Visual field testing remains an essential part of detecting and monitoring the progression of glaucoma, so it should be no surprise that new product options for performing this type of testing continue to proliferate, while existing options continue to be refined. Currently, more than 14 companies offer an in-office perimeter, using different algorithms to detect glaucomatous defects and analyze the data. In addition, with the advent of head-mounted virtual perimetry and tablet-based perimetry, a long list of additional companies and testing approaches have entered the picture.
All of this technology is helping to make the doctor’s job easier and potentially make results more accurate. “Today’s machines incorporate a lot of technology that not only helps us collect the data but also helps us assess whether the disease is getting worse and whether the test was reliable,” notes Steven L. Mansberger, MD, MPH, Chenoweth Chair of Ophthalmology and director of the Glaucoma Services at the Legacy Devers Eye Institute in Portland, Oregon. “That’s significant, because we’re all very busy.”
Here, to help make sense of the increasing number of options, multiple surgeons and researchers share their experiences with these technologies. In particular, given the popularity of the Zeiss Humphrey perimeter in the United States, they focus on the different SITA algorithms and when it makes sense to use each of them.
Is Faster Better?
 |
|
Patients are notoriously unhappy about taking visual field tests. The current faster versions are easier on patients, but are slightly less accurate. This may permit more frequent testing, however. |
One of the questions facing clinicians who use the Humphrey perimeter is, which version of SITA (Swedish Interactive Threshold Algorithm) testing should they use: SITA Standard, SITA Fast or SITA Faster? There are also questions centering around the recently available SITA 24-2C test, which checks additional points in the visual field.
“SITA Standard has been well-proven to be very reliable, because it double-checks the sensitivity at each spot,” Dr. Mansberger explains. “In contrast, SITA Fast and Faster do not. As a result, we can do visual fields in less time with SITA Fast and SITA Faster, but we have to test patients more often to ensure reliable results.”
Stuart K. Gardiner, PhD, a senior scientist at Devers Eye Institute in Portland, Oregon, who has contributed to the development of visual field software, says the differences between the two faster options—SITA Fast and SITA Faster—are relatively small. “They made a few tweaks to get from SITA Fast to SITA Faster that are fairly inconsequential for patient care,” he notes. “It uses a slightly different way to assess variability; it’s quicker because it’s not based as much on catch trials. I don’t see a big reason not to switch from SITA Fast to SITA Faster, for clinical purposes.”
Of course, the length of time spent taking a visual field test is partly determined by the patient. In addition to the level of patient cooperation, Jonathan S. Myers, MD, chief of the Glaucoma Service at Wills Eye Hospital and a professor of ophthalmology at Thomas Jefferson University’s Sidney Kimmel Medical College in Philadelphia, points out that how quickly a visual field test is completed is affected by the status of the patient’s disease. “SITA Faster is faster than SITA or SITA Fast, but some of the biggest time gains are for patients with moderate to advanced glaucoma,” he notes. “They often have the slowest fields with SITA standard.”
Dr. Myers notes relevant data from two studies. One study done at five centers tested one eye each of 126 patients either diagnosed with glaucoma or considered glaucoma suspects. The patients were tested with SITA Standard, SITA Fast and SITA Faster at each of two visits. The data showed that SITA Faster gave results very similar to those of SITA Fast, but with slight differences compared to SITA Standard.1
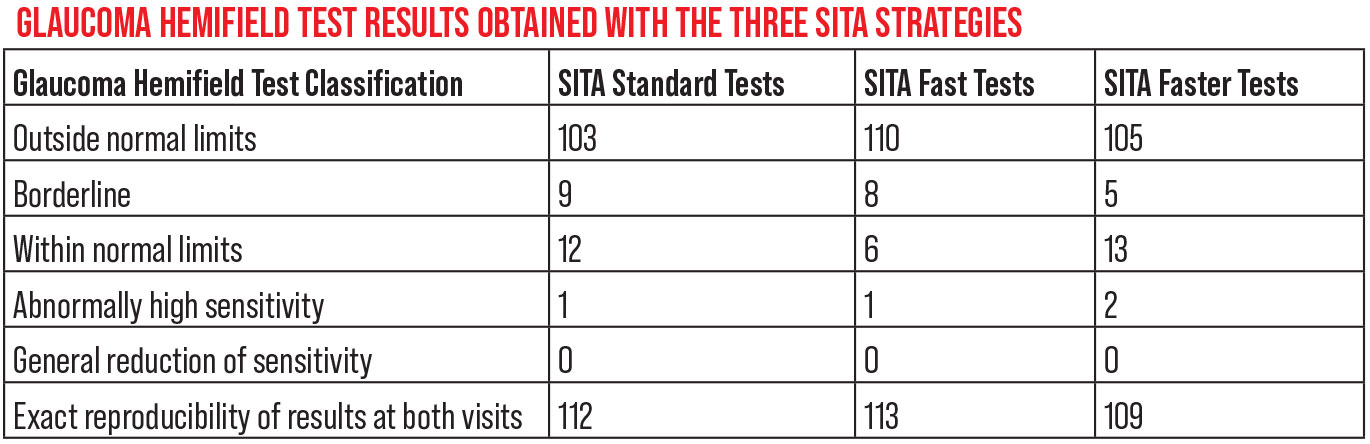 |
A 2019 study compared the three SITA speeds, analyzing results from 125 patients (51 percent female, mean age 67 years). Mean test times were 369.5 seconds for SITA Standard, 247 seconds for SITA Fast and 171.9 seconds for SITA Faster (p<0.001).1 |
The authors of this study point out two key technical differences between SITA and SITA Faster:
- A key part of the test is conducting a threshold evaluation to determine an appropriate stimulus intensity for the patient, which takes time. The early SITA programs started testing at 25 dB, a value inherited from the Humphrey full threshold test, which was created before researchers had any knowledge of normal age-corrected sensitivity values. The newer versions of the test save time by starting at or near the age-corrected normal threshold value.
- The early tests assessed the patient’s fixation by projecting stimuli into the blind spot to see if the patient responded. (Those machines had no way to perform optical or video surveillance of the patient’s gaze.) Using this approach has several flaws: 1) It adds time to the length of the test; 2) it can only check fixation periodically; 3) the blind spot may be inaccurately located, causing the machine to report poor fixation when fixation was actually good; and 4) the patient’s visual field status is known to have a big impact on the accuracy of this approach. With gaze tracking technology now available, the developers of SITA Fast and Faster felt that this was a good substitute for the blind spot fixation assessment method—especially when combined with observations by the technician running the test.
The other study noted by Dr. Myers was conducted at the Wilmer Eye Institute.2 This study tested 421 patients twice with SITA Standard and once with SITA Faster (in that order), with a mean time between tests of 13.9 months. They looked at the differences between the first two tests (both done with SITA Standard) and the differences between the last two (SITA Standard vs. SITA Faster). They compared the results in three groups: patients with mild, moderate and advanced disease severity. The study found that converting from SITA Standard to SITA Faster led to similar visual field performance in patients with mild glaucoma, but resulted in higher mean deviation values in patients with moderate or advanced glaucoma.
Making the Switch
“Many of these technological differences are smart choices,” notes Dr. Myers. “However, some clinicians may not be happy about another one of them: The new tests don’t do false-negative trials. In these trials, the machine shows a stimulus the patient should see; if the patient doesn’t see it, it’s a sign that the patient may be distracted or tired. Not doing these trials saves time, but many of us look for a high false-negative score to warn us that a test result may not be representative of the patient’s best visual result.”
Dr. Myers says he has limited experience with SITA Faster because his practice primarily uses SITA Fast when using the Humphrey machine; in addition, some patients at his other offices are tested on Haag-Streit’s Octopus perimeter. Nevertheless, he says that the switch to SITA Faster reminds him of the switch from full threshold to SITA several years ago. “A lot of patients with moderate to advanced disease looked better when tested with the SITA algorithm,” he recalls. “At the time, we debated whether this was because it was a faster test, so patients didn’t get as fatigued, or because the thresholding algorithm was substantially different.
“The change from SITA to SITA Fast or Faster seems similar,” he says. “The new test is quicker, and many patients look better on the new test. Nevertheless, if a patient is stable, I think you can switch and re-establish a baseline. But you have to be careful if you think a patient is progressing and you’re considering advancing therapy if the change is confirmed. That’s not the time to switch testing algorithms.”
Some clinicians say they’ve already adopted the SITA Faster algorithm as their primary testing algorithm in the clinic, including David Fleischman, MD, MS, FACS, an associate professor in the Department of Ophthalmology at the University of North Carolina at Chapel Hill, and perioperative medical director at UNC Hillsborough. “The number of complaints about visual fields that I used to hear from my patients when I started with SITA Standard was reduced considerably when I adopted SITA Fast. Since switching to SITA Faster those complaints have become rare.
“I acknowledge that SITA Standard is considered the gold standard,” he continues. “However, I was tired of having to inform my patients that they didn’t perform their test reliably and that they’d need to repeat it. Repeating these tests takes up considerable staff time and effort in clinic, and the patient feels like a failure. I can eat the increase in variability that comes with SITA Faster in exchange for the patient feeling better about the testing, and I have no qualms repeating this test frequently over the course of a year. That helps me gauge the status of a field—and just as important, the speed of progression.”
The Patient Factor
As already noted, a big reason for switching to a faster testing strategy is that patients find most visual field tests difficult to tolerate—and the longer the test, the less they like it.
Dr. Myers confirms that the faster test is definitely appreciated by patients, making it feasible to test more often. “That’s part of the reason we switched to the Octopus perimeter in some of our offices,” he notes. “We found that the TOP (tendency oriented perimetry) algorithm used in the Octopus was substantially faster than SITA Standard or SITA Fast. Our patients really appreciate that, and they’re more willing to take the test. We thought it was worth losing a little bit of accuracy to gain the option of doing the test more often.”
Dr. Gardiner points out, however, that the time savings from using the faster test aren’t actually as dramatic as they may seem at first. “SITA Faster brings the test time down from five or six minutes to two or three minutes, but the time it takes to set up, get the patient’s information into the instrument and so forth, doesn’t change,” he says. “For that reason, switching to SITA Faster might only shorten the entire process from 25 minutes to 20 minutes for both eyes. So in terms of workflow in the clinic, it’s not as dramatic an improvement as it might sound. It’s certainly not cutting the overall testing time in half.”
So, how should a clinician decide which test to use for a new patient? “When choosing a test for a new patient, I’d consider a couple of factors,” says Dr. Gardiner. “For one thing, some patients can tolerate and give good results with a longer test. However, if someone has trouble concentrating for five minutes but can manage two minutes, then it’s worth doing a shorter test.
“Another factor is that, if someone already has vision loss, or you think there’s a good chance that they’re getting worse rapidly, then you need to have the most accurate information possible,” he continues. “It’s worth taking the time to do the longer test to get more accurate information on those patients. That may be fine with the patient, because if a patient has obvious vision loss or is getting worse fairly quickly, it’s much easier to persuade them that it’s worth doing a six-minute test instead of a two-minute test. Conversely, if a patient is normal or has very early loss, and your clinical opinion is that it’s less urgent, the shorter test might be acceptable.”
“I’d say that for early glaucoma patients and suspects, using a test that’s faster is probably OK,” Dr. Mansberger says. “If you have someone who’s older and has more severe glaucoma—someone who has more variability to begin with in terms of visual field testing—then it might be better to use a standard visual field algorithm like SITA Standard. You don’t want to give an older patient a shorter test that might produce an abnormal result, because you might end up thinking they’re getting worse when they just had a bad day.”
The 24-2C Test
The SITA 24-2C test expands the testing range of the SITA Faster test to include some central visual field locations, normally not tested except by a separate test such as the 10-2 test. Dr. Gardiner says that he was one of a number of people who worked on developing the 24-2C test. “The grid that’s used in the standard 24-2 test isn’t designed to pick up localized defects in the center of the visual field,” he explains. “The usual way to compensate for that is by giving the 10-2 test; it has good coverage of the center of the field, but no coverage in the periphery. The 24-2C was designed to be a compromise that checks all the same locations as the 24-2, plus a few extra central ones from the 10-2 test. The idea was to get more complete coverage without having to spend the time it takes to do two tests.
“A group of experts helped the company decide which central locations to add to the grid,” he continues. “The locations we chose weren’t random—they were the ones most likely to pick up glaucomatous defects that were being missed with the 24-2 test. Of course, if we added every central location from the 10-2, the test would take a lot longer, and if a test takes too long, then the patients get tired and the results become less reliable.
“At the moment, only the SITA Faster algorithm on the Humphrey can run the 24-2C test grid,” he adds. “Of course, adding the extra central points makes the test take a little bit longer than the original SITA Faster test—but only a little. It still takes less time than doing the SITA Standard test. In any case, I think it’s really important to test the extra locations in the central part of the field, because they affect activities of daily living.”
Comparing Algorithms A number of different algorithms beside SITA are available for use in visual field testing. Stuart K. Gardiner, PhD, a senior scientist at Devers Eye Institute in Portland, Oregon—who has worked with many of them—says that the GATE (German Adaptive Threshold Estimation) algorithm, available on the Octopus perimeter, is similar to SITA. “It’s designed for clinical care,” he notes. “One notable difference is that the Octopus perimeter has included more central locations in its test grid for many years. “All of these programs initially try to come up with a sensitivity estimate at each location,” he explains. “Once that’s done, both SITA Standard and GATE apply a spatial filter that incorporates information from neighboring locations to reduce the data noise a bit. That’s good for clinical care but less ideal for research purposes, because we need to know what the original estimates were for each location. “That’s where an algorithm like ZEST (zippy estimation by sequential testing) comes in,” he continues. “ZEST is open-source, so there are no proprietary secrets; we know exactly how it works. Unlike the commercial algorithms, ZEST doesn’t do any post-processing of the measured data. That makes it more predictable. The tradeoff is that it doesn’t reduce the variability of the results as much as the more widely used commercial algorithms do. “I believe ZEST is mostly being used for research, and I don’t think it would offer any clinical advantage over SITA or GATE,” he says. “In fact, I believe that adding extra central testing locations, as the SITA Faster 24-2C or Octopus GATE algorithms do, will have much more of an impact on clinical care than the differences between the testing algorithms.” Another algorithm is TOP (tendency oriented perimetry), available on the Octopus instrument. “TOP takes spatial filtering to an extreme, trying to shorten test time as much as possible by using information from neighboring locations,” Dr. Gardiner explains. “It makes it a much faster test, but you lose a lot of localized information. The idea is similar to SITA Faster, although the algorithms aren’t identical.” —CK |
Dr. Myers says he’s read a number of studies evaluating the potential pros and cons of adding some central points to the 24-2 test. “The literature makes it clear that while the 24-2C may pick up some paracentral defects that you might otherwise miss, there are still a lot of paracentral defects that it won’t pick up,” he explains.3 “For example, most clinicians won’t change treatment because we see one isolated abnormal point in a field. We assume it’s a mild depression and we don’t make much out of it, because patients don’t test perfectly. Most of us require two or three contiguous abnormal points on the field to feel that something significant may be happening.
“Two studies show a challenge with the 24-2C [relating to this],” he continues. “Because it doesn’t have as many paracentral points, it often won’t show two or three abnormal points next to each other—where the 10-2 would.4,5 We’re not likely to retest everyone who has one abnormal paracentral point on the 24-2C, and as a result, we could miss a lot of people who have paracentral defects—people we wouldn’t miss if we tested with the 10-2. Of course, this doesn’t mean that the 24-2C test doesn’t add value; it just means that the value is limited. So if you’re really concerned about central defects, the 10-2 is a more definitive test.”
So which test should you use for the majority of your patients? “From a practical standpoint, you want to choose a test with an algorithm that your technicians can follow through on easily and quickly,” Dr. Mansberger says. “The 24-2C, which is only available on the HFA3, uses the same algorithm as SITA Faster but also checks the central visual field. I suspect that most doctors who have the HFA3 would choose the 24-2C for most patients, because it tests more locations.
“However, if a patient is progressing, you might move that patient from the 24-2C to a SITA Standard 24-2, just to get lower variability and be able to follow them more carefully,” he adds. “If a patient only has central visual field left, you’d move them to a 10-2 visual field. For patients with lots of variability and lots of loss, but more than just a central island of vision left, you might switch to a size 5 stimulus. This will allow you to get some information from areas with a sensitivity worse than 19 dB.”
Dr. Mansberger says he does like to get a 10-2 field on every glaucoma patient. “This gives us a sense of their central visual field sensitivity,” he explains. “Then, we repeat it every one or two years to see if there’s a change in that area. Of course, the patients who should be tested regularly with a 10-2 test are those with visual field loss close to fixation. In that case, you may want to do 10-2 testing exclusively. If the patient only has vision left in the center, why spend time testing parts of the visual field that are already gone?”
Portable Perimetry
There are two new approaches to perimetry that are portable: virtual reality headsets and perimetry done on computer tablets.
“In contrast to the massive, expensive instruments used in the clinic, tablet perimeters are designed for use at home, especially for frequent testing,” notes Dr. Gardiner. “However, they’re not as repeatable, because the test-taking conditions aren’t as controlled. You have to do more frequent testing to make up for that, but patients can do more frequent testing quite easily.
“There are two primary problems with tablet perimetry,” he continues. “The biggest problem I see is that the room lighting can make a big difference in your results. If you do the test in a brightly lit room, you won’t get the same result as if you do it in a dimly lit room. The second problem is that you have to keep the tablet at a constant distance from your eyes. That’s certainly possible, but how well it’s done in the real world is an open question.
“For those two reasons, the results of perimetry done using a tablet will be quite a lot more variable,” he concludes. “However, if you have a patient that you trust to do it once a week with the setup the way you want it to be, you can get fantastic data from them. That would more than make up for the variability.”
Head-mounted Virtual Reality
A number of head-mounted perimeters are now available, including Vivid Vision, the HERU perimeter, the VisuAll (Olleyes), the VirtualEye Perimeter (BioFormatix), the PalmScan VF2000 (MicroMedical), the eCloud Perimeter (Elisar), the IMO perimeter (Crewt Medical Systems), and the Toronto Portable Perimeter (VEM Medical Technologies). “A number of glaucoma clinics are already using these,” notes Dr.
Mansberger. “The technology is generally not too expensive; it’s around $10,000 for a device, compared to a visual field machine which might cost $30,000.”
Dr. Gardiner points out that the virtual reality headset perimeters provide more repeatable data than tablets because they block out almost all of the outside light. “Also, the viewing distance is kept constant,” he notes.
In-office Product Alternatives | |
Although most American ophthalmology practices currently use a Humphrey perimeter, quite a few rely on the Octopus perimeter (Haag-Streit). Other current perimetry options include:
| Many of the competitors appear to be good at their job. A recent prospective, case-control study (sponsored by Optopol) compared SITA Fast to Optopol’s ZETA Fast in 26 glaucoma patients and 26 controls.8 David Fleischman, MD, MS, FACS, an associate professor in the Department of Ophthalmology at the University of North Carolina at Chapel Hill and perioperative medical director at UNC Hillsborough, acted as primary investigator in the study. The data indicated that both technologies worked well, with similar speed and sensitivity. The Optopol strategy took slightly longer but was also slightly more sensitive in terms of detecting glaucomatous defects. “From the standpoint of performance and data acquisition, I’m satisfied with Zeiss’ SITA algorithms, particularly the SITA Faster algorithm, which has quickly overtaken the majority of my clinical perimetric testing,” Dr. Fleischman explains. “However, competition breeds innovation, and I’m open to new, better and cheaper technology when and where it exists.” —CK |
“The virtual reality headsets cost more than a tablet, but they’re still a lot less expensive than a standard perimeter,” Dr. Gardiner continues. “So, if you use these options you save money and gain convenience, but you’ll have higher variability in your data.”
“We do a fair amount of head-mounted perimetry in our offices,” notes Dr. Myers. “From our perspective in the clinic, it makes life easier, because instead of moving patients to the room with the machine, the head-mounted perimeter goes to wherever the patient is. That saves a lot of technician time. And, we have multiple headsets, so we don’t get as backed up on the machine.
“We’ve also done some limited home testing,” he continues. “Mathematical modeling of visual field variability has provided evidence that testing every week or every month will detect visual field progression six months to two years earlier than conventional yearly perimetry.6 We’ve already done a pilot trial with patients testing themselves every week at home using the Oll-eyes device, but that only involved about a half-dozen patients. We’re currently doing a larger trial with about 50 patients.”
Dr. Myers notes that his office has worked with Olleyes on their VisuAll perimeter. “Last year,” he says, “we published a study comparing it to Humphrey.7 We found that there’s a fair amount of agreement, but also a fair amount of difference.”
Although Dr. Myers admits that so far he has no comparative experience with other head-mounted perimeters, he’s impressed with the multiple tasks the Olleyes device is capable of performing. “In addition to visual field testing, the VisuAll can do visual acuity testing, contrast testing and color vision testing,” he says. “One reason this is helpful is that the instrument has a virtual assistant that talks to the patient, much the way a technician instructs the patient through a test. If the patient starts to perform less well on the visual field test, the assistant says things to encourage the patient to get back in the game, or encourages them by saying they’re doing a great job. That means that these tests can be run without a technician present. In the current era in which we have a shortage of technicians, this raises the possibility of helping with our workflow in the clinic.”
How do the patients feel about this option? Apparently, some elderly patients are bothered by wearing a device on their head. “For some older people it can be uncomfortable,” says Dr. Gardiner. “These devices aren’t super heavy, but they’re not light. Of course, this complaint won’t be universal, but an older person with neck issues will hate wearing a device on their head.”
However, Dr. Myers says his office has found that virtual perimetry is more ergonomically comfortable for many elderly patients. “They don’t have to lean into the visual field machine,” he points out. “So most—though not all—of our elderly patients appreciate the ergonomics.”
Dr. Gardiner points out a problem that potentially applies to both tablets and head-mounted perimeters—and sometimes is a problem in the clinic as well. “To get reliable results with any of these perimeters your eyes have to adapt to the background light level before taking the test,” he explains. “That can take several minutes.
“As you can imagine, this is a problem with patients conducting visual field tests on their own, whether they’re using a tablet or a head-mounted perimeter,” he continues. “If you’ve been out in the sun, you can’t just take the test right away and expect to get good results. So, if you have your patients use one of these options, they need to understand about allowing time for their eyes to adapt to the lighting level. In research studies, we make sure that this is managed. Ironically, even in the clinic, I suspect this may sometimes be overlooked.”
Looking Ahead
Dr. Mansberger looks forward to future improvements in visual-field-testing technology. “Of course, head-mounted perimetry could become very useful in the future,” he says. “In the meantime, we’re already seeing algorithms that incorporate factors such as whether the patient needs to be tested with a size 5 stimulus. Maybe in the future we’ll have a visual field machine that we won’t even need to program. We’ll just start it and it will figure out the best algorithm relative to the patient’s sensitivity; then it will determine whether the patient is progressing, and also look at the central visual field. We know that a lot of patients have central visual field loss, but we don’t routinely test for that today.”
“As time goes by, we’re getting more information about the costs and benefits of these different perimetry options,” Dr. Gardiner notes. “I don’t think there will ever be a consensus that one test is universally better; it will always be about balancing the costs and benefits for different individuals in different situations. That definitely includes the amount of visual damage already present. The closer someone is to losing most of their vision, the more it’s worth spending the time and effort to get the most accurate results.
“I honestly wouldn’t want to bet on which of these options will end up being the standard of care in the future,” he adds.
“It’s an exciting time for these new vision testing devices,” Dr. Myers concludes. “They’re not yet proven, but at least we’re starting down that road. I’m excited about the new ideas and new technologies these companies are developing for our patients.”
1. Heijl A, Patella VM, Chong LX, et al. A new SITA perimetric threshold testing algorithm: Construction and a multicenter clinical study. Am J Ophthalmol 2019;198:154-165.
2. Pham AT, Ramulu PY, Boland MV, Yohannan J. The effect of transitioning from SITA Standard to SITA Faster on visual field performance. Ophthalmology 2021;128:10:1417-1425.
3. Phu J, Kalloniatis M. Ability of 24-2C and 24-2 grids to identify central visual field defects and structure-function concordance in glaucoma and suspects. Am J Ophthalmol 2020;219:317-331.
4. Chakravarti T, Moghadam M, Proudfoot JA, et al. Agreement between 10-2 and 24-2c visual field test protocols for detecting glaucomatous central visual field defects. J Glaucoma 2021;30:6:e285-291.
5. Phu J, Kalloniatis M. Comparison of 10-2 and 24-2c test grids for identifying central visual field defects in glaucoma and suspect patients. Ophthalmology 2021;128:10:1405-1416.
6. Anderson AJ, Bedggood PA, George Kong YX, Martin KR, Vingrys AJ. Can home monitoring allow earlier detection of rapid visual field progression in glaucoma? Ophthalmology 2017;124:12:1735-1742.
7. Razeghinejad R, Gonzalez-Garcia A, Myers JS, Katz LJ. Preliminary report on a novel virtual reality perimeter compared with standard automated perimetry. Glaucoma 2021;30:1:17-23.
8. Mathews B, Laux J, Barnhart C, Fleischman D. Comparison of ZETA Fast (PTS) (Optopol Technology) and Humphrey SITA Fast (SFA) (Carl Zeiss Meditec) perimetric strategies. J Ophthalmol 2022, 5675793.



