What was once science fiction is now literal virtual reality. Head-mounted VR perimeters are capable of conducting visual field tests and many other vision tests with minimal oversight from humans while producing promising results. Experts say VR visual fields have a bright future in screening, as an adjunctive instrument in the clinic and in the fast-approaching world of remote care. However, the technology still has a long way to go before it’s ready to substitute for standard automated perimetry.
We spoke with glaucoma specialists about the VR features they’re excited about, and what’s needed for this technology to take off in the clinic.
Virtual Reality Highlights
There’s a lot to look forward to in this new realm of computer-generated care, from faster thresholding to increased portability and ease of use. Here’s what glaucoma specialists have to say about it:
• Eye-tracking technology. One of the key features of many VR visual field devices is a type of technology that tracks the eyes’ movements with high precision (e.g., by one degree) and alters the test accordingly. “When you ask the patient to look at a central target, a machine [with eye-tracking technology] moves the whole visual field to expose the specific part of the retina that’s supposed to receive the light,” explains Reza M. Razeghinejad, MD, a glaucoma specialist at Wills Eye Hospital in Philadelphia. “If the eye movement is more than, say, 15 degrees off-center, the machine can send an alert to the patient, letting them know they need to refocus at the central target. We don’t have the ability to do that with the standard machine. Instead, the standard perimeter requires that a technician be in the room during the test to watch for fixation losses and notify the patient. How accurate is your technician, and for how long?”
• Foveal reflex-friendly. On a similar note, some VR perimeters don’t require fixation on a central target at all. Yvonne Ou, MD, an associate professor of ophthalmology who’s used the Vivid Vision Perimeter (Vivid Vision) in NIH-funded research at the University of California, San Francisco, says this device employs a testing strategy in which patients are asked to move their head or pointer, depending what they’re using, toward the fixation, stimulus or fixation task, and then perform the stimulus task. “Basically, every time the stimulus is presented,” she says, “the patient is looking at the stimulus [as opposed to only fixating on a central target], which I think makes the test easier to understand and perform for patients because they don’t need to suppress their desire to look at the stimulus.”
Virtual Reality Through Time1 • 1929: The Link Trainer commercial flight simulator by Edward Link, an electromechanical device mimicking movement during flight (e.g., turbulence), used later to train U.S. pilots in World War II. • 1935: Pygmalion’s Spectacles by Stanley G. Weinbaum, an early fictional account of virtual reality goggles. • 1939: View-Master stereoscope for virtual tourism. • 1950s: The arcade-style theater cabinet Sensorama by cinematographer Morton Heilig. • 1960: The Telesphere Mask by Morton Heilig, the first head-mounted VR display. • 1961: Headsight, the first head-mounted VR display with motion tracking and an early version of our modern head-mounted VR displays. |
• Patient comfort. Those familiar with VR perimeters seem to agree that patients find this approach more comfortable than sitting at the traditional standard automated perimeter. Dr. Razeghinejad, who’s used the VisuALL (Olleyes) in company-funded studies at Wills, says that with these headsets patients can sit in any position or take the test in an exam chair, waiting room chair or wheelchair.
“Many of our glaucoma patients have other comorbidities,” he says. “They may have back pain or neck pain or other issues that make it difficult to sit at the [standard] machine. Positioning can be a problem, because the patient’s forehead must go exactly against the bar and the chin in the chin cup. If the head is tilted, the results could differ from that of normal positioning.
“Virtual perimetry helps a lot with these patients,” he continues. “I’ve tried these devices for those who aren’t able to produce a reliable result with the standard machine. Some of my patients did better with these devices, which is a huge help for managing them.”
Alana L. Grajewski, MD, a glaucoma specialist in Miami and the medical director of Virtual
Vision Health, maker of the Virtual Vision perimeter, points out that these devices are particularly good for testing young children. “It’s very difficult to patch children, but these devices don’t require patching. Patients can’t tell which eye they’re looking out of. So, it’s quite easy in that regard.”
• Testing those with advanced glaucoma. “Another group that benefits from VR testing are those who have really advanced glaucoma with tiny central islands of vision,” Dr. Razeghinejad says. “It’s sometimes challenging to find the eyeline and positioning at the standard machine, but it seems easier to find the central fixation with these devices since it’s so much closer to the eye, and position isn’t critical.”
• User-friendly for patients. In addition to providing a comfortable testing environment, many VR perimeters also have built-in audio/visual features that instruct patients on how to take the test and how they’re performing. Based on her patients’ experiences and survey responses, Dr. Ou says the instructions are easy to understand and the test is easy to perform. “They prefer it over the Humphrey visual field, both in terms of comfort and decreased fatigue,” she says.
It helps if patients have some degree of familiarity with technology, but it’s not a requirement, Dr. Ou adds. “We did a study this past summer with participants whose primary language wasn’t English, to see if the test is translatable across different populations. With some additional training, these patients were also able to perform the test successfully. I think it’s definitely a test that’s broadly applicable to a lot of different situations and different patients.”
 |
|
Many virtual reality head-mounted perimeters, such as the VisuALL ETS (Olleyes), include common testing protocols such as 24-2, 10-2, 30-2, 24-2C, and other tests such as color vision, visual acuity, contrast sensitivity, pupillometry and more. |
• A potential time saver. “When you’re checking perimetry virtually, you don’t need to move the patient around the clinic, so it saves a lot of time for the physician,” says Dr. Razeghinejad.
Additionally, the in-headset training minimizes the need for a technician to administer the test, freeing up that time.
• Affordability. VR perimeters vary in price but are relatively inexpensive. “Eventually, for patients to have these in their home, [the VR perimeters] are going to be what I call device agnostic, meaning there’s going to be software and not really the device itself, in order for it to be affordable. It’ll likely be off-the-shelf devices.”
• Home testing. In the same vein, experts say that one future use of VR perimetry lies in home testing. “It’ll be exciting for patients to be able to test themselves, and the doctor will be able to see [the results] from wherever they are,” Dr. Grajewski says.
• Screening in remote areas. The portability of these VR headsets makes them ideal for use in remote areas and regions without access to standard visual field testing. Dr. Razeghinejad says future additions to the headsets will boost their screening utility even more. “I think these devices are going to change a lot in the coming years. They track not only the visual field, but many can also check visual acuity, color vision and pupil reaction. Some are working on checking eye motility. That’s going to be really helpful. In the future, adding fundus imaging will be fantastic.”
What’s Missing?
Though head-mounted VR perimetry presents many new and exciting opportunities, there’s still a considerable amount of groundwork that needs to be done and questions that need answers before they’re ready for more widespread adoption. Chiefly among the obstacles is a lack of a normative database since this perimetry technology in its current form is so new.
Glaucoma specialist James C. Tsai, MD, MBA, of New York Eye and Ear Infirmary of Mount Sinai in New York, says that more research is needed. “We need new publications that work out the correlation between the results on the VR visual field and traditional automated perimetry,” he says.
“We know that these devices are comparable in many ways, but we don’t have as much data as the gold standard,” Dr. Grajewski says. She says the outlook is hopeful for overcoming this challenge. “Over time, because these devices are gaining in popularity, we’ll have that data. In fact, we have more data now than three months ago.”
Virtual Reality Visual Field Devices Here are some of the currently available VR perimeters on the market: • VisuALL (Olleyes). Olleyes says its VisuALL perimeters provide comfortable, comprehensive testing while the multilingual AI assistant monitors patients to promote clinician multitasking. According to the company, the devices are disinfectable, suitable for multiple age groups and positioning needs, feature a 4K display and are compact and portable. The perimeters are part of a three-pronged virtual reality platform (VRP) suite which also consists of a web-based application and a HIPAA-compliant cloud for provider-patient interaction. VisuALL ETS and S Models are available. The new VisuALL VRP Choice package includes a headset and a suite of the company’s customizable testing options such as AVA-fast 24-2 and 30-2, pediatric protocols, supra threshold testing and more. To learn more, visit olleyes.com. • Vivid Vision Perimeter (Vivid Vision).Vivid Vision Perimetry or VVP head-mounted device includes a variety of testing protocols such as 24-2, 10-2 and 30-2-M, along with the Ladybug protocols. Clinicians can also create custom visual field tests using their own csv. The company says that the VVP prompts natural fixation and also allows patients to guess as often they’d like without biasing their results thanks to the device’s advanced psychological approach. The device is suitable for office and home-based use for more frequent monitoring. To learn more, visit perimetry.seevividly.com. • Virtual Vision (Virtual Vision Health). Virtual Vision Health’s Virtual Eye device features 256-bit encryption, printable and EHR-compatible examination records and cloud-based software for reviewing or conducting tests remotely. It comes with audio instruction to replace technician monitoring and is easily sanitized, according to the company. The company also says the Virtual Eye device’s testing modalities, accuracy and repeatability are comparable to standard automated perimetry. Test patterns include 5-2, 10-2, 24-2, 24-2C and 30-2; full field 120; superior 64 and 36 (ptosis); Esterman; and color sensitivity; along with thresholding strategies and stimulus sizes III, V (I-VI). The Virtual Eye’s visual field reports include progression analysis, raw threshold values, glaucoma hemifield test, mean deviation, pattern standard deviation, visual field index and reliability indices. To learn more, visit virtualvision.health. • Easyfield VR (Oculus). Easyfield VR is a mobile visual field analyzer and vision tester headset. Oculus says that in addition to improving practice flow and reducing technician time, this device doesn’t rely on an internet connection, uses continuous eye tracking, includes English and Spanish audio support, integrates with all Oculus diagnostic devices and allows patients to test quickly and comfortably. Tests include 45-second visual field screening; under three-minute thresholds 10-2, 24-2, 30-2; progression analysis with a familiar printout; ptosis and Esterman visual fields; as well as testing for color vision, stereoacuity and contrast sensitivity. To learn more, visit oculus.de/us/products/easyfield-vr. • Smart System VR Headset (M&S Technologies). M&S Technologies’ Smart System VR headset with SMARTracker2 eye tracking software has quick screening protocols (a 45-second QuickScreen test) and full threshold testing in under three minutes per eye. The company says the device gives audio and visual cues to both technician and patient, works without an internet connection and provides immediately exportable results to the practice’s EMR. The lightweight headset is easily portable and compact, M&S says. A host of tests are built in, including 10-2, 24-2 and 30-2 thresholding; supra threshold, ptosis and Esterman; color vision, stereo testing and contrast sensitivity. M&S says they offer live, immediate technical support. To learn more, visit mstech-eyes.com/vr-headset. • VF3 (Virtual Field). Virtual Field says its head-mounted perimeters are user-friendly and allow for patients to sit where they’re most comfortable, whether at a table or in the exam chair. The perimeter uses CPT codes 92081, 92082, 92083 and 95919. Built-in progression analysis software enables clinicians to track visual field loss over time. The VF3 includes visual field testing and color vision screening. The VF3 Pro includes visual fields, color vision, pupillometry, active eye tracking and kinetic visual fields (Goldmann perimetry). To learn more, visit virtualfield.io. • VF2000 (MicroMedical Devices). The VR2000 VR headsets provide full and fast threshold testing as well as a number of other vision screenings, a 4K display and the company’s Active Eye Tracking technology in the VF2000 NEO model. The devices can be used without a Wi-Fi connection, are ADA compliant and also include multi-language instruction in the self-guided patient testing interface. The company says the available tests and screenings satisfy CPT codes 92081, 92082, 92083 and 92283. Other available models include the VF2000 G2. To learn more, go to micromedinc.com. • Advanced Vision Analyzer (Elisar Vision Technology). Elisar says its AVA Advanced Vision Analyzer is simple to use and includes advanced infrared tracking technology that automatically corrects for fixation loss. It includes test patterns 24-2, 30-2 and 10-2 and screening strategies, full threshold, Elisar Standard and Elisar Fast. The AVA enables multiple patient testing positions, including reclined positioning. The company also notes that the AVA generates a patient-friendly version of the visual field report to help the clinician better explain the diagnosis. Additionally, the cloud-based software updates automatically. To learn more, visit elisar.com. • VirtualEye Perimeter (BioFormatix). This head-mounted perimeter performs 24-2 visual field testing using a manual (subjective) mode, where patient response is recorded via mouse click and a visual grasp (objective) mode, where an eye tracker registers evidence of target acquisition by sensing changes in gaze. The company says this gaze-tracking feature increases test reliability and accuracy while enabling hands-free operation. Additionally, BioFormatix says its technology can be reconfigured to accommodate emerging and future testing scenarios. The headset includes a display and eye-tracking camera as well as space for a trial lens and an infrared illuminator. It’s compatible with Windows computers. To learn more, visit bioformatix.com/perimetry.html. • nGoggle (NGoggle). The nGoggle is a portable, brain-based, head-mounted device for detection of glaucomatous field loss with electrophysiological sensors, mA current stimulators and cloud-based software. Wireless electroencephalography measures brain activity and eye-brain-visual field communication. To learn more, visit ngoggle.com. |
Practical Considerations for VR Integration
Rapid innovation is both a blessing and curse. Since glaucoma diagnosis relies on longitudinal data, the stability of the visual field testing platform is key. “The standard automated Humphrey and Octopus visual fields are pretty stable platforms,” says Dr. Tsai. “There may be some slight changes in, let’s say, software or algorithms, but they’re steady.
“It’d be a lot easier to use VR visual fields if someone were to develop a program that either takes the data we’ve garnered over the years [on SAP] and translates it into what we’d see in the VR visual field data, or vice versa. If you were starting all your patients on VR visual fields, then it’d be very simple. You’d follow them with the same platform longitudinally.”
Dr. Razeghinejad points out that most of the VR perimeters have their own thresholding algorithms. “The instruments aren’t talking to each other,” he says. “You may get the same pattern of visual field loss, but the numbers and depths may not be exactly the same.”
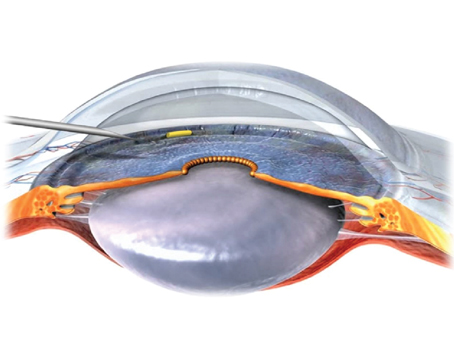
 |
|
With virtual reality testing, patients can test in a comfortable position in various locations such as a waiting room or exam chair. Eye-tracking software and audio instructions minimize the need for a technician to administer and monitor the test. Additionally, several companies offer test instructions in multiple languages. |
Though VR visual field data and SAP data aren’t interchangeable, Dr. Grajewski says VR perimeters could increase the frequency of monitoring if used alongside SAP. “Right now, patients come in every four months or every six months for a visual field, but wouldn’t it be nice if we were monitoring every month? If you saw something grossly different [on VR perimetry] you might repeat it with that device, and if it was still grossly different, you’d bring the patient in to get their baseline [on SAP] and compare that to their previous SAP results. There’s good data that indicates that following patients more frequently leads to better care.
“At the moment, VR visual fields aren’t near the sophistication of Humphrey or Octopus, which have years and years of investigation and standardization with respect to the algorithms,” Dr. Grajewski acknowledges. “Clinicians are always going to make major decisions based on progression analysis and SAP. There will be times when VR is preferable and there will be times when you’ll use SAP. Will the technology of these VR devices eventually catch up? Possibly. A lot of work is going into them, but we need more time and we need more data.”
She adds that some patients may get better test reliability outside of the office. “Sometimes what you lose in sensitivity you’ll pick up in the ability of a patient to take the test better,” she says. “That’s one of the things I think all of us have seen with the head-mounted devices. But when you really want to see an area, you’ll use the instrument with years and years of robust data. With VR visual fields, you could decide if somebody was worse or needs to come in, but I’d say most glaucoma specialists are still waiting for more information on monitoring with VR devices. From a screening point of view, they’re fabulous.”
Screening and Monitoring
The glaucoma monitoring capabilities of VR perimeters are still developing. Dr. Ou says that one of the barriers to incorporation right now is that clinicians want a test that can monitor glaucoma progression. “There’s still quite a bit of work to be done on the clinical research side to definitively demonstrate that [VR devices’] test-retest reliability is sufficient and that they’re sensitive enough to detect glaucoma progression. To my knowledge, the field hasn’t demonstrated that these tests can be used for monitoring. I do think that screening would be a great situation for portable visual fields or VR visual fields. We’ll need to establish outcome measures for screening: What is a failed screening test? What is a successful screening test? How do we determine the cutoff for a pass/fail?”
Dr. Tsai states that VR visual field headsets would work very well in a population-health model. “In a population-health model, you’re not paid per test, but instead you’re aiming for tests that are cost-effective and easily done at home, at community centers, outside of doctors’ offices, and tests that don’t require skilled personnel. If we move forward to that type of health-care environment—less fee-for-service—then I see these VR tests really taking off.”
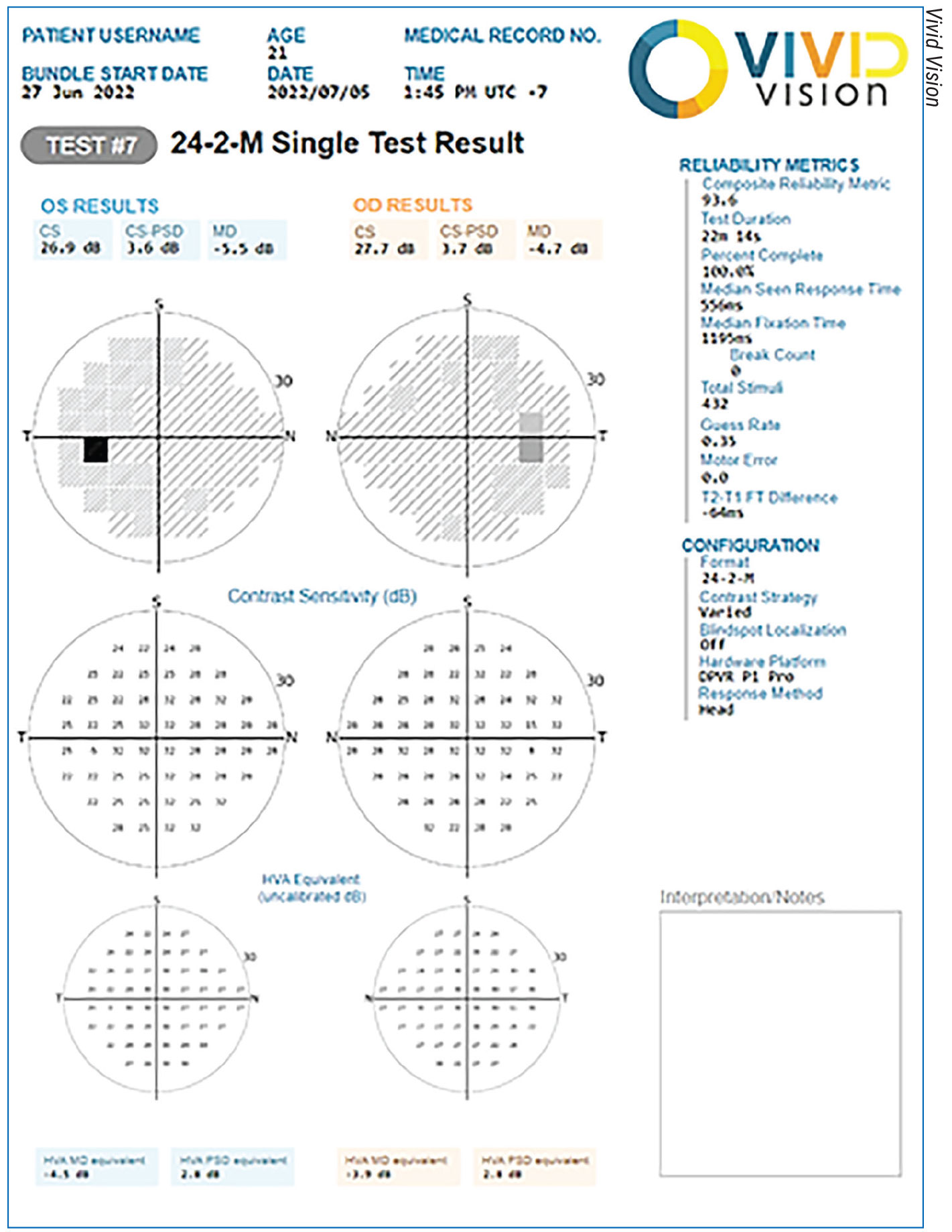 |
|
Most virtual reality perimeters include readouts that closely resemble the ones physicians are already familiar with from standard automated perimetry. |
He says a primary care office could be a good setting for such a test. “Patients with a family history of glaucoma or those who’ve been told they have elevated eye pressure could come in and be readily tested in primary care offices, rather than sending the patient for a much more costly comprehensive eye exam,” he says. “If we paired VR visual field headsets with some AI-guided analysis of the optic nerve and a portable way to measure eye pressure, we’d have three very important test points. That would really help define which patients should be seen by an ophthalmologist/glaucoma specialist and which patients might be able to be followed in their primary care office for yearly exams because they’re at very low risk for developing glaucoma.”
Dr. Tsai is the director of the newly formed Center for Ophthalmic Artificial Intelligence and Human Health at Mount Sinai. “As we embrace either AI-guided technology and/or technologies such as VR visual field headsets that rely on AI-based software, we’ll be able to validate these technologies and demonstrate their clinical usefulness in many different models of care, not just population health, even though that’s what we’re leaning towards because we see there could be a real benefit,” he says.
Reimbursement
“In glaucoma practice, we believe that if we can get reliable visual fields on a consistent basis over time, we have a better chance of determining whether a patient is truly progressing or remaining stable,” says Dr. Tsai. “Currently, the payment system model doesn’t readily reimburse for very frequently performed visual fields.
“One of the challenges of glaucoma care is that there’s got to be a way to get compensated for the care of patients,” he continues. “One of those ways is the traditional visual field, with a CPT code that’s been proven. With these new technologies, there are questions about what the reimbursement will be, how it compares to what we get compensated for traditional visual fields, and the fact that we may still need to perform traditional visual field testing to ensure we’re not missing anything.
“Computer-based visual field testing has been around for decades,” he adds, “but there was very low adoption of that, primarily because it’s difficult to figure out how to monetize or make it attractive for practices to rely upon.”
Held to the Standard of Care
Widespread adoption of VR visual fields by the majority of practitioners is slow going. “The challenge with medicine is that we can embrace innovation, but we’re always held to a traditional standard of care,” Dr. Tsai explains. “Standard of care tends to be less innovative because it’s had to be tested and validated over many years. That’s what we rely upon. Even doctors who want to move forward with these innovative technologies are still held back by concerns such as, ‘What if I rely on this VR visual field to tell me that this patient is stable, when in fact they’re not stable? What if I miss something?’ or ‘What if this VR visual field tells me the patient’s progressed when they haven’t?’ Those are all questions I believe clinicians have that we’re very interested in exploring.
“Novel technology is great,” he continues. “Anything that makes it easier for patients to receive top-notch care is fantastic. But we need to know that the companies marketing these devices have done enough background research that we’re convinced the technology is reliable and has been validated and that we aren’t doing patients any harm by relying on these technologies. That said, I hope we’ll be able to figure out in the near future how to incorporate VR visual fields into our normal workflow of glaucoma patients.”
Dr. Razeghinejad has conducted research for Olleyes.
Dr. Tsai is a consultant for AI Nexus Healthcare, Eyenovia, ReNet X Bio and Smartlens.
Dr. Grajewski is the medical director of Virtual Vision Health and has a financial interest in the company.
Dr. Ou has no related financial interests.
1. History of Virtual Reality. Virtual Reality Society. vrs.org.uk. Accessed January 11, 2024.