In an effort to boost their practice’s bottom line, some surgeons are finding success by expanding the diagnosis and treatment options to their dry-eye patient population.
One benefit of offering dry-eye services is that it can convert nonsurgical candidates to surgical candidates. “In a refractive surgery practice, there are patients who may not qualify for laser correction because of their meibomian gland dysfunction and dry eyes,” says Sheldon Herzig, MD, medical director and co-founder of the Herzig Eye Institute in Toronto, Ontario, Canada. “Having an established dry-eye clinic to help these patients preoperatively, providing the most advanced technologies to perhaps restore normal tear function, can convert a non-candidate to one who does very well with refractive surgery.”
Dr. Herzig notes that dry-eye patients can consume a lot of chair time in a busy practice, so having a dedicated dry-eye clinic that is appropriately staffed and equipped will not only deal with dry-eye disease more efficiently but will also help keep the practice running more efficiently.
Marguerite McDonald, MD, from Ophthalmic Consultants of Long Island in New York, has incorporated a dry-eye center of excellence in her practice. “There is signage about it everywhere, and there are booklets and leaflets in every single room,” she says. “We try hard to stay on time, but most patients have time to scan at least one brochure while they are waiting for the doctor to come in. Even if they haven’t heard of us being a dry-eye center of excellence, they will leave knowing that we are, and they often tell their friends. There is a lot of word-of-mouth referral in a dry-eye practice. If you make an unhappy middle-aged dry-eye patient happy after she has been to five or six doctors, the halo effect is incredible. You are much more likely to get her daughter’s LASIK and her father’s cataract surgery.”
All patients seen in the practice take a very short questionnaire. It takes them less than 30 seconds to check off whether or not they have symptoms of dry eye and the frequency of those symptoms. Tear osmolarity testing is ordered on any patient who checks off ocular surface symptoms on the questionnaire and on most patients who are 40 or older, because the incidence of dry-eye spikes in this age group. “Additionally, I order tear osmolarity on anyone presenting for any kind of ophthalmic surgery and on anyone with a history of dry eyes. Honestly, there aren’t very many people in a cornea specialist’s practice who don’t get a tear osmolarity test as part of their exam,” she says.
Dr. McDonald uses the results of the tear osmolarity test to guide therapy. A normal score is 290 to 295 mOsm/L. At this score, the tears are in homeostasis with the blood, which is normal and healthy. For every point above this score, the eyes are drier. If a patient is between 295 and 310 mOsm/L, she is asked to use artificial tears four times a day. In severe cases, patients are on lid scrubs twice a day and erythromycin ointment at night, low-dose doxycycline by mouth, artificial tears four to eight times a day, and nutritional supplements. This can be overwhelming for many patients. In these cases or in cases where the patient is unable to complete this regimen, Dr. McDonald offers LipiFlow.
LipiFlow, LipiView and IPL
Adding LipiView, LipiFlow and intense pulsed light therapy to a practice is one way to boost revenue. “Dry eye is becoming a more attractive market now because there are more objective diagnostic tools and in-office therapeutic treatments that have expanded our armamentarium,” says Elizabeth Yeu, MD, an assistant professor at Eastern Virginia Medical School and corneal specialist at Virginia Eye Consultants in Norfolk, VA.
LipiView is a diagnostic tool that, to a certain degree, quantifies the meibum and helps objectively gauge how patients may respond to a LipiFlow treatment, she adds. “LipiView provides a numerical measurement of the thickness of the lipid layer within the tear film, with value ranges that correlate this to posterior lid margin disease severity,” says Dr. Yeu.
LipiFlow and intense pulsed light are the newest treatment options for dry eye. Dr. McDonald says that LipiFlow has a high conversion rate in her practice. “It is a 12-minute computer-controlled pulsating thermal lid massage treatment that is highly effective in treating dry eye,” she says. “The LipiFlow treatment is not covered by insurance, so—for the average practice with the average LipiFlow pricing structure—the margins are usually at least as good as if the surgeon performed a LASIK procedure. Another advantage to the LipiFlow treatment is that there is just about no medicolegal liability with it; I have never heard of a LipiFlow lawsuit because it is so noninvasive.”
Jay Pepose, MD, PhD, medical director of Pepose Vision Institute and president of the Lifelong Vision Institute in St. Louis, notes that LipiFlow should not just be considered as a last-resort treatment option. “The patients who are trying LipiFlow as a last resort are the most motivated, but you have to be careful with them because if you have someone with no meibomian gland function, those patients are so end-stage that they may not respond to the treatment. It is always better to catch people before end-stage, while they still have some functional glands,” he says.
Another procedure used to treat dry eye is intense pulsed light, or IPL. “I like the concept but there is very little published about it compared to how much is published about other treatments, such as LipiFlow,” Dr. McDonald says. “There is a little more liability with IPL, so you have to be careful: Patients who are more darkly pigmented can get scarring, and one has to remember to insert the eye shields or there can be ocular damage.”
Adding new treatment options can disrupt patient flow, so you may want to consider grouping dry-eye patient visits. “When we first started offering LipiFlow, when a patient said he or she wanted it, we were doing it right that very moment,” Dr. McDonald says. “However, this made patient flow a bit chaotic. Because it is a 12-minute procedure, we decided to have ‘Dry-eye Fridays.’ We do LipiFlow treatments all day on Fridays. We have now trained our optometrists to perform LipiFlow procedures, but we did them ourselves until we felt we had done enough to be totally comfortable with these treatments.”
The Bottom Line
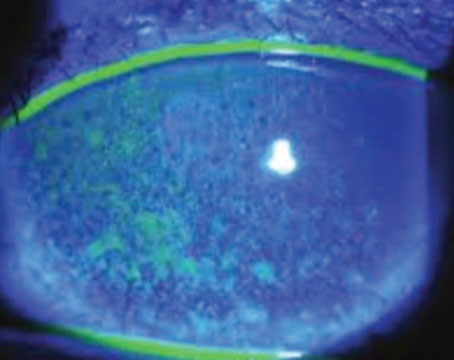
Other ways to increase income include tear osmolarity testing and taking anterior segment images. “The Keratograph 5M by Oculus has—in addition to a Placido-based topographer—five new images that assist in the diagnosis of dry eye and meibomian gland disease and the response to treatment,” Dr. McDonald says. “For instance, it has an automated tear breakup time, which is notoriously difficult to measure by clinical observation only. Not only does it tell you what the tear breakup time is, but it shows you what part of the cornea broke up first. It will give you the average breakup time in seconds and will classify the level of dry eye. It also has meibography, so the glands can be seen and the gland-containing area of the lid can be calculated, as well as demonstrating gland tortuosity and documenting where on the lid the dropout is occurring. It also has a way to categorize conjunctival erythema by calculating the ratio of blood vessels to sclera. It will accurately and automatically stage conjunctival erythema for the clinician, so it takes away the subjectivity of staging ‘redness.’ ”
Additionally, it determines the thickness of the lipid layer using interferometry, provides automatic measurement of the tear meniscus height, and tracks the movement of particles in the tear film to determine tear viscosity. “The practice can invoice for these photographs using the external photography CPT code, and the average reimbursement for these photos is $40,” Dr. McDonald says.
To develop a dry-eye center of excellence, Dr. McDonald recommends starting with tear osmolarity first. “Get the doctors and staff comfortable with how to do it and when to do it. Once you have that under your belt, you should quickly move on to acquiring LipiFlow technology and the Keratograph 5M,” she says.
However, be prepared for a big price tag. “The Keratograph 5M is approximately $25,000 to $28,000. The LipiFlow/LipiView package from TearScience is around $100,000,” she says.
To defray these costs, Dr. Yeu says she has heard of practices that are collectively purchasing the fairly portable unit and are sharing the LipiFlow like a “timeshare,” where the unit travels between the practices on a rotating schedule. “The machine can go to one practice one week and then to another practice the next week,” she says. “Another great idea to help cover the overhead may be to consider offering your referring ophthalmologists and optometrists the option of bringing their patients over and allowing them to perform their own treatments.”
Dr. Yeu believes that the use of LipiFlow to treat dry eye is on the rise. “Although it’s still a relatively newer therapy and there is not as much out there in evidence-based literature to support this yet, we believe that the LipiFlow will likely grow in its indications,” she says. “I would not be surprised to see this being utilized in all realms of mild to moderate dry-eye disease, not just for the obvious evaporative ones. In-office meibomian gland expression is going to be more and more widely utilized. It is like any other chronic disease in that there is no single modality therapy that is a cure-all. I think LipiFlow is a great adjunctive professional therapy that will continue to grow and gain greater momentum in the next few years and is certainly not a fad treatment.”
Even if you are not interested in getting in this deep and purchasing expensive equipment, your practice can still capitalize by simply expanding your dry-eye patient base and following them. These added patients will also expand your surgical population as they later require cataract surgery or glaucoma treatment.
Bruce Maller, an ophthalmic business consultant, has developed a conservative dry-eye financial model (See Tables 1 & 2). First, he provides an example of a dry-eye patient’s visits/charges for one year if a patient had the chief complaint of blurry vision. Visits alone would bring in $354 per patient per year. Additionally, if two punctal plugs were implanted, the revenue would be $219 per patient, and the revenue for four plugs is $370 per patient.
Then, he calculates the revenue and net income opportunity for a practice that was able to bring in 1,500 dry-eye patients, which is a conservative estimate according to Dr. McDonald. “Bruce assumes that with very modest marketing, it would be fairly easy for any practice to get 1,500 new dry-eye patients to come in over the course of a year,” she says. “Based on several recent Gallup polls, Bruce was able to calculate how many cataract, glaucoma and retina cases would be found in those 1,500 dry-eye patients. He assumed that the ophthalmologist will only be able to keep half of them in the practice. Though Bruce used modest estimates in every instance, as well as 2012 Medicare reimbursement rates, it was staggering how profitable this effort—an emphasis on treating dry eye—was to the average practice. You don’t have to stop treating cataracts or glaucoma or anything else; your volume of these cases will actually increase.”
When tear osmolarity testing is added to the model, an additional $160,800 of net revenue is possible. (See Table 3).
Other Innovative Ideas
For additional income, Dr. Pepose’s practice also sells some dry-eye products. “It is not terribly profitable but we have an optical, and the optical carries fish oil and different artificial tears,” he says. “We try to carry some that you can’t get too easily at the pharmacy. We want to have a good, non-preserved tear and a good, oil-containing tear. This also gets people into the optical, where they may make an additional purchase. Some practices are also initiating allergy skin testing, so we are looking into that because there is a lot of overlap in these patients between dry eye and allergy.”
Dr. McDonald believes that it is the perfect time to get into this field because of the demographic shift in the population. In addition, there are better diagnostics, better drugs and better procedures for ocular surface disease. “We can do more for these patients than ever before, and with virtually no medicolegal exposure,” she notes. REVIEW