The detection of CME can be either through clinical examination, angiographic examination or optical coherence tomography examination. Of the three techniques, optical coherence tomography has the highest sensitivity, followed by angiography and then clinical examination. Therefore, the incidence of pseudophakic CME varies depending on which technique is employed. The incidence of CME measured by OCT and fluorescein angiogram after uneventful cataract surgery is up to 41 percent and 30 percent, respectively.4,5 The detection of CME with these sensitive instruments does not always correlate to visual acuity. In the past, clinical pseudophakic CME was defined as reduced visual acuity in the presence of angiographic petaloid CME following cataract extraction, and the reported incidence was 1 percent to 2 percent.6 More recently, OCT has emerged as a less invasive, more sensitive tool for detection. The incidence of pseudophakic CME with reduced vision measured by OCT is up to 14 percent.7
Histopathology
Histopathological specimens of CME following cataract surgery exhibit retinal capillary dilation, serous fluid in the outer plexiform and outer nuclear layers, and inflammatory cells in the iris, ciliary body and around blood vessels.8 Intracytoplasmic edema of Müller cells and displacement of photoreceptor nuclei and receptor axons can result in perifoveal cysts or lamellar holes in severe cases. Subretinal fluid can also be seen.
|
Pathophysiology
The pathogenesis of pseudophakic CME appears multifactorial based on experimental studies and clinical observations.5,10 Proposed etiologic factors include inflammation, vitreous traction and hypotony.11,12 Of these, the core mechanism is likely surgically induced anterior segment inflammation that results in the release of endogenous inflammatory mediators. Prostaglandins, cytokines and other vasopermeability factors disrupt the perifoveal retinal capillaries, resulting in fluid accumulation.
Prostaglandins are products of the arachidonic acid cascade and have been studied widely as contributors to edema in systemic tissues including the eye.13 Surgically induced trauma to the iris, ciliary body and lens epithelium disrupts the blood-aqueous barrier resulting in release of prostaglandins, vascular endothelial growth factor, insulin-like growth factor-1 and other inflammatory mediators.14 These chemical transmitters diffuse through the vitreous to the retina where they disrupt the blood-retinal barrier. A critical threshold of inflammatory mediators in the aqueous is likely required for detectable edema.
Risk Factors
The development of pseudophakic CME is influenced by pre-existing systemic and ocular conditions, as well as complications during surgery. It is important to identify risk factors for prophylaxis and treatment.
Diabetes mellitus, even in the absence of diabetic retinopathy, has been shown to almost double pseudophakic CME incidence rates.15 The incidence of CME post-cataract surgery has also been reported higher in eyes with diabetic retinopathy.16 Another analysis, however, suggests insufficient evidence for phacoemulsification surgery causing progression of macular edema.17 Optimally treating diabetic retinopathy and macular edema is advised prior to proceeding with cataract surgery.
Uveitic eyes have a higher incidence of pseudophakic CME detected by OCT than non-uveitic eyes.18 Strict control of ocular inflammation for at least three months is recommended prior to cataract surgery. Other ocular conditions associated with a higher incidence of pseudophakic CME include epiretinal membrane, vitreomacular traction, retinal vein occlusion and topical prostaglandin use.19,20
Before extracapsular cataract extraction technique, the rates of CME were higher with intracapsular cataract extraction. Despite advancements in phacoemulsification technique, surgical complications can still occur and increase the risk of CME. Retained lens fragments have a reported CME incidence up to 46 percent.21
Vitreous loss, vitreous to the wound, iris incarceration in the wound, posterior capsule rupture and YAG capsulotomy have all been reported to predispose to CME.5 Selection of the intraocular lens also plays a role in CME development. Iris-fixated IOLs have the highest reported rate of CME, and anterior chamber intraocular lenses have a higher rate than posterior chamber intraocular lenses.5
Diagnosis
Reduced visual acuity following cataract surgery is the most common clinical finding in pseudophakic CME. The onset is typically four to 12 weeks after surgery, reaching a peak incidence four to six weeks postoperatively. Patients may complain of metamorphopsia, central scotoma and reduced contrast sensitivity. Refraction may show a hyperopic shift. Clinical examination shows loss of the foveal depression and retinal thickening. Intraretinal parafoveal cysts may be observed, occasionally with splinter retinal hemorrhages. The use of a contact lens or narrow-slit beam with slit-lamp biomicroscopy may be helpful in identifying intraretinal cystic changes.
|
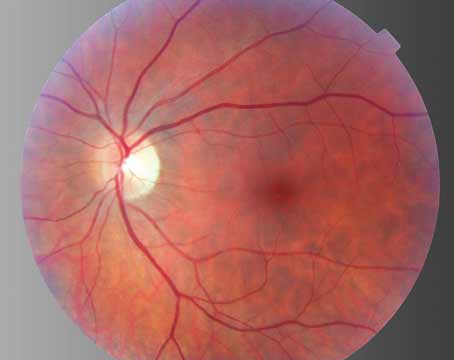
Spectral-domain OCT has emerged as a sensitive tool for detecting and monitoring pseudophakic CME. OCT is an objective, noninvasive and reproducible instrument showing cystic spaces in the outer nuclear and outer plexiform layers (See Figure 2). Occasionally, intraretinal thickening is present on OCT that lacks the distinct intraretinal cystic pattern. Detachment of the neurosensory retina with subretinal fluid may also be seen.
The natural history of pseudophakic CME is spontaneous resolution of edema with visual improvement in three to 12 months in 80 percent of patients (See Figure 3).23 Only a small proportion of patients will suffer chronic visual morbidity.
Prophylaxis and Treatment
Currently no standardized protocol exists for the prophylaxis and management of pseudophakic CME because of a lack of prospective randomized clinical trials. Therapeutic interventions are based on the proposed pathogenesis of edema, mainly inflammation and vitreous traction.
In an attempt to reduce the risk of postoperative CME, all pre-existing ocular conditions should be controlled prior to cataract surgery. Eyes with diabetic retinopathy should have appropriate evaluation and management. Uveitic eyes should have adequate inflammation control for at least three months prior to proceeding with cataract surgery.
|
The newer NSAIDs on the market include nepafenac and bromfenac, which claim enhanced penetration into the posterior segment based on animal studies.28,29 Whether similar penetration and improved therapeutic effect is found in human eyes remains unknown. A retrospective review of 450 eyes reported no clinical pseudophakic CME following uneventful phacoemulsification surgery in eyes receiving prophylactic nepafenac compared to five eyes in the control group.30 This result was statistically significant.
Topical NSAIDs do have side effects that warrant consideration, especially when using NSAIDs for a non-FDA-approved indication like pseudophakic CME. Common side effects include stinging, burning, conjunctival hyperemia and allergy. NSAIDs can be toxic to the cornea, ranging from punctate epithelial erosions to corneal infiltrates or even melt. Delayed corneal epithelial healing has also been reported.
In addition to NSAIDs, topical corticosteroids are commonly used in prophylaxis and treatment. Studies reporting the efficacy of corticosteroids in pseudophakic CME are often confounded by concomitant topical NSAID administration. It does appear that combination therapy with topical NSAID and corticosteroid may be superior to either individual therapy. A small, randomized control trial in 2000 compared topical ketorolac to topical prednisolone to combination therapy for the treatment of pseudophakic CME.31 Average improvement in Snellen visual acuity over three months was 1.6 lines in the ketorolac group, 1.1 lines in the prednisolone group and 3.8 lines in the combination group. Perhaps a synergistic effect is observed with combination therapy, although more studies are needed.
For pseudophakic CME refractory to topical therapy, periocular corticosteroids given sub-Tenon’s or subconjunctivally provide more sustained drug release. Intravitreal triamcinolone acetonide, dexamethasone implant (Ozurdex, Allergan) and fluocinolone acetonide implant (Retisert, Bausch + Lomb) have also been used in refractory cases. The literature reporting their efficacy in macular edema is mainly in diabetic or retinal vein occlusion eyes. Their efficacy in pseudophakic CME is unknown. Side effects of periocular and intravitreal corticosteroids include endophthalmitis and elevated intraocular pressure.
Vascular endothelial growth factor causes breakdown of the blood-retinal barrier and increased vascular permeability, contributing to the development of macular edema. Anti-VEGF with intravitreal bevacizumab (Avastin, Genetech) has been shown effective in refractory pseudophakic CME. A multicentered, retrospective study reported that 72 percent of eyes with refractory pseudophakic CME treated with at least one intravitreal bevacizumab injection had improvement in visual acuity with a reduction in mean central macular thickness at 12 months.32 Forty-three percent of the eyes required more than one injection for best visual acuity.
Carbonic anhydrase inhibitors like oral acetazolamide affect fluid pumping across the subretinal space by retinal pigment epithelial cells. They have been reported effective in treating macular edema due to retinitis pigmentosa and aphakia, but their efficacy in pseudophakic CME is unknown.
When medical therapy is ineffective in resolving pseudophakic CME, surgical intervention is often the next step. Removal of a malpositioned intraocular lens may be effective in certain refractory cases.33 Nd:YAG laser and pars plana vitrectomy can be used to lyse abnormal vitreous adhesions to the intraocular lens, corneal wound or iris. Release of vitreomacular traction is believed to allow resolution of macular edema. A multicenter, randomized control trial in 1985 examined eyes with chronic aphakic CME attributed to vitreous adherence to the wound.34 Eyes that underwent pars plana vitrectomy had improved visual acuity compared to controls.
Other therapies reported in small pilot series as effective for refractory pseudophakic CME include intravitreal infliximab (Remicade, Centocor Ortho Biotech),35 intravitreal diclofenac 500 μm/0.1 ml,36 and subcutaneous interferon alpha (Imgenex).37
Over the past decade, the detection and monitoring of pseudophakic CME has improved with the development of high-resolution, spectral domain OCT. However, the prevention and management of the disease has remained relatively unchanged. Topical NSAIDs and corticosteroids remain mainstay therapy. Evidence for NSAID use is stronger than for corticosteroid use, and combination therapy may be superior to single therapy although further studies are needed. REVIEW
Dr. Lally is a first-year surgical vitreoretinal fellow at the Ophthalmic Consultants of Boston/Tufts Medical Center, and he completed his residency in ophthalmology at the Wills Eye Institute in Philadelphia. Dr. Shah is a vitreoretinal surgeon at Ophthalmic Consultants of Boston and an assistant professor at Tufts University School of Medicine. Contact Dr. Shah at Ophthalmic Consultants of Boston, 50 Staniford St., Ste. 600, Boston, MA, 02114. Phone: (617) 314-2693. E-mail: cpshah@eyeboston.com.
1. Irvine SR. A newly defined vitreous syndrome following cataract surgery. Am J Ophthalmol 1953;36:599-619.
2. Gass JD, Norton EW. Follow-up study of cystoid macular edema following cataract extraction. Trans Am Acad Ophthalmol Otolaryngol 1969;73:665-682.
3. Loewenstein A, Zur D. Postsurgical cystoid macular edema. Dev Ophthalmol 2010;47:148-159.
4. Lobo CL, Faria PM, Soares MA, Bernardes RC, Cunha-Vaz JG. Macular alterations after small-incision cataract surgery. J Cataract Refract Surg 2004;30:752-760.
5. Flach AJ. The incidence, pathogensis and treatment of cystoid macular edema following cataract surgery. Trans Am Ophthalmol Soc 1998;96:557-634.
6. Wright PL, Wilkinson CP, Balyeat HD, et al. Angiographic cystoid macular edema after posterior chamber lens implantation. Arch Ophthalmol 1988;106:740-744.
7. Kim SJ, Belair ML, Bressler NM, et al. A method of reporting macular edema after cataract surgery using optical coherence tomography. Retina 2008;28:870-876.
8. Michels RG, Green WR, Maumenee AE. Cystoid macular edema following cataract extraction (The Irvine-Gass Syndrome): A case studied clinically and histopathologically. Ophthalmic Surg 1971;2:217-221.
9. McDonnell PJ, de la Cruz ZC, Green WR. Vitreous incarceration complicating cataract surgery: A light and electron microscopic study. Ophthalmology 1986;93:247-253.
10. Jampol LM. Aphakic cystoid macular edema: A hypothesis. Arch Ophthalmol 1985;103:1134-1135.
11. Reese AB, Jones IS, Cooper WC. Macular changes secondary to vitreous traction. Trans Am Ophthalmol Soc 1966;64:123-134.
12. Wolter JR. The histopathology of cystoid macular edema. Albrecht Von Graefe’s Arch Klin Exp Ophthalmol 1981;216:85-101.
13. Miyake K, Ibaraki N. Prostaglandins and cystoid macular edema. Surv Ophthalmol 2002;47:S203-S218.
14. Murata T, Nakagawa K, Khalil A, et al. The relation between expression of vascular endothelial growth factor and breakdown of the blood-retinal barrier in diabetic rat retinas. Lab Invest 1996;74:819-825.
15. Schmier JK, Halpern MT, Covert DW, et al. Evaluation of costs for cystoid macular edema among patients after cataract surgery. Retina 2007;27:621-628.
16. Hayashi K, Igarashi C, Hirata A, Hayashi H. Changes in diabetic macular oedema after phacoemulsification surgery. Eye (Lond) 2009;23:389-396.
17. Shah AS, Chen SH. Cataract surgery and diabetes. Curr Opin Ophthalmol 2010;21:4-9.
18. Belair ML, Kim SJ, Thorne JE, et al. Incidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomography. Am J Ophthalmol 2009;148:128-135.
19. Henderson BA, Kim JY, Ament CS. Clinical pseudphakic cystoid macular edema: Risk factors for development and duration after treatment. J Cataract Refract Surg 2007;33:1550-1558.
20. Warwar RE, Bullock JD, Ballal D. Cystoid macular edema and anterior uveitis associated with latanoprost use: Experience and incidence in a retrospective review of 94 patients. Ophthalmology 1998;105:263-268.
21. Cohen SM, Davis A, Cukrowski C. Cystoid macular edema after pars plana vitrectomy for retained lens fragments. J Cataract Refract Surg 2006;32:1521-1526.
22. Ursell PG, Spalton DJ, Whitcup SM, Nussenblatt RB. Cystoid macular edema after phacoemulsification : Relationship to blood-aqueous barrier damage and visual acuity. J Cataract Refract Surg 1999;25:1492-1497.
23. Bradford JD, Wilkinson CP Bradford RH. Cystoid macular edema following extracapsular cataract extraction and posterior chamber intraocular lens implantation. Retina 1988;8:161-164.
24. Chin MS, Nagineni CN, Hooper LC, Detrick B, Hooks JJ. Cyclooxygenase-2 gene expression and regulation in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 2001;42:2338-2346.
25. Rosetti L, Chaudwi H, Dickersin K. Medical prophylaxis and treatment of cystoid macular edema after cataract surgery: The results of a meta-analysis. Ophthalmology 1998;105:397-405.
26. Yavas GF, Ozturk F, Kusbeci T. Preoperative topical indomethacin to prevent pseudophakic cystoid macular edema. J Cataract Refract Surg 2007;33:804-807.
27. Flach AJ, Jampol LM, Weinberg D, et al. Improvement in visual acuity in chronic aphakic and pseudophakic cystoid macular edema after treatment with topical 0.5% ketorolac tromethamine. Am J Ophthalmol 1991;112:514-519.
28. Gamache DA, Graff G, Brady MT, et al. Nepafenac, a unique nonsteroidal prodrug with potential utility in the treatment of trauma-induced ocular inflammation. I: Assessment of anti-inflammatory efficacy. Inflammation 2000;24:357-370.
29. Baklayan GA, Patterson HM, Song CK, et al. 24-h evaluation of the ocular distribution of (14)C-labeled bromfenac following topical instillation into eyes of New Zealand White rabbits. J Ocul Pharmacol Ther 2008;24:392-398.
30. Wolf EJ, Braunstein A, Shih C, Braunstein RE. Incidence of visually significant pseudophakic macular edema after uneventful phacoemulsification in patients treated with nepafenac. J Cataract Refract Surg 2007;33:1546-1549.
31. Heier JS, Topping TM, Baumann W, Dirks MS, Chern S. Ketorolac versus prednisolone versus combination therapy in the treatment of acute pseudophakic cystoid macular edema. Ophthalmology 2000;107:2034-2039.
32. Arevalo JF, Maia M, Garcia-Amaris RA, et al; Pan-American Collaborative Retina Study Group (PACORES). Intravitreal bevacizumab for refractory pseudophakic cystoid macular edema: The Pan-American Collaborative Retina Study Group results. Ophthalmology 2009;116:1481-1487.
33. Shepard DD. The fate of eyes from which intraocular lenses have been removed. Ophthalmic Surg 1979;10:58-60.
34. Fung WE, Vitrectomy-ACME Study Group. Vitrectomy for chronic aphakic cystoid macular edema. Results of a national, collaborative, prospective, randomized investigation. Ophthalmology 1985;92:1102-1111.
35. Wu L, Arevalo JF, Hernandez-Bogantes E, Roca JA. Intravitreal infliximab for refractory pseudophakic cystoid macular edema: Results of the pan-american collaborative retina study group. Int Ophthalmol 2012;32:235-243.
36. Soheilian M, Karimi S, Ramezani A, Peyman GA. Pilot study of intraviteal injection of diclofenac for treatment of macular edema of various etiologies. Retina 2010;30:509-515.
37. Deuter CM, Gelisken F, Stubiger N, et al. Successful treatment of chronic pseudophakic macular edema (Irvine-Gass syndrome) with interferon alpha: A report of three cases. Ocul Immunol Inflamm 2011;19:216-218.