Presentation
A 66-year-old Caucasian female presented to the Wills Eye Emergency Room with severe pain in her right eye for one day. She initially presented to an outside ophthalmologist who noted her intraocular pressure to be 75 mmHg in the right eye. The outside ophthalmologist placed two laser peripheral iridotomies and gave the patient 500 mg of oral acetazolamide. The intraocular pressure failed to respond, and the patient was referred to the ER for further management. The patient recounted more than 30 years of intermittent right eye soreness but none as severe as this episode.
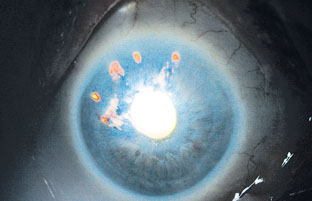 |
| Figure 1. External photograph of the right eye illustrating a shallow anterior chamber despite multiple peripheral iridotomies. Two patent peripheral iridotomies and four partially patent PIs are evident by retroillumination. |
The patient’s past medical history was significant for atrial fibrillation, hypertension and chronic lumbar pain. Review of systems was positive for a headache and back pain.
Examination
Best-corrected visual acuity was light perception only in the right eye and 20/30 in the left eye. Pupil examination revealed a fixed right pupil with a trace afferent pupillary defect. Intraocular pressure was 60 mmHg by applanation tonometry in the right eye and 18 mmHg in the left eye.
Slit-lamp examination of the right eye revealed a hazy cornea, shallow anterior chamber, six peripheral iridotomies (two patent, four partially patent), and 2+ nuclear sclerosis (See Figure 1). Angle structures in the right eye could not be visualized by gonioscopy due to corneal edema.
Slit-lamp examination of the left eye revealed a clear cornea, quiet and mildly shallow anterior chamber, one patent peripheral iridotomy, and 2+ nuclear sclerosis. Gonioscopy in the left eye revealed (A)C25p with 2+ trabecular meshwork pigmentation and no peripheral anterior synechiae.
What is your differential diagnosis? What further workup would you pursue?



