Presentation
A 39-year-old African-American female presented to the Wills Eye Emergency Room with bilateral vision loss. Her vision loss was first noted in the right eye eight weeks prior to presentation with vision loss in her left eye following two weeks later. Her symptoms were associated with headache and fatigue, which she attributed to “not getting enough vitamins.” She had a CT scan of the head at an outside hospital that was reportedly “negative.” She saw a local ophthalmologist, who noted optic nerve pallor and recommended that she go directly to the Wills Eye Emergency Room for immediate evaluation. However, she chose to ignore her symptoms until a family member noted her right upper lid droop and deviation of her right eye.
Medical History
The patient’s past medical history was significant for sarcoidosis confirmed by lung biopsy in 2008, hypertension, epilepsy and hydrocephaly at birth status-post placement of a ventriculoperitoneal (VP) shunt requiring 15 to 20 revisions by the age of 15. The patient did not note any prior ocular history. Her chronic medications included levetiracetam, lisinopril and hydrochlorothiazide. She noted medication allergies to phenytoin and vancomycin. She denied any history of alcohol, tobacco or recreational drug use.
Examination
The patient’s ocular examination revealed a visual acuity of no light perception in her right eye and hand motion vision in her left eye.
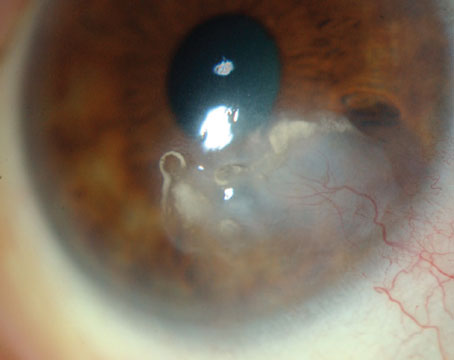
She had an amaurotic pupil on the right and a sluggish pupil on the left. In primary gaze the patient’s right eye was noted to be “down and out” (See Figure 1). Ductions revealed 50 to 70 percent limitation on supraduction, infraduction and adduction on the right, and full ductions on the left. She was unable to perform a confrontational visual field due to poor vision. Goldmann applanation tonometry revealed intraocular pressures of 20 mmHg in the right eye and 22 mmHg in the left eye. External evaluation revealed ptosis of the right upper lid with a margin reflex distance 1 (MRD1) of 0 mm on the right and 3 mm on the left. Posterior exam revealed trace bilateral optic nerve pallor without edema. Her vessels were attenuated and there was mild retinal pigment epithelial mottling in the macular areas bilaterally. The remainder of her anterior and posterior exam was normal.
|
What is your differential diagnosis? What further workup would you pursue?