consider the environment around you,” says Dr. Galor. “Optimizing temperature and humidity, maintaining a clean environment as much as you can by changing your air filter, addressing sources of mold and installing an air purifier are all ways to improve your indoor environment.”
One environment that many patients neglect to recognize as a contributing factor is the office space. Strenuous activity in front of a screen for a long period of time eventually leads to DED complications. “Being on the computer for 12 hours a day affects your blink rate, which can affect your tear metrics,” says Dr. Galor. “People talk about the 20/20/20 rule: Set a timer, stand up, and blink a few times. Take breaks and consider the work environment. For example, installing a humidifier if your work area is arid may help your eyes feel better.” The 20/20/20 rule suggests that patients suffering from DED should set a timer for 20 minutes during computer use. Then, after the timer goes off, they should stand for 20 seconds staring and blinking at an object 20 feet away. This helps reduce screen time and encourages an increase in blink rate.
 |
| Click image to enlarge. |
Antibiotics and Anti-Inflammatories
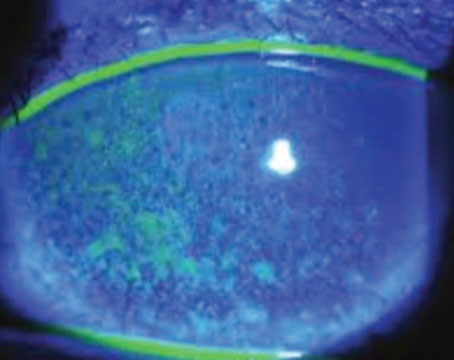
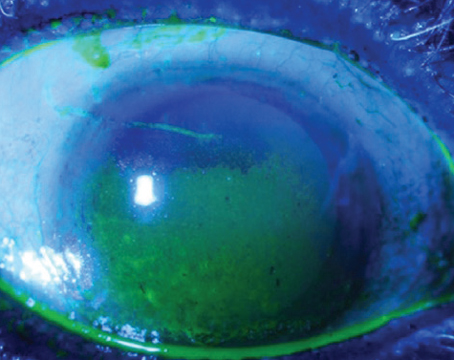
“If a patient has physician-measured clinical signs consistent with dry eye, such as decreased tear production as measured with Schirmer’s, ocular surface damage, evidenced by lissamine green or fluorescein staining, or increased osmolarity, then I definitely go on to the next step, which is prescription eye drops,” says Dr. Akpek. “It’s important to choose the eye drop according to the clinical finding. We need to differentiate aqueous-deficient from evaporative dry eye.”
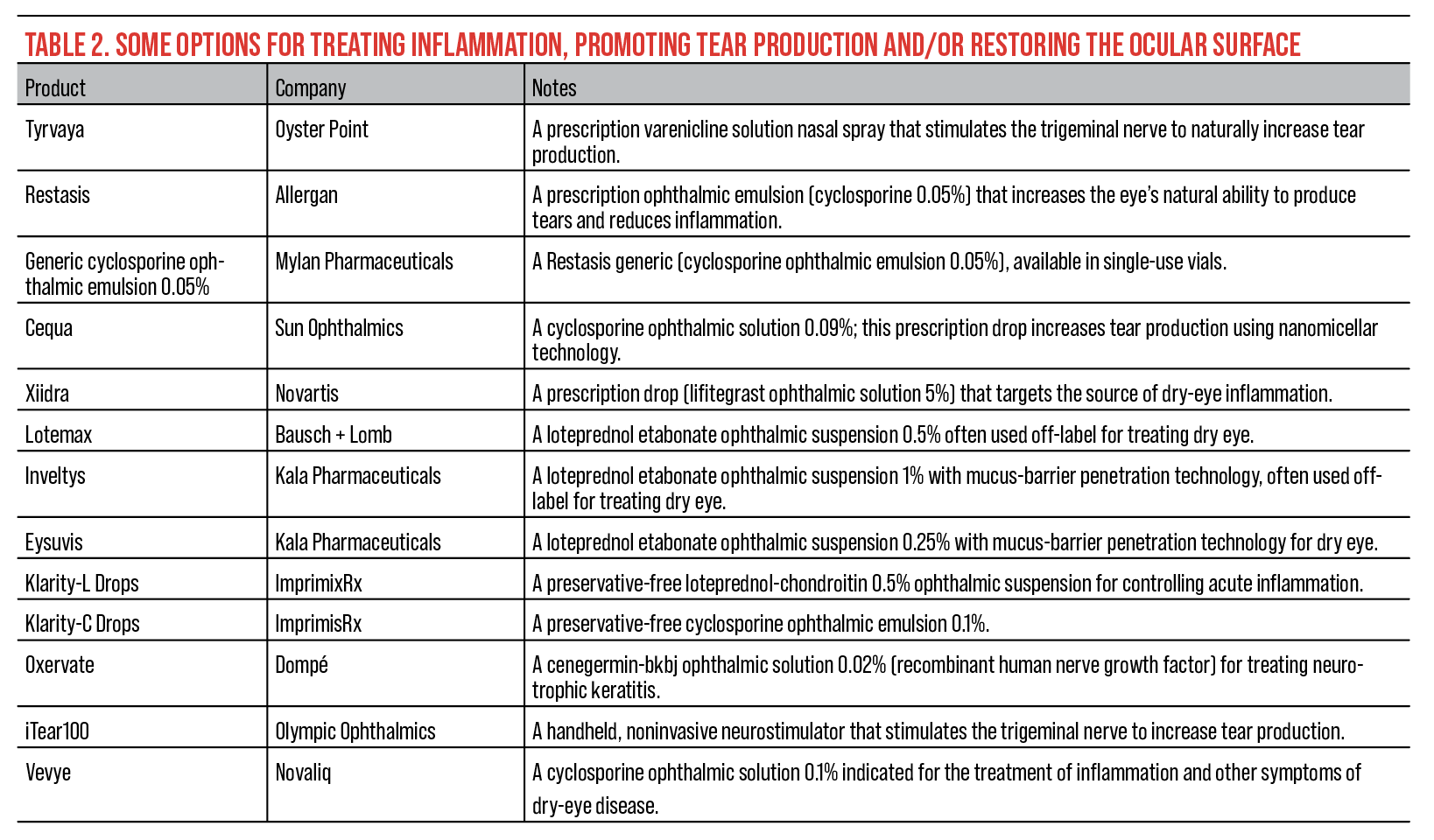
In the past, corticosteroids have been used off-label to treat inflammation in dry-eye patients. “I have a very low threshold for steroid use for inflamed eyes,” says Dr. Starr. “There’s now an FDA approved steroid for dry-eye disease flairs, Eysuvis.”
Eysuvis (loteprednol etabonate 0.25%, Kala Pharmaceuticals), Lotemax (loteprednol etabonate 0.5%, Bausch + Lomb) and Flarex FML (fluorometholone acetate 0.1%, Eyevance) in rapidly relieving the symptoms and signs of moderate or severe dry eye.2
“Anti-inflammatories, like cyclosporine products and lifitegrast, are generally used as a first-line therapy in people who have an immune component to their dry eye, such as Sjögren’s, graft-versus-host disease and other autoimmune diseases,” adds Dr. Galor. “But, of course, there are no absolutes and there are a lot of crossovers, so people with autoimmune dry eye also get MGD, and they often get prescribed antibiotics. People who have ocular surface inflammation, without a known autoimmune disease, often get a trial of an anti-inflammatory medication.”
Other ways to reduce inflammation in dry-eye patients is by treating with antibiotics. “A lot of the antibiotics that we use in the realm of ocular surface disease actually have some anti-inflammatory properties, and that’s where doxycycline, minocycline and azithromycin–both topical and oral–have antibiotic properties which can certainly help when there’s bacteria that are sensitive to those antibiotics,” says Dr. Starr. “They can help debulk the bacterial load, the lid margin and the ocular surface, and can play a role in everything from bacterial conjunctivitis to things like MGD and anterior blepharitis. Their anti-inflammatory properties are beneficial in the ocular surface diseases where inflammation is the core mechanism and pathophysiology.”
A novel approach to reducing inflammation and increasing tear production is Oyster Point’s Tyrvaya (varenicline). “It’s a secretagogue that is applied to the nasal mucosa,” says Dr. Akpek. “Tyrvaya could be a good replacement for over-the-counter drops because it stimulates the natural tears and doesn’t upset tear-film homeostasis through drop instillation.”
Dr. Starr adds that “this neurostimulation nasal spray for dry eye very likely reduces inflammation with long-term treatment.”
 |
| Click image to enlarge. |
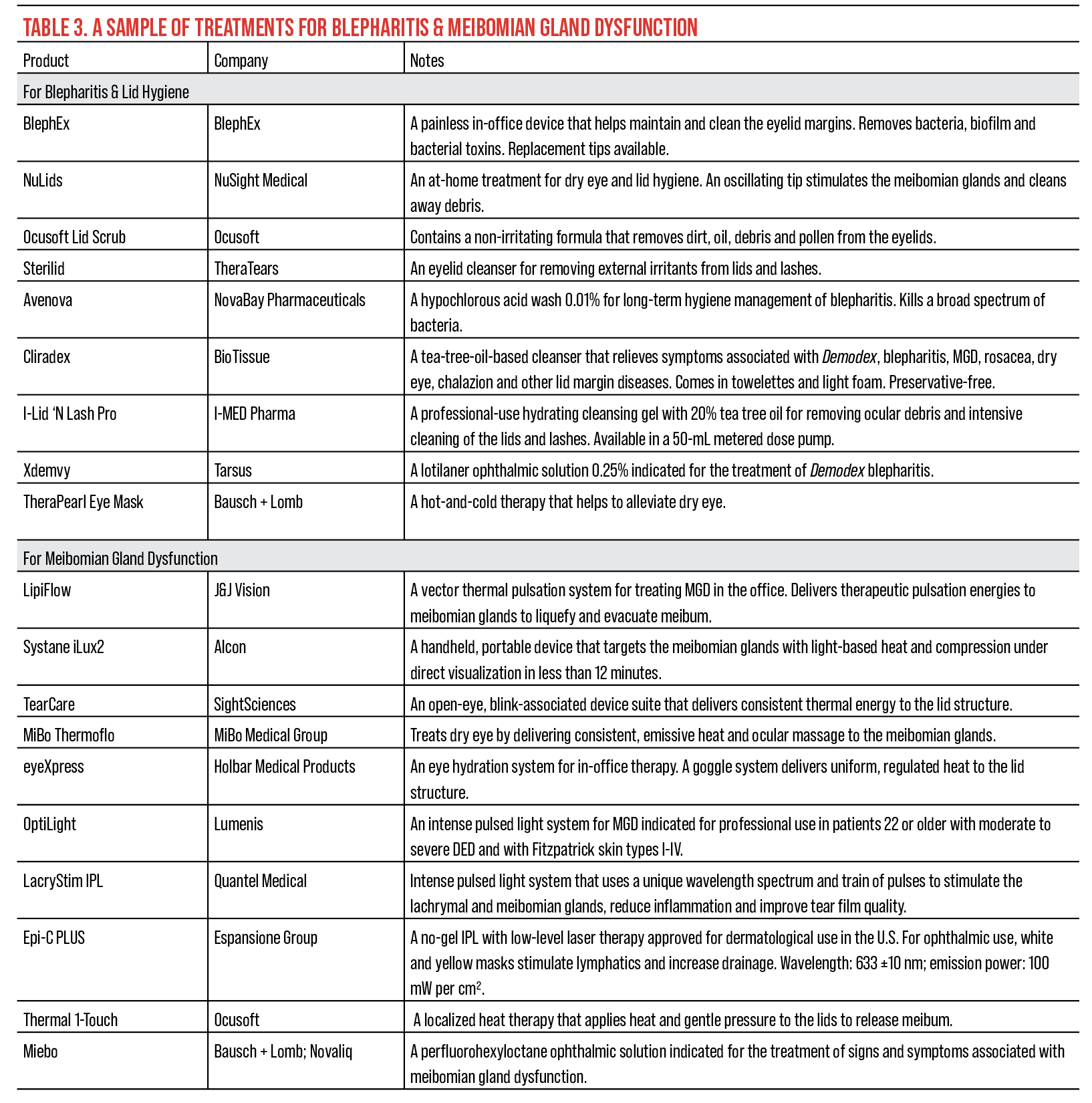
Treating MGD and Blepharitis
“MGD can present itself in several ways,” says Dr. Galor. “Some patients present with plugging and/or keratinization of the gland openings, others with thick, toothpaste-like meibum or gland dropout. Over-the-counter approaches to MGD including heating masks along with the eyelid hygiene. There are several products available over the counter for this purpose.
“There are also a lot of office-based procedures that target different aspects of MGD,” Dr. Galor continues. “When people have intact glands but poor meibum quality, a procedure that heats and/or massages the lids can be used. Some of the clinically available devices include LipiFlow [J&J Vision], Systane iLux2 [Alcon] and TearCare [SightSciences], to name a few.”
“Some people have keratinization and/or obstruction of their meibomian glands, and in this, situation eyelid probing can be considered,” says Dr. Galor. “For this procedure, a small probe is introduced into the meibomian gland opening to try to relieve the obstruction.” For example, Maskin MGI probes (Katena) along with a jojoba anesthetic ointment containing 8% lidocaine releases periductal fibroses from meibomian glands, freeing glands from strictures that block the flow of indispensable meibum.3
“IPL, or intense pulse light, is gaining traction, and there’s growing evidence that it can help treat some forms of blepharitis and MGD with intense pulses of light, often in patients with rosacea and ocular lid margin disease,” says Dr. Starr. Products such as OptiLight (Lumenis) and LacryStim IPL (Quantel Medical) use wavelengths of light to stimulate the meibomian glands to facilitate the secretion of meibum, along with other beneficial mechanisms.
“Blepharitis is tied to dry-eye disease because it has an impact on the meibomian glands,” says Dr. Starr. “If there’s blepharitis, I want to know if it’s anterior, posterior or both; if it’s due to bacteria, to Demodex, to medications, to hormones, or to a whole host of things, because that helps me to guide my treatment.”
Depending on whether the blepharitis is anterior, posterior or mixed, the treatment options may differ. “When people have anterior blepharitis, removing the debris on the eyelashes with BlephEx is an option,” says Dr. Galor. BlephEx is a microblepharoexfoliation device that removes bacteria and toxins from the eyelids. For posterior treatments, Cliradex (BioTissue), containing 4-terpineol, a compound found in tea tree oil, cleanses the eyelid, ridding the surface of Demodex. Additionally, practitioners now have access to Xdemvy (lotilaner ophthalmic solution 0.25%), the first FDA-approved treatment for Demodex blepharitis.
“When you start talking about parasitic mites that live in your eyelids and crawl out onto your eyelid margin and deposit eggs and waste products on your eyelashes, that’s really an uncomfortable conversation to have with a patient,” says Dr. Starr. “If you see the collarettes, it’s pathognomonic and you want to decrease the mite burden and population.”
 |
| Click image to enlarge. |
Contact Lenses
There’s also an interplay between contact lens use and dry-eye signs and symptoms.
“Contact lens wear can affect the eye in two ways: First, we think it affects the health of the meibomian glands,” says Dr. Galor. “Patients who are long-time contact lens wearers often have meibomian gland dropout on exam. We believe that contact lens wear at least partially contributes to this finding. Second, contact lens wear can also impact corneal nerves. People who wear contact lenses for a long time sometimes lose nerve sensitivity, so they don’t respond to the environment as robustly as they should.”
Proposing daily disposable contact lenses can help reduce the risk of DED. “We find that the daily disposable contact lenses with the more modern materials tend to be the safest of all and provide the least induction of major ocular surface issues in dry eye,” says Dr. Starr. “These tend to be very well tolerated, leading to lower risks of infections and hypoxia.”
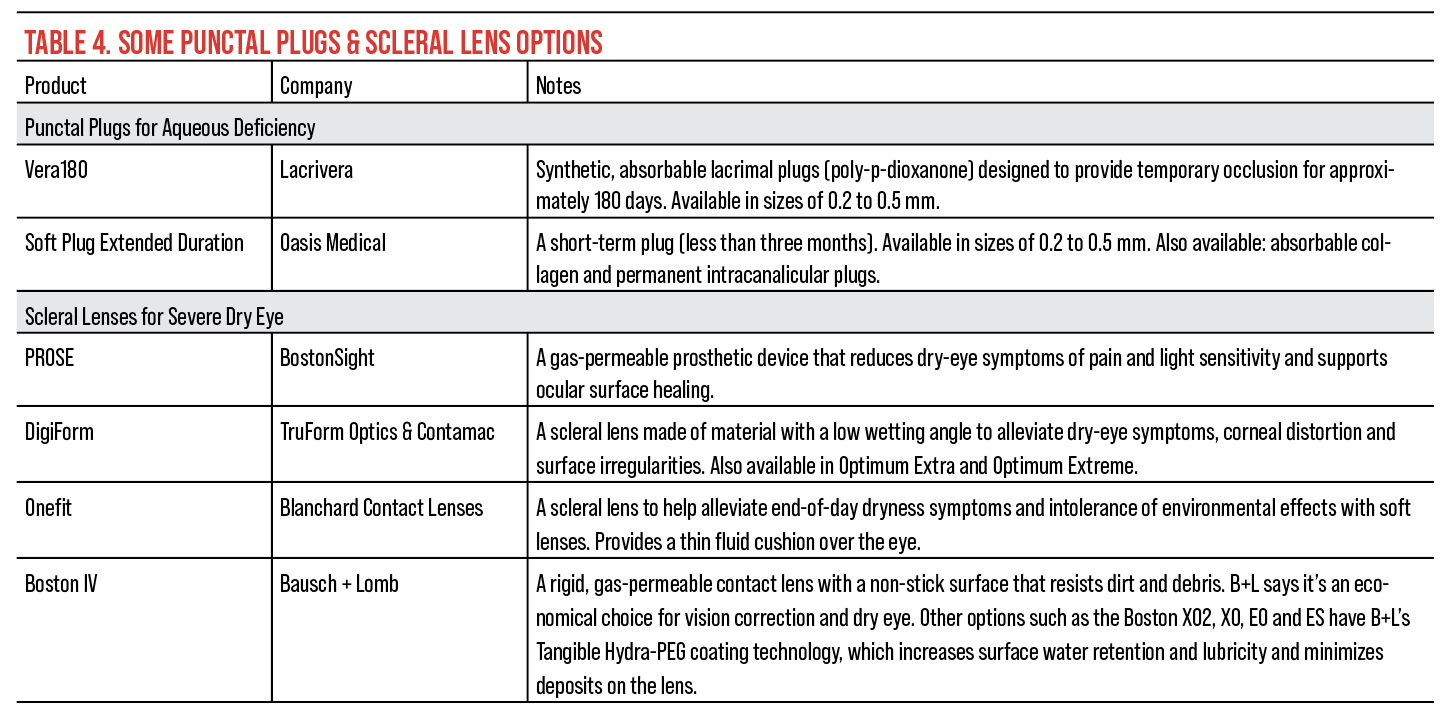
For more severe dry-eye cases, clinicians can offer more durable and advanced contact lens options. “Scleral lenses are a good option for individuals with very low tear production and corneal and conjunctival epithelial disruption,” says Dr. Galor. “Scleral lenses produce an artificial tear layer underneath the lens that protects the surface during the day. You can also put autologous serum tears in the scleral lens to give the surface extra growth factors.”
Patients should be well educated about other treatment options and the long-term effects of scleral lenses before moving forward. “They are permanent in that the patient will have to wear them for prolonged periods of time,” says Dr. Akpek. “It’s not an interim treatment. It’s sort of like a last-resort treatment, and that’s usually done after attempting to improve the tear secretion or production and then lessening the tear loss by basically blocking the tear ducts and putting the patient on the autologous tears to renew and regenerate the epithelium.”
Autologous Serum Eye Drops
As pointed out in the previous section, autologous serum tears can go hand-in-hand with scleral lenses, as well as other lens options. Formulating autologous serum eye drops is a process in which the cellular and liquid components of a patient’s blood are separated in a diluted saline solution, which contains biological nutrients that are similarly present in tears.4
“For me, the autologous serum drops are generally reserved for the more advanced, higher-severity-level ocular surface and dry-eye disease patients,” says Dr. Starr. “Because one will try traditional treatments first from over-the-counter products to FDA-approved prescription medications, punctal plugs, procedural treatments, and so on and so forth. It’s in patients with more severe disease–these are generally cases with autoimmune disease, chemical burns and chronic cicatrizing issues–that’s not necessarily amendable to multiple traditional treatments.”
Dr. Akpek elaborates further on how to use these eye drops. “In those patients who don’t respond to, for example, bandage contact lenses, punctal plugs or trying to improve the corneal epithelium, autologous serum tears with a concentration from 20 to 100 percent, four-to-six times a day, could be used,” says Dr. Akpek. “In order to enhance corneal epithelium regeneration, I do frequently employ autologous serum eye drops, whether the dry eye is aqueous deficient or evaporative.”
Recent FDA Approvals
There have been recent FDA approvals as well. Miebo (Bausch + Lomb; Novaliq) Vevye (Novaliq) and Xdemvy (Tarsus) are the latest treatments to receive approval in 2023.
Miebo (perfluorohexyloctane ophthalmic solution, Bausch + Lomb), originally NOV03, is a prescription eye drop for DED that directly targets tear evaporation, especially in cases with MGD. Miebo underwent two Phase III studies, GOBI and MOJAVE. According to the clinical studies, Miebo met both its primary sign and symptom efficacy endpoints. The two primary endpoints studied were the change from baseline at week eight in total corneal fluorescein staining (tCFS) and eye dryness Visual Analog Scale (VAS) score. Researchers reported that Miebo patients experienced relief from their symptoms as early as day 15 with statistically significant reductions in VAS eye dryness scores. There was also a significant reduction in tCFS at day 15 as observed in both studies. The most common adverse reactions patients experienced were blurred vision (1.3 percent, GOBI; 3 percent, MOJAVE) and eye redness (1 percent, GOBI; 3 percent, MOJAVE).
Vevye (cyclosporine 0.1%, Novaliq), originally CyclASol, is a prescription eye drop for the treatment of signs and symptoms of DED. According to clinical trials, Vevye’s safety and efficacy was assessed in a total of 1,369 patients with dry-eye disease, of which 738 received Vevye. The primary endpoint was the percentage of patients achieving ≥10-mm improvement from baseline in Schirmer’s Tear Test score. In the CYS-002 study, 8 percent of 51 Vevye patients achieved this endpoint at 29 days as opposed to 0 percent in the placebo group (n=51). In the CYS-004 study, 11 percent of 409 Vevye patients achieved this endpoint at 29 days as opposed to 7 percent of the 395-patient placebo group. The most common adverse effects Vevye patients experienced were instillation-site reactions (8 percent) and temporary decrease in visual acuity (3 percent).
Xdemvy (lotilaner 0.25%, Tarsus), originally TP-03, is a prescription eye drop for the treatment of Demodex blepharitis. According to clinical trials, efficacy was demonstrated by a significant improvement in the reduction of collarettes by day 43, with some patients seeing improvement as early as two weeks. The endpoints in two Phase III studies, SATURN-1 and SATURN-2 (n=833), observed mite eradication and erythema cure. Out of 833 patients, 415 recieved Xdemvy for treatment and 418 recieved a placebo.
In the SATURN-1 trial, 81 percent of Xdemvy patients had a collarette grade of 0 or 1 (range 0 to 4, where Grade 0 indicates ≤2 collarettes on the eyelid and Grade 4 indicates ≥ two-thirds of the eyelid has collarettes) on day 43 as opposed to 23 percent in the placebo group. In the SATURN-2, 89 percent of Xdemvy patients had similar results to those in the treatment arm of SATURN-1 as opposed to 33 percent in the placebo group.
By day 15, the SATURN-1 trial reported 68 percent of Xdemvy patients achieved complete mite eradication. The most common adverse reactions patients experienced were instillation site stinging and burning (10 percent), and more severe reactions experienced were chalazion and punctate keratitis (2 percent).
“When looking under a slit lamp you’ll see the collarettes, especially in somebody who has symptoms of dry eye or recurrent itchy, scaly lid margins.” says Dr. Starr. “This can be treated with the approved drop. I’m sure there’s going to be a lot of aftermarket studies looking at things like adjuncts that might make Xdemvy more effective and work faster."
Dr. Starr is a consultant for Allergan, Bausch + Lomb, Kala Pharmaceuticals, Novartis Pharmaceuticals and Oyster Point Pharma and has been affiliated with the Bausch + Lomb medical education program. Dr. Galor is a consultant for Novaliq, Novartis Pharmaceuticals, AstraZeneca, Dompé, Tarsus, Bausch + Lomb, and Allergan. Dr. Akpek is a consultant for Dompé, HanAll, Iolyx, Kyria, Novaliq, Sinqi and Xequel and has received research support from Novartis Pharmaceuticals and Ocular Therapeutics.
1. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf 2017;15:3:276-283.
2. Yang CQ, Sun W, Gu YS. A clinical study of the efficacy of topical corticosteroids on dry eye. J Zhejiang Univ Sci B 2006;7:8:675-8.
3. Detailed review of the maskin protocol for meibomian gland probing. MGD Innovations. https://mgdi.com/detailed-mg-probing-protocol. August 11, 2023.
4. Valencia Castillo SL, Martín ES, García Frade LJ, et al. Autologous serum eye drops improve tear production, both lachrymal flow and stability tests and conjunctival impression cytology with transfer in dry eye disease. Blood Transfus 2021;19:1:45-53.