In this article, we’ll discuss the pitfalls that physicians face when talking with patients, and how to streamline communications to make a practice as efficient as possible, while still putting the patient first.
Practices’ Pitfalls
Perhaps the best place to begin is where practices go wrong and what mistakes to avoid when building a relationship with patients. Maureen Waddle, a principal and senior consultant with BSM
 |
John Pinto, of J. Pinto and Associates, an ophthalmic practice management consulting firm, also shares two extreme examples of failure to communicate with patients. “There’s a lot of latitude in this area. In practice A, the doctor would walk into the room, not say hello to the patient, do the slit lamp exam, dictate his findings to the scribe, and then walk out. He would not say hello, goodbye, shake hands or describe the condition to the patients,” Mr. Pinto explains. “Upon the doctor’s departure, the scribe would then become the health educationist, and say, ‘The doctor has described that you have a cataract, and here’s what that is and how we can help you with that.’ Then they would escort the patient to the surgical counselor when that was indicated.
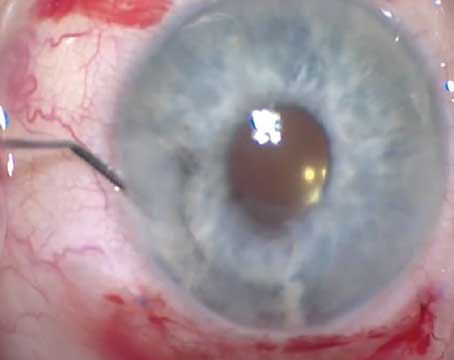
“Now in practice B, in the same kind of suburban environment and patient demographic, the doctor would walk in, without a scribe in the room,” he continues. “He would spend at least a half an hour, up to 45 minutes, doing the most routine of exams. He had a biology roll-down chart, which had a sagittal section of the eye on it, and he would use a stick with a hook on the end of it to pull this chart down. At the end of each exam, he’d roll it back up just so he could dramatically pull the chart down for the next patient.
“This practice, you might assume, was where the patients were extremely satisfied,” Mr. Pinto says. “In point of fact, his practice was shrinking due to his inefficiency. When we talked to some of his patients in a group, one patient said, ‘He’s okay, but when he pulls down that chart, I know I’m going to be in there for a while.’ He was providing graduate level education for his patients, and they weren’t satisfied. It wasn’t belittling—he was just a pedant. We heard a lot of, ‘I don’t want to know that much about my eyes. I want to get in, get out and get on with my day.’
“Thankfully, the vast majority of ophthalmologists practice between the extremes of Doctors A and B,” Mr. Pinto says.
Joseph Panarelli, MD, an ophthalmologist based in New York, discusses his experience with talking to patients in terms they’ll understand. “There’s definitely a learning curve when you start, because you’ve come out of school and residency and your instinct is to keep talking like you’re being tested. It’s a weird feeling because that language is a part of your life at that point. You need to be able to step back and realize that the vast majority of people won’t understand what glaucoma is or what is medically happening to their eyes,” he says. “It’s an invaluable skill to be able explain, in layman’s terms, what is happening. It’s a tough instinct to shake. It just takes time and practice.”
Staff and Patients
Because a great staff can enhance a patient’s visit and make the doctor’s life that much easier, proper communication with not only patients but also with your staff is essential for having a patient leave a practice satisfied with his visit. “There is nothing more frustrating than having a tech express one thing to a patient, and then a doctor expresses a different or contradictory opinion,” Ms. Waddle claims. “That’s a training issue with the staff. You have to get that under control. It does help the doctor to have the techs and scribes do some patient education, but there’s definitely a line. It’s critical, because if you have conflicting messages, that will break down the patient’s confidence and trust in the doctor.”
Mr. Pinto also says he’s seen this happen. “I’ve seen examples where techs have overstepped their bounds and have begun telling patients what’s wrong with them and what the next steps are. Then the doctor comes in and sees that the tech has it wrong. That has to be stopped,” he states. “I’ve seen opposite far extreme of that too, where the staff has to memorize scripts with responses to questions that patients have. Like being on Broadway with no latitude. That’s stiff and off-putting to the patients and the staff.
“It takes a couple years of decent training and exposure for a person who’s never been a tech before to become an effective tech,” he continues. “In practices that have great HR habits, technicians stick around long enough to learn all these things. But practices that are problematic have this adverse cycle they’ll get into. The working conditions aren’t great, so the tenure isn’t long, so the staff don’t hang in there long enough to learn how to do their jobs confidently. Then the doctors get frustrated, and the wheel keeps turning.”
Mr. Pinto offers some solutions to this issue, seen in some of the most efficient practices. “The doctor has to be engaged in the process of staff education, to make sure that the patients feel cared for,” he says. “Even at the front desk, patients will often have follow-up questions before they leave about how to use their new eye drops or something to that effect. If you don’t know how to talk to them there, you could lose a valued patient.”
Further emphasizing the importance of a well-trained staff, Mr. Pinto says, “It’s not always about the face-to-face time with the doctor. I think it’s about listening, ultimately. Not how much you can tell the patient, but how you can make sure they’re heard. You can’t view them as patients you’ve seen thousands of times before, even though you have. You have to give them time as individuals and make sure they feel their concerns and questions are heard. Doctors can have three- to four-minute encounter times when they’re supported by a great staff that delight patients and are extremely efficient in how they run their practice,” he continues. “On the flip side, you also see doctors with 10- to 15-minute times that have unsatisfied patients. Your staff can take a lot of the pressure off your hands if they’re properly trained.”
Putting the Patient at Ease
When practice-management experts sit down with patients and doctors, one of the most valuable attributes of the doctor is the ability to put the patient at ease about whatever procedure the doctor is performing and to effectively explain a complex procedure in simple terms.
Mitchell Jackson, MD, an ophthalmologist from Lake Villa, Ill., says, “I think this is an area where there’s a steep learning curve. It’s valuable because this will be why patients come back, and what they’ll talk about when people ask them how the procedure went,” he says. “I take five to 10 minutes to explain to them what we’re about to do and walk them through the procedure as best I can, in terms they’re familiar with. Analogies help here, but if it gets into the real nitty-gritty technical stuff, I’ll brush over that, and focus on the bigger picture and end results of the procedure.”
Dr. Jackson notes the importance of the staff in his approach to putting the patient at ease. “There’s only so much you can say,” he points out. “If you have a trained staff behind you that the patient trusts, then their word supporting yours means a lot. That can be the difference between someone who’s a nervous wreck and someone who’s confident going into surgery. Even before surgery, the staff can be there to comfort patients and reassure them. If you have a competent and trustworthy staff behind you, it’s much more comforting for the patient.”
Ms. Waddle also gives some advice to doctors on how to put a patient at ease before a procedure. “When you’re going into surgery, recommend that the patient bring someone with him. We all hear and perceive things differently, so to have at least one other person listening along with the patient who can help clarify is always helpful and reassuring,” she says. “They might also ask a question that the patient didn’t think of at the time, which can be valuable. So encourage patients to bring loved ones or family with them. It goes a long way. It also helps to have some simple instructions or common experiences for the patients in writing. A lot of practices use videos sometimes, too.
“Most importantly I think, is for doctors to learn from each other—take these pearls from your colleagues and figure out what works when communicating with patients,” she continues. “Listen for the best analogies and descriptions that will resonate with your patients. I know a lot of doctors use the camera analogy to describe your eyes. It’s great if you can find a few analogies that work and connect with the patients. That helps them be more confident in what they’re facing.”
“We are all patients of one doctor or another and we’ve all had the experience of being jabbed by a needle or poked at without any fair warning,” Mr. Pinto adds. “There’s a real call for some advanced notice and timing. I recently had a procedure and the doctor took me in and had his assistant in the room hold my hand. Now I don’t necessarily need that, but it’s a really nice touch, one that we could learn a lot from in eye care.”
Legal Troubles
Not only can a lack of communication with patients lead to an inefficient and stunted practice, there are also some weighty legal pitfalls that could come attached. Anne Brendel, a health-care attorney in Los Angeles, claims, “Legal issues often make physicians pay more attention to their requirements. They’re more likely to listen if they can be punished for it.” With that in mind, here’s a look at some legal troubles that could befall a practice as a result of inefficient communication with its patients.
“Initially, talking to the patients obviously helps strengthen that patient-doctor relationship. Good communication also helps practitioners obtain proper consent,” Ms. Brendel says. “CMS has offered guidelines for informed consent as well. Communication can also decrease civil and criminal liability.
“Ultimately, and worst-case scenario, fraud can be an issue—even malpractice,” she continues. “Having the appropriate conversation with the patient is important as a way to decrease liability for practitioners. Documenting this conversation is important too. Should an action arise later, it’s not he-said, she-said, because the conversations were documented.”
As for how to avoid these legal issues, she offers some advice. “Treatment information sheets are very helpful. You can attach those to the informed-consent forms. In addition to having a conversation with the patient, you should keep a document ultimately signed by the patient that lays everything out clearly,” she says. “Something that says that you talked about the risk and the patient had an opportunity to ask questions. This can also protect physicians later, too, because there will be documentation that the patient had the opportunity to raise a question, even if he chose not to. When you have that, it protects the physicians since it puts the fault back on the patient for not raising a concern when he had an opportunity to.”
With new technologies on the rise and increasingly strict regulatory measures, taking five minutes to talk and actively listen to patients is becoming a forgotten art. However, the best practices still know the intrinsic value of taking the time to talk with a patient. “Ultimately, in the best practice, where satisfaction is the highest, these things are seen as important from the top of the organization down,” Mr. Pinto says. “These interactions are as much what patients are paying for as the surgery or treatment they may need. The best practices hone their communication craft just as they do their surgical craft.” REVIEW
None of the contributors to this article have disclosed any financial interests.