Tabletop visual field analysis is the gold standard for assessing the functional component of glaucoma and following patients over time to look for progression of disease, but the test results are difficult to interpret. The test is operator- and patient-dependent, and the results shouldn’t be considered in isolation, physicians say. Here, glaucoma experts review the strengths and weaknesses of visual field testing, as well as provide their tips on interpreting patients’ fields.
Visual Fields: An Overview
“When patients are diagnosed with glaucoma, they either have no functional deficits and a normal visual field, or they have some deficits. Once we establish a baseline with the visual field and initiate treatment, then we monitor that over time and look for any changes that might indicate progression of their glaucoma,” explains Leonard Seibold, MD, who is in practice in Aurora, Colorado.
According to Jonathan Eisengart, MD, who is in practice at the Cleveland Clinic in Ohio, the visual field test can face challenges from the test-takers themselves. “To take this test, patients need to be able to cooperate, so they need to be able to pay attention and not fall asleep, which is hard for many people. Additionally, they need to have reflexes that are fast enough to push the button when the light flashes. Cataract, corneal disease, or retinal disease certainly can affect the outcome of the visual field,” he says.
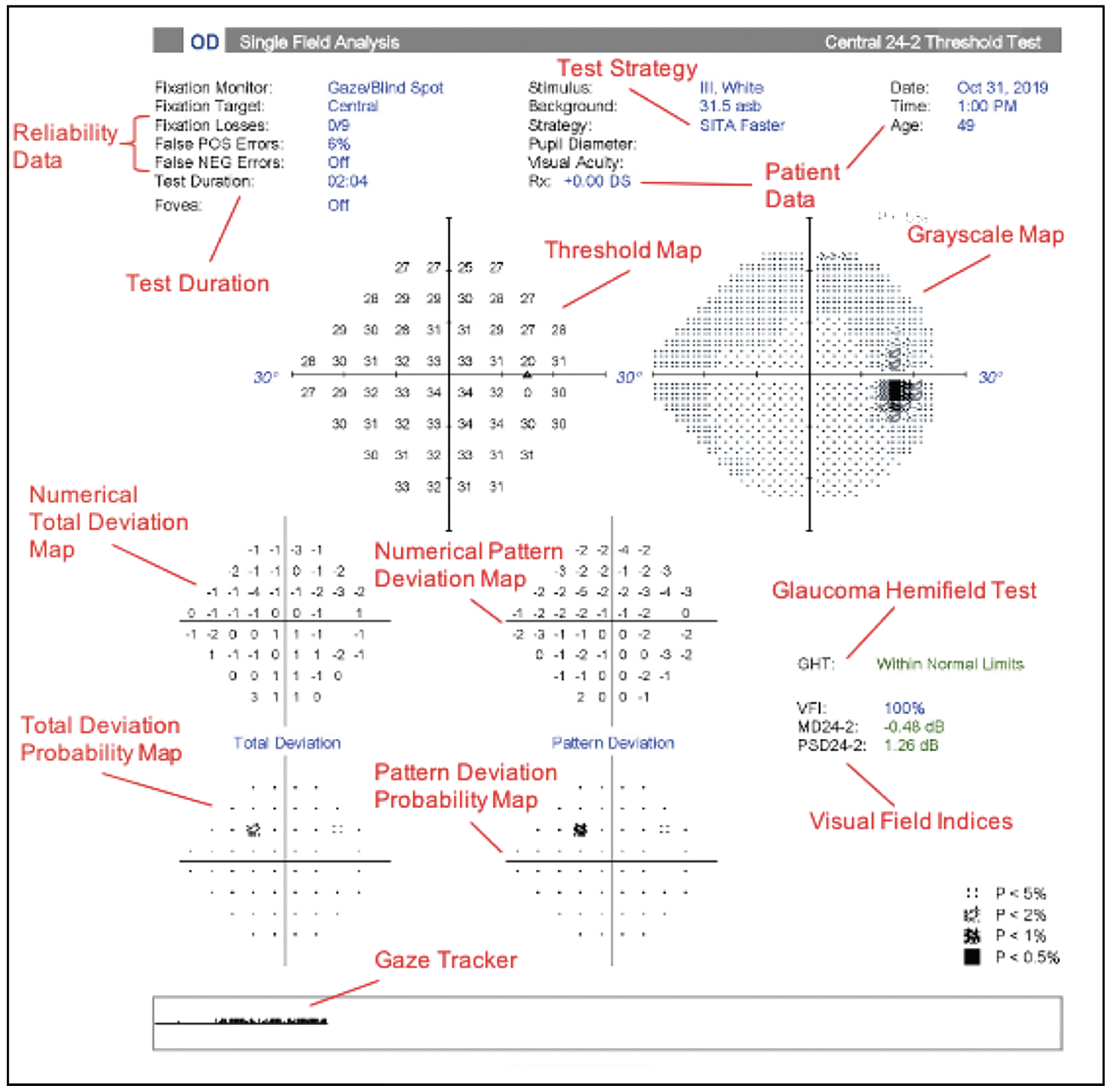
In addition to being difficult for some patients to take, the test results can be difficult to interpret. “If a patient has an obvious, dark, classic visual field defect that easily matches the appearance of the optic nerve in the OCT—so there’s a structure-function correlation—then it’s not that hard to interpret. The problem is that there are just so many nonspecific results. Many times, we get results that are kind of wishy-washy. There are the classically defined visual field defects that are typically glaucoma. But, many times, we just get scatterings and groupings of defects that don’t coalesce into a classic pattern, and then you’re left trying to decide if that’s a meaningful result or not. A lot of what we do is trying to filter out what’s real and what’s just random variation that you get from test to test. We must try to determine if it’s real change from glaucoma getting worse, or if it is sort of the intrinsic inaccuracy and variability built into the test itself. This is where it can be very tough to interpret a visual field in isolation. You really need the rest of the exam and all of the other data that you collect when you see the patient,” Dr. Eisengart explains.
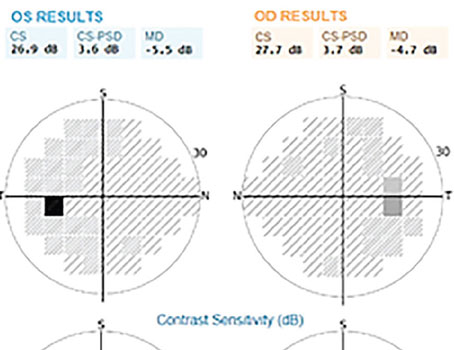
 |
| Figure 1. Humphrey visual field 30-2 test of the left eye of a patient with a nasal step and incomplete arcuate scotoma. The patient recently underwent a trabeculectomy for visual field loss progression. (All photos courtesy Kevin M. Miller, MD) |
Understanding the Visual Field
In addition to following progression, visual field tests can be used to stage the severity of glaucoma. “The ICD-10 coding classification has a well-described way to stage glaucoma based on the visual field. It defines mild disease as having no visual field deficits on a 24-2 Humphrey visual field, whereas any scotoma that’s not within 10 degrees of the central fixation and is only on one hemifield is moderate glaucoma, and any scotomas that are either in both superior and inferior hemifields or within 10 degrees of fixation are considered severe,” Dr. Seibold explains.
Unfortunately, visual fields are highly nonspecific. According to Dr. Eisengart, there are many false-positive results, and any visual field can be inaccurate. “If I see something on a visual field that looks worse, I need to either have that test repeated, or I need to have something corroborating it. So, for instance, let’s say I have a visual field that looks like the patient is developing a glaucomatous defect. If I’m going to believe that one test, I must have something to corroborate it, such as high pressure or the optic nerve changing. Or, I need to have the OCT changing in a way that’s consistent with the visual field change. If I don’t have another piece of evidence that points to the same thing, I will need to repeat the visual field later because I know that there’s a really high false-positive rate with these tests,” he says.
He adds that the visual field results need to be placed in the complete clinical context. “This includes the patient’s intraocular pressure, their adherence to medications, their optic nerve imaging like OCT, and the optic nerve exam,” Dr. Eisengart says. “Also, when I’m looking at visual fields and I’m trying to decide what to do, a small change might be significant in someone who’s 50 or 60 years old, but a small change with a mild visual field defect in someone who’s 85 might be something that can be safely monitored. So, we must look at the overall patient and his or her health to decide what to do. However, it’s an extremely important test because, besides visual acuity, it’s the only test that shows us what the patient sees. It’s extremely important for determining the function of the optic nerve, but we also must be careful when we interpret it because of its intrinsic unreliability.”
Kevin M. Miller, MD, who is in practice in Los Angeles, adds that visual fields are best at identifying progression in moderate to severe glaucoma. “Visual fields are terrible indicators of early disease,” he says. “You literally must lose half of your optic nerve to pressure damage before you start seeing the first defects, and the first defects in glaucoma are usually nasal step defects. If you look at the nasal side of the macula, you’ll see a blind spot that respects the horizontal midline. It can be above or below the horizontal midline, but that’s where you’ll find it. As it progresses, you’ll see the defect extends from that nasal step area either under or over the macula in an arcuate pattern. Then, the arcuate defect tends to just expand, while still respecting the midline. Then, when you have really advanced glaucoma, you see arcuate defects on both sides. The nasal portion of the disc is very resilient to pressure damage, and the macula fibers are also resilient to pressure damage. Those are the last two things to go.”
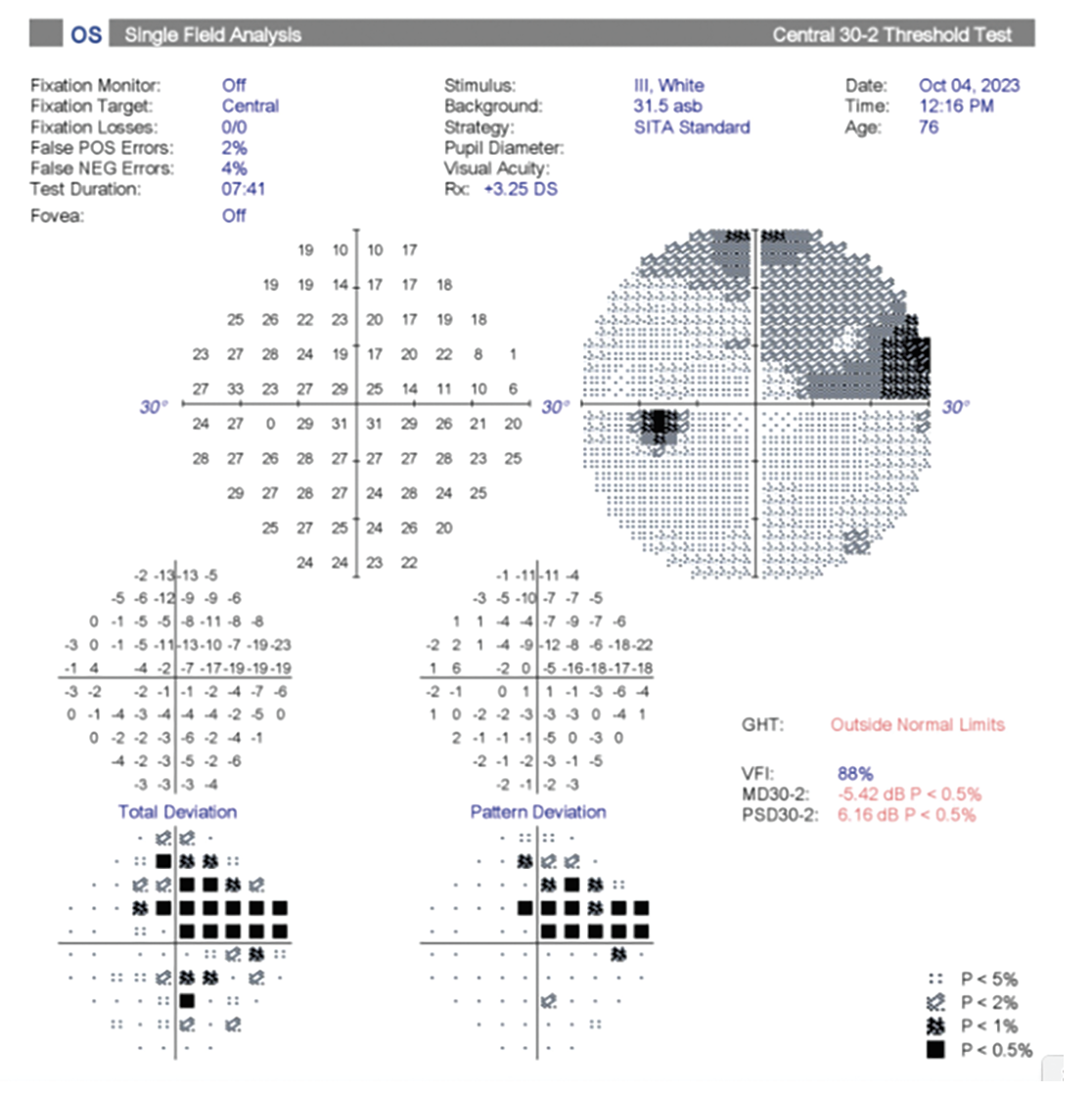
 |
| Figure 2. Understanding the Humphrey Visual Field. |
Limitations
According to James T. Murphy, MD, who is in practice in New Haven, Connecticut, the popular Humphrey Visual Field Analyzer has several limitations. First, the results are operator- and patient-dependent. “Technicians administer the visual fields, so it starts with planning and communicating what field you want to have done and how to do it. Additionally, fields are only as good as patients’ reliability, attention and endurance,” Dr. Murphy explains. His practice uses the Humphrey Visual Field Analyzer as well as Virtual Field and Olleyes, which are wearable virtual reality devices.
For an in-depth look at VR perimetry, see this issue’s cover story here. |
Dr. Miller agrees. “If a patient is daydreaming and clicking the button randomly or looking all around, then you’re going to get meaningless results,” he says. “I consider three things to determine whether the results are usable or reliable: One is fixation loss. You must have the fixation monitor turned on. But, if it’s turned on, then what happens is, every so often, the instrument will throw a light onto the perimeter where the blind spot is supposed to be. And if the patient is looking straight ahead, the patient should not see that light, no matter how bright it is. In a typical exam, the instrument will throw the light into the blind spot maybe 17 to 20 times, and then you can count how many times the patient saw the light. So, if they say they saw the light four out of 19 times, that means the patient wasn’t looking straight ahead more than 20 percent of the time. The other two things I look at when judging reliability are false-positives and false-negatives.”
According to Dr. Seibold, there are several parameters that can provide a sense of the reliability of the test. “In addition to looking at fixation losses, false-positives and false-negatives, we make sure that the prescription the technician puts into the machine is accurate for that patient. We also look at the pattern of any visual field deficits to make sure that it’s in a pattern that makes sense with the patient’s disease and that it correlates to where the patient has optic nerve damage. Looking at all of those things can help you gauge test reliability. However, even if all of those check out, and there’s no obvious parameter that looks off, we still repeat it,” he says.
According to Dr. Seibold, with glaucoma, changes are often observed on OCT first. “Most commonly in moderate glaucoma, you will see changes on OCT and visual field in concert with each other, so you’ll see an optic nerve change along with a visual field deficit that correlates,” he says. “That gives you a lot more confidence deciding if a change that you’re seeing is real. If only one of them is changing, I’m more suspicious that it could just be the natural variation or variability of that particular test, whether it’s an OCT change or a visual field change.”
Dr. Murphy notes that the clinician needs to be aware of sources for confounding field defects that are non-glaucomatous in nature. For example, dense nuclear sclerotic cataract, macular holes, and macular degeneration, and even a dense vitreous opacity can cause a central scotoma. Glaucomatous defect progression can be concealed by other defects from retinal disease, prior cerebrovascular accidents or defects caused by non-arteritic anterior ischemic optic neuropathy. “One must be able to use prior fields, structure-function correlation, and deduction to determine what is glaucomatous and what isn’t, as well as what is true progression and what is performance and reliability variability. During the pandemic, glaucoma specialists noticed that bulkier N95 masks were causing an inferior nasal step-like artifact. Unusual nasal or edge defects could represent a mask, or even the patient’s facial, eyelid or orbital anatomy or their positioning (or lack thereof) during the field testing. Patients with low test endurance can sometimes slouch away from the lens attached to the HFA. If his or her eye moves far enough away from that lens, and your office staff isn’t watching closely enough, then the lens rim becomes a source of artifact. Positioning is very important for Zeiss’ HFA product,” he says.
Tips for Success
Though commonly used perimeters have limitations, there are ways to improve the reliability of the results. For example, Dr. Murphy always reviews previous fields and decides what protocol to run. “I decide whether it’s going to be a 24-2, a 10-2 or a 24-2C with added central points near fixation,” he says. “I always have the foveal sensitivity turned on because during any field protocol it aids with maintaining fixation and can provide valuable information about the patient’s central field sensitivity. In contrast, some of the wearable devices test both eyes simultaneously in alternating fashion, which is especially helpful for patients who have one eye with poor vision or poor fixation. In these cases, the good eye helps keep the poorer eye fixated throughout the duration of testing.”
His practice sees patients who speak languages other than English, and he’s excited about the virtual test options that offer an extensive list of languages. “Both Olleyes and Virtual Field have an audio component that includes an earpiece that provides real-time audio feedback to help the patient test more reliably and accurately,” he says. “I serve a patient base that speaks a wide array of languages, and we simply could never have testing staff on hand to serve all these patients properly. I believe all patients deserve to have access to native language coaching for their diagnostics. Olleyes and Virtual Field can both provide needed translation and standardized, reliable coaching, and that can dramatically increase the diagnostic value of these tests.”
It can also be helpful to have multiple devices in your office. “We used to offer only Zeiss HFA,” says Dr. Murphy. “Some patients who are wheelchair-bound or who have limited neck, back, or spine mobility can have physical limitations that prevent them from being able to position properly for traditional tabletop perimetry. So, having an option that will allow you to serve all your patients regardless of their physical limitations has really added to our practice and those patients’ management.”
Drs. Eisengart, Miller, Murphy and Seibold have no financial interest in any of the products or companies mentioned in this article.