Dry eye’s effects on quality of life and vision are more widely recognized today, especially in the refractive cataract surgery space, where an optimized ocular surface is vital for obtaining accurate corneal measurements. There are an abundance of dry-eye treatment options, with more advances coming down the pipeline each day. Nevertheless, the condition remains challenging to treat due to its multifactorial nature and often conflicting signs and symptoms. Here, experts discuss their treatment strategies for the many faces of dry eye.
Redefining the Disease
 |
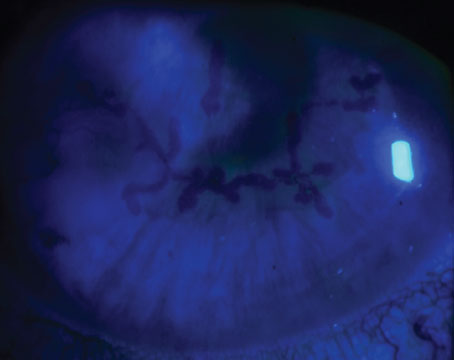
| In this eye, no lissamine green stain is visible under the area covered by the scleral lens. Photo: Mina Massaro-Giordano, MD. |
Experts note that dry eye’s range of clinical presentations and symptoms has made it a challenge to define, and the lack of standardized terminology has hindered the strength of research. “Patients with dry eye don’t necessarily have dry eyes,” points out Mina Massaro-Giordano, MD, co-director of the University of Pennsylvania’s Dry Eye and Ocular Surface Center in Philadelphia. “There are multiple causes for ocular surface disease. The challenge is homing in on the right ones to tailor your treatment, which requires constant monitoring and management, usually with more than one medication.”
There have been several definitions and diagnostic criteria for DED over the years, including those proposed by the National Eye Institute, the Tear Film & Ocular Surface Society Dry Eye Workshops I and II, the Japanese Dry Eye Research Group, the Korean Corneal Disease Study group, the Asia Dry Eye Society and the American Academy of Ophthalmology.
The most recent definition, published in the International Journal of Molecular Sciences in 2020, was drafted with the clinician in mind by a group of global DED experts who convened at four meetings between 2016 and 2018. Their consensus definition states: “Dry eye is a multifactorial disease characterized by a persistently unstable and/or deficient tear film causing discomfort and/or visual impairment, accompanied by variable degrees of ocular surface epitheliopathy, inflammation and neurosensory abnormalities.”1
Stephen C. Pflugfelder, MD, of Houston’s Baylor College of Medicine, says the new definition is meant to be clinically applicable and to promote consistent diagnoses. “The group felt that dry eye is really a disease defined by an unstable tear film,” he explained. “Tear dysfunction is easy to measure in the clinic, making it a practical and reproducible marker of DED. Once tear-film instability has been identified, additional testing can be done to identify the underlying cause of the dry eye, such as inflammation levels or other factors associated with an unstable tear film.”
 |
Mild Dry Eye
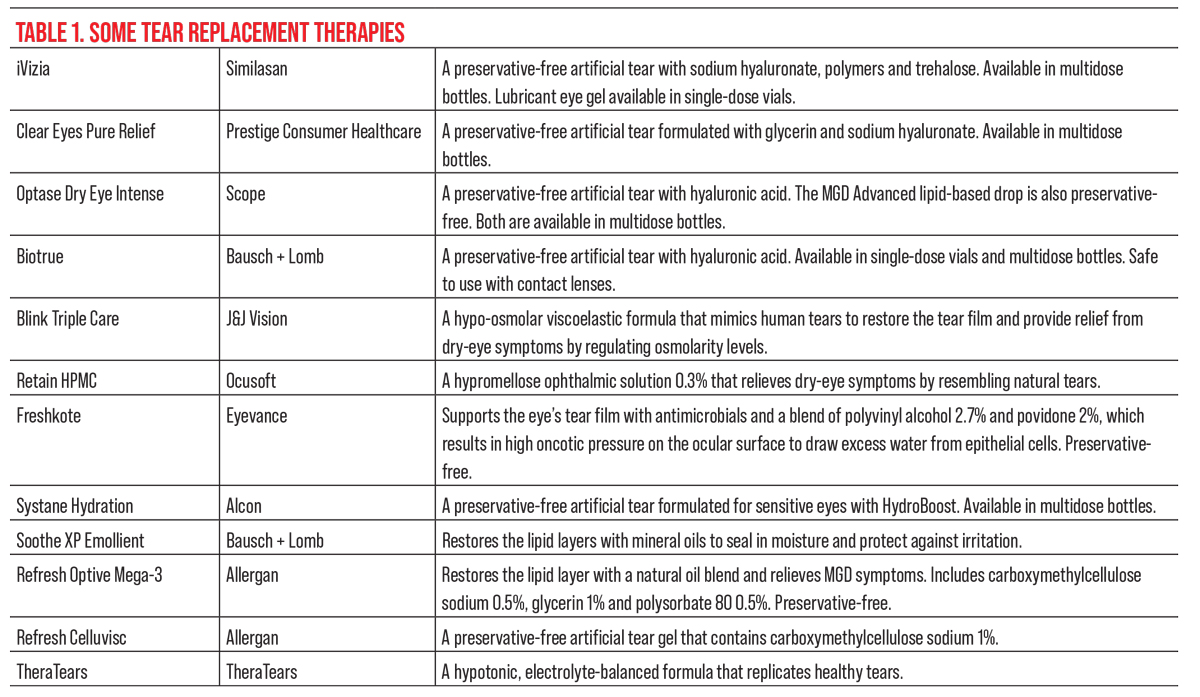
Clinicians say almost any artificial tear available over the counter will effectively alleviate some mild dry-eye symptoms. “I don’t make a big distinction among the different brands, but I may recommend a tear with a lipid-based component, for example, if there’s a meibomian gland problem,” says Grayson W. Armstrong, MD, MPH, of the Massachusetts Eye and Ear Infirmary. “I tell my patients they’ll probably be fine with any OTC tear. I’ll push them to use preservative-free options if they’re going to be using drops frequently (e.g., more than four times per day).”
“There haven’t been many head-to-head comparisons of various artificial tears, but certain components may give some formulas an edge over others,” Dr. Pflugfelder says. “Personally, I prefer artificial tears that contain hyaluronic acid. There are a number of those in the United States [e.g., Blink Tears (Johnson & Johnson Vision) and Systane Hydration PF (Alcon)]. Hyaluronic acid tends to lubricate and retain tears better because it binds moisture to the eye and reduces surface friction. There are also tears with osmoprotectants in them such as glycerin, erythritol and carnitine, which may decrease inflammation and protect the eye from high osmolarity.”
Proactive artificial tear use goes a long way toward providing symptom relief. In addition to using tears throughout the day, if necessary, Dr. Armstrong specifically encourages his patients to instill tears before they plan to read, look at their phone or do computer work for long periods of time. “Many of my patients tell me their dry eye is worse in the evening, which also happens to be when they read,” he says. “Using drops prophylactically, remembering to blink and taking breaks every 20 minutes is sometimes enough for cases of mild dry eye.”
Though artificial tears are a mainstay of DED care, experts note that they’re not always appropriate for every patient as a first-line option. “In general, I find that patients are pretty noncompliant with artificial tears,” Dr. Armstrong says. “I try to recommend a treatment that makes sense for the patient’s compliance level. Sometimes I’ll recommend warm compresses or lid scrubs first if the patient has a meibomian gland or blepharitis problem. In Massachusetts, we have a cold climate, and heaters dry out patients’ homes, so I’ll often suggest using a humidifier as well.”
Making small environmental or behavioral changes can alleviate some mild dry-eye symptoms, Dr. Pflugfelder points out. For mild “level-one” cases, he also often recommends humidifiers and other modifications such as avoiding drafts or positioning the video display at eye level. “It depends on patient preference,” he says. “If they don’t respond to these measures, or to artificial tears, I often introduce an anti-inflammatory therapy.”
For patients with aqueous deficiency, punctal plugs may also provide some relief. “I start with dissolvable plugs (three- or six-month duration) because I’m not sure the patient will like them,” Dr. Pflugfelder says. “Non-dissolvable plugs are usually made of silicone, and they have a mushroom shape, so there’s a portion of the plug that comes out to rest on top of the punctum. Sometimes it rubs on the eye, whereas the absorbable ones are intracanalicular, so nothing’s sticking out.”
 |
The Multidose PF Revolution
Clinicians tend to nudge patients toward preservative-free options to avoid the toxicity of BAK, which can worsen dry eye. In the past, preservative-free artificial tears were only available in single-dose vials, but thanks to developments in preservative-free multidose bottle technology, patients no longer have to deal with those tiny vials.
Unidirectional valves and air filters in multidose PF bottles ensure any remaining drops or outside contaminants don’t enter or re-enter the sterile bottle. Some artificial tears with this technology include Optase Intense (Scope), Freshkote PF (Eyevance), Retain HPMC (Ocusoft), Oasis Tears PF (Oasis Medical), iVizia (Similasan), Refresh Relieva PF (Allergan), Biotrue (Bausch + Lomb), Clear Eyes Pure Relief (Prestige Consumer Healthcare) and Systane Hydration (Alcon).
“This is a really nice technology,” Dr. Armstrong says. “These options tend to be a little more expensive at the outset than the single-dose vials or normal OTC artificial tears, but you can keep using the same bottle until its expiration date instead of buying a new box every month or throwing out the vials at the end of each day. The multidose bottles work very well, and patients love them. This is going to be a game-changer.”
Trigeminal Nerve Stimulation
For patients who have difficulty instilling drops or are already using other topical medications, the nasal spray Tyrvaya (varenicline, Oyster Point) may provide some relief. “Tyrvaya harnesses the power of the nerves in the trigeminal nerve pathway to increase basal tear production,” Dr. Massaro-Giordano explains. “The spray stimulates the nerves to create a feedback loop to the lacrimal glands to help pump out lacrimal fluid. When these tears are collected, there’s extra oil and extra mucus, so it’s a better tear film.”
“My patients seem to like it, particularly the aqueous-deficient ones or patients who wear contact lenses,” Dr. Pflugfelder says. “It provides an almost immediate increase in their tears. They can feel their eyes are moister, and its effects may last for an hour or several hours. I’d say there’s a pretty high satisfaction level among these patients.”
Joseph Christenbury, MD, of Eye Consultants of Atlanta, offers Tyrvaya as a third-line option or adjunct therapy to his moderate and severe dry-eye patients who grow tired of or have difficulty using drops. “I counsel patients that the nasal spray will make them sneeze,” he says. “It’s another promising tool to have in your basket, especially for elderly patients and those with decreased mobility.”
Soothing Inflammation
When patients experience dry-eye flares, clinicians often turn to corticosteroid drops, such as Lotemax (loteprednol etabonate 0.5%, Bausch + Lomb), Eysuvis (loteprednol etabonate 0.25%, Kala) or Flarex FML (fluorometholone acetate 0.1%, Eyevance). Corticosteroids get the inflammation under control quickly so patients can begin or resume more conservative dry-eye treatments such as warm compresses or artificial tears. With a short, usually two-week, course, these are typically safe options, though clinicians emphasize the importance of checking your patient’s glaucoma status before initiating any steroid treatment. Patients with a history of poor contact lens hygiene may also be poor candidates for a steroid drop.
“For patients with symptoms unresolved by artificial tears, I may put them on a maintenance medication such as Xiidra, Restasis or Cequa, depending on their insurance plan and coverage,” Dr. Christenbury says. “Cequa has a higher concentration of cyclosporine than Restasis [0.09% vs. 0.05%], so sometimes that works if patients feel Restasis isn’t enough, but it mainly comes down to insurance coverage. There’s a generic Restasis available now, which may help reduce the cost burden.”
“I use Restasis for moderate to severe aqueous-deficient dry eye because these patients have reduced goblet cell numbers,” Dr. Pflugfelder says. “Any of the cyclosporine drops will increase goblet cells, which are known to be very helpful for maintaining eye health. I find Xiidra tends to be more beneficial for reducing symptoms rather than signs. Its effects on signs in the clinical trials were fairly minimal, but it can, in certain patients, provide a lot of symptomatic improvement. So, if patients have high symptom severity scores and don’t respond to milder treatments (for ‘level one’ and/or some pulsed corticosteroids) then I would consider Xiidra.”
Xiidra may be particularly helpful for patients with both dry eye and evidence of meibomian gland disease or rosacea blepharitis, Dr. Armstrong notes. “The anti-inflammatory aspect tends to do a good job of alleviating some of these symptoms,” he says. “There’s no generic version of Xiidra though, so if it’s pricey, I don’t push it on the patient.”
He adds that if patients have an underlying medical condition such as Sjögren’s syndrome or lupus, where autoimmune inflammation causes severe dry eye, he’s quick to offer Restasis at the first or second visit with the patient. “These patients tend to suffer from lots of dry eye,” he says. “It’s an immune issue where they just aren’t producing tears. Sjögren’s patients who start Restasis tend to do pretty well.”
Expressing Meibomian Glands
MGD treatment mainstays include warm compresses, eyelid massages, manual expression and devices that heat the lids or deliver pulsed light to encourage oil egress.
 |
Dr. Pflugfelder uses LipiFlow (J&J Vision) and Thermal 1-Touch (Ocusoft) devices in his practice. Thermal 1-Touch heats the lids and glands, which are then manually expressed. Patients return for repeat treatments about every six to eight weeks with the Thermal 1-Touch, he says. “There are reports of sustained effects for six months or longer, but it’s always hard to know,” he notes. “I’d say, just based on what patients prefer, it’d be about every few months, depending on out-of-pocket expenses.”
“The Systane iLux2 [Alcon] is a handheld thermal device,” Dr. Massaro-Giordano says. “With this device, the doctor gently squeezes the eyelid while applying heat to allow egress of the oil onto the surface of the eye.” Some other thermal devices include the MiBo Thermoflo (MiBo Medical Group) and eyeXpress (Holbar Medical Products).
Intense pulsed light devices such as OptiLight (Lumenis) and LacryStim IPL (Quantel Medical) are often used in combination with thermal devices to improve MGD and the tear film. IPL devices emit pulsed light at a wavelength in the 500- to 1,200-nm range, which selectively targets chromophores in telangiectasias. This eyelid vessel destruction is thought to inhibit the access of inflammatory mediators to the meibomian glands. The heat emitted may also help oil expression and destroy inflammation-causing bacteria. Be sure to consider your patient’s skin phototype before initiating IPL.
Before using a MGD device on his patients, Dr. Christenbury tries to clean up the glands and reduce inflammation with a month or so of doxycycline. “We’ve been using LipiFlow for years and recently got TearCare (Sight Sciences),” he says. “These devices aren’t 100-percent effective, but they kickstart the patient in the right direction. They heat and express the oil in the glands more effectively than compresses alone. They’re a good adjunct for your tough meibomian gland cases. Once-a-year treatments are usually enough to make a difference, but some patients prefer every six to nine months.
“If the MGD is severe or if there’s associated ocular rosacea, I’ll put patients on at least a month or two of doxycycline,” Dr. Christenbury adds. “I also like using Azasite as a topical drop to reduce inflammation in the glands and on the ocular surface.”
Managing Blepharitis
Pinpointing the cause of dry eye here is key. “If you just treat the eyeball when the patient has an eyelid problem—well, you can imagine how the inflamed eyelid continues to rub against the eye, exacerbating the problem,” says Dr. Massaro-Giordano. “Special ointments or steroids may help, depending on the etiology, and sometimes I give a pulsed dose of a stronger antibiotic steroid drop to treat the ocular surface. If they’re having a hard time healing the surface, I may add autologous serum.”
Half the battle of blepharitis is getting your patients to believe it’s real, says Dr. Armstrong. “I created a PowerPoint about blepharitis to show my patients what’s going on,” he says. “I found that if I just talked about it and tried to describe it, patients didn’t really believe it was real, but if I showed them photos of Demodex collarettes or redness and crusting on the eyelashes and lids, then they began to see it wasn’t just this made-up thing.”
Clinicians say it’s critical that patients do warm compresses once or twice a day, as well as eyelid massage and lid hygiene to remove debris with therapies such as Ocusoft lid scrub and cleansers, Sterilid (TheraTears), Avenova (NovaBay Pharmaceuticals) and Cliradex (BioTissue). Cliradex, a tea-tree-oil-based cleanser may be useful for managing the symptoms associated with Demodex blepharitis. An at-home device called NuLids (NuSight Medical) uses an oscillating tip to clean away debris.
For in-office treatments, there are I-Lid ‘N Lash Pro (I-MED Pharma), a 20% tea tree oil hydrating cleansing gel, and BlephEx (BlephEx), a device used to exfoliate along the lash line and remove inflammatory biofilm.
 |
Autologous Therapies
Serum tears are another option for treating DED when other treatments fail. “They’re a bit like super-powered artificial tears,” Dr.
Christenbury says. “They have nutrients and nerve growth factors, and they’re regenerative.” To obtain these serum tears, patients undergo a blood draw, and a compounding pharmacy spins the blood down and sends the serum tears to the patient.
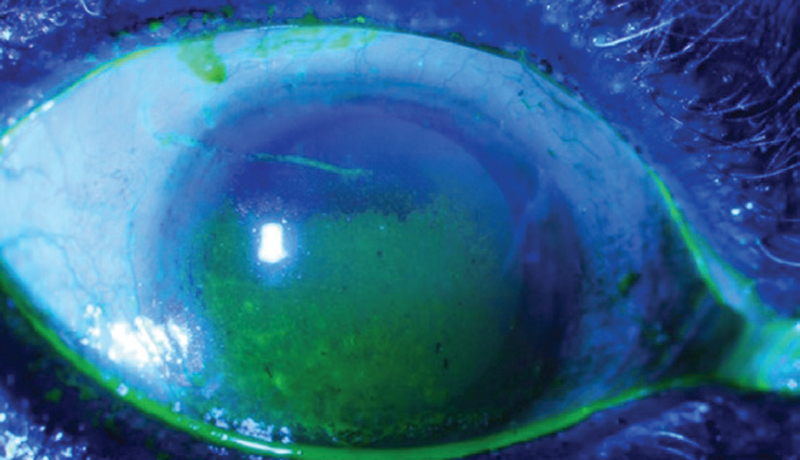 |
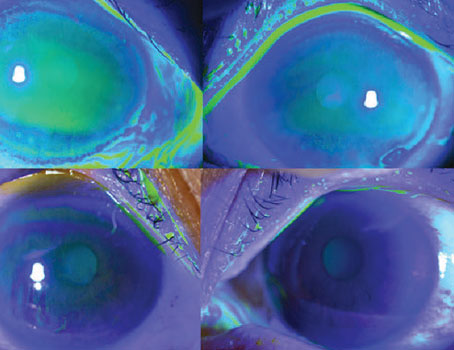
| A dry cornea with punctate epithelial keratoconjunctivitis with fluorescein staining. Photo: Mina Massaro-Giordano, MD. |
“Autologous serum eye drop treatments can help heal the ocular surface, but the downside is that they’re very expensive and usually not covered by insurance,” Dr. Massaro-Giordano points out. “There are different amniotic membrane products and serum products, and they all kind of work similarly, where growth factors are placed on the eye, whether in drop or contact lens form, to speed up healing.”
Dr. Pflugfelder frequently uses platelet-rich plasma tears in his patients. “At least in my hands, I find platelet-rich plasma to be more effective than serum tears or regular plasma,” he says. He and his colleagues published a multicenter study in The Ocular Surface a few months ago that reported that platelet-rich plasma was highly effective at treating signs and symptoms of ocular surface diseases such as DED, neurotrophic keratopathy, dormant corneal ulcers, limbal stem cell deficiency and cicatrizing conjunctivitis.2 Almost three-quarters of patients demonstrated an improvement in corneal staining from baseline. The number who had punctate epithelial erosions or epithelial defects dropped from 76.5 to 47 percent and from 23.5 to 7.8 percent, respectively (p<0.0001). SANDE score symptoms also decreased significantly at six month follow-up (median: 90 to 34.6, out of 100 points; p<0.0001).
Amniotic membrane is a less-often-used therapy for severe dry-eye, but proponents say it’s effective. Dr. Christenbury uses cryo-preserved amniotic membrane. He says the treatment works rapidly with effects lasting for a few months. “Amniotic membrane doesn’t rely on patient compliance,” he points out. “It’s good for healing and regenerating the ocular surface. The membrane remains on the eye for five to seven days, and then we remove it. We counsel patients that their vision will be blurry during that time.”
Scleral Lenses
Scleral lenses are used frequently for moderate and severe dry eye, particularly in cases of corneal epithelial disease, Sjögren’s syndrome and graft versus host disease. “There’s probably nothing better for protecting the cornea, improving symptoms and decreasing light sensitivity in moderate to severe dry eye than scleral lenses,” says Dr. Pflugfelder.
Scleral lenses sit on the scleral portion of the eye and vault over the cornea. “These lenses are filled with fluid, so the cornea is bathed in fluid the whole day,” Dr. Massaro-Giordano says. “These work very nicely for some patients.”
“We fit a variety of scleral lenses,” Dr. Pflugfelder says. “The lens with the highest satisfaction rating is probably PROSE (BostonSight) because it’s completely custom-fit. Unfortunately, it also tends to be the most expensive. These lenses are fit using computer-aided design to adjust the diameter or vault.”
“We’re lucky to be in a field where there’s always new and amazing medications coming down the pipeline,” says Dr. Armstrong. “We’re seeing advances in topical therapies, gene therapies, and nerve stimulators. There’s always something to look forward to at the next academic meeting.”
Dr. Christenbury is a speaker for BioTissue. Dr. Pflugfelder is a consultant for AbbVie, Dompé, Kala Pharmaceuticals, Aerie, Allergan and Kowa. Dr. Massaro-Giordano is a consultant for Oyster Point, Kala, Physician Recommended Nutriceuticals, Clarus and Dompé. Dr. Armstrong has no related financial disclosures.
1. Tsubota K, Pflugfelder SC, Liu Z, et al. Defining dry eye from a clinical perspective. Int J Mol Sci 2020;21:9271. [Epub December 4, 2020].
2. Soifer M, Tovar A, Wang M, et al. A multicenter report of the use of plasma rich in growth factors (PRGF) for the treatment of patients with ocular surface diseases in North America. The Ocular Surface 2022;25:40-48.