Alan Kay, the computer scientist behind the graphical-user interface that eventually became the centerpiece of the Apple Macintosh, once said, "The best way to predict the future is to invent it." If this is true, the engineers at Lenstec are trying to predict a future of intraocular lenses in which accommodative IOLs are the most popular option for surgeons looking to treat presbyopia. Here's the latest data from the large-scale U.S. Food and Drug Administration study of Lenstec's Tetraflex IOL, and where the lens may go from here.
The Concept
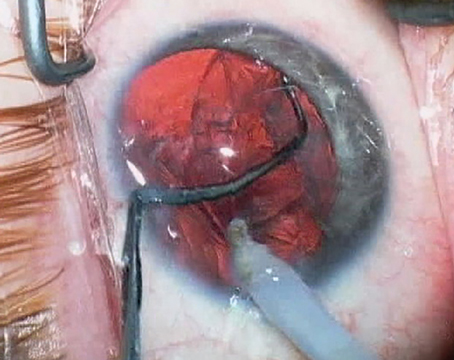
The Tetraflex is a single-piece lens composed of hydrophilic acrylic material with a 5.75-mm, UV-blocking optic. It has two haptics, also made of hydrophilic acrylic. The lens is flexible, with a 5-degree anterior vault.
Paul Dougherty, MD, an investigator for and consultant to Lenstec, says the lens is designed to provide some measure of accommodative amplitude by relying on two forces in the eye. "During accommodation, the ciliary body contracts and vitreous pressure increases," he says. "This pushes the lens forward, increasing both the effective power of the lens and coma, the latter being one of the natural mechanisms of accommodation."
Since the lens is similar in size to a monofocal IOL, Dr. Dougherty says he hasn't encountered problems with inserting it. "You usually can get the whole lens into the capsular bag with the injector, and you then move the lens back and forth to make sure the haptics are in the proper position," he explains. "I use a 2.8-mm incision to put it in, but I've seen it implanted through an incision as small as 2.2 mm. The current injector cartridge is 1.8 mm, but the company has a new 1.6-mm injector cartridge as well. The 1.6-mm cartridge goes through a 2.2-mm incision. We used the 1.8-mm cartridge in the study, so that's probably the one that will be approved. There's also a pre-loaded injector that's in the final stages of development. Right now, my tech loads the cartridge preoperatively."
Lens Performance
Currently available data on the Tetraflex from the lens's FDA trial includes one-month outcomes of 265 eyes of 168 patients and six-month outcomes on 174 eyes of 111 patients. Dr. Dougherty recently presented data on 103 eyes of 62 patients at the meeting of the Society for Excellence in Eyecare/American College of Eye Surgeons meeting in February. Forty-one of the 62 patients underwent bilateral Tetraflex implantation, with the rest only getting the lens in one eye.
In Dr. Dougherty's data set, at six months 55 percent of the patients could see 20/20 or better uncorrected, and 96 percent could see 20/40 or better. Eighty-one percent of the patients are within ±0.5 D of the intended refraction and 96 percent are within ±1 D.
Considering distance-corrected near vision, which many use to evaluate the performance of presbyopic IOLs, 85 percent of the patients could read newspaper print (20/80 or better) at six months. Twenty-two percent were able to read print smaller than that used in a newspaper's classified ads. Overall, at six months postop, 46 percent of the patients had a binocular accommodative amplitude of at least 2 D and 15 percent of them got 3 D or more of accommodation.
"The main issue with the lens is not everyone gets full accommodation," says Dr. Dougherty. "In the study, we were only allowed to do 0.5 D of mini-monovision in one of the patient's eyes to maximize his or her reading ability. But they get functional reading.
If patients ever need reading glasses, they pop in a pair of +1s at night." Dr. Dougherty predicts that, when the lens eventually is approved, he'll probably induce 0.5 D to 0.75 D of monovision to boost the near vision.
Dr. Dougherty says, though, that bilateral implantation is preferable to monocular. As evidence of this, he points to a study from the
In 175 bilaterally implanted Tetraflex patients available for follow-up at one year from the FDA study, 55 percent say that they occasionally wear glasses to read small print or in dim lighting conditions compared to 35 percent of 54 monofocal IOL control patients, and 19 percent of Tetraflex patients say they never wear them vs. 11 percent of controls. Twenty-six percent say they always have to wear glasses for near tasks postop compared to 54 percent of the monofocal patients. The differences were statistically significant (p<0.001).
Dr. Dougherty says, though, that patients' reading speed in the FDA study was impressive. "Traditionally, clinicians look at distance-corrected near vision for evaluation of presbyopic lenses, but sitting and staring at a chart and picking out letters isn't that clinically relevant," Dr. Dougherty says. "What we did in the study was look at reading speed using the MNRead functional reading test." The reading test was performed binocularly in 41 bilaterally implanted cases using the patients' infinity corrected distance vision correction. A group of 35 patients with monofocal IOLs was used as a control. The testers made an audio recording of the patients as they read, which was then scored at a central reading center.
At one year, the two groups have similar reading speed in print sizes equivalent to 20/80 vision and larger. As the print gets smaller, however, the Tetraflex group shows a statistically significantly better reading speed, down to a print size that's equal to 20/25, at which point the control group can't read. Dr. Dougherty points out that, even at the 20/40 print size, which is smaller than the print in a phonebook, the Tetraflex patients average 63 words per minute vs. 26 wpm for the monofocal patients.
The adverse events that occurred in the
As far as the lens's approval status with the FDA, Lenstec Vice President Jim Simms says more follow-up is needed before the ultimate submission for marketing approval.
"The enrollment for the study is complete, and we're now waiting for our entire patient population to reach two years postop," he says. "We should be submitting our file for approval by the end of this year, and then it's up to the FDA."