One of the most disheartening, and downright scary, complications of LASIK is corneal ectasia, since it's a condition that will get progressively worse and take the patient's vision with it. Some surgeons, however, are trying novel techniques on patients with post-LASIK ectasia, and say the results show promise. Here's a discussion of how these emerging methods may help these eyes.
The Latest on Intacs
Beverly Hills, Calif., surgeon Brian Boxer Wachler has used Addition Technology's Intacs on 40 patients with post-LASIK ectasia, based on data from studies of Intacs for either keratoconus or ectasia.1-3
"At the point I'm considering Intacs for these patients, they've had the ectasia for probably six months to a year, at least," he says. "The severity can range from mildly reduced uncorrected acuity and induced astigmatism to dramatically reduced best-corrected acuity in which people may not even be able to wear a gas-permeable contact lens. So it becomes a matter of case-by-case goal management, depending on how advanced they are."
In many cases, Dr. Boxer Wachler just uses a single Intac, usually a 0.30 mm or 0.35 mm, rather than two. He puts it in at an optical zone of 6.8 mm at 66 percent corneal depth.
He says it's very important to understand the manifest refraction in these patients, because, even though their acuity may not be very good, the axis of astigmatism is crucial. Knowing the axis allows him to make the entry incision on axis to help reduce the cylinder. If the manifest is 20/40 or worse best-corrected, he'll have the patient manually turn the knob on the phoropter that controls the astigmatic axis until he subjectively finds the clearest meridian, because, he says, the Jackson Cross cylinder lens in these patients isn't very helpful. Also, the manifest refraction must be in plus-cylinder notation. If the refraction were in minus-cylinder notation, the incision would be 90 degrees from where it should be.
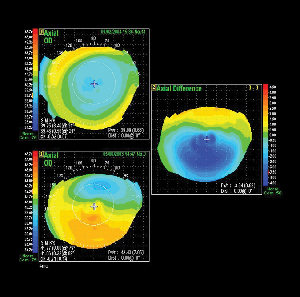 |
| A post-LASIK ectasia patient who was caught early (bottom topography). Top image: The same eye 11 months after using the drops. The corneal shape has become more regular, but the patient needs to remain on the drops to keep the effect. Image: Brian Boxer Wachler, MD. |
The results depend on how advanced the patient's ectasia is.
"The more advanced the ectasia, the more modest my goals will be," he says. "If someone has really advanced ectasia and 8 D of astigmatism, perhaps the goal is to get them down to 4 D of astigmatism. And if they were having difficulty wearing a gas-perm lens beforehand, maybe our goal would be to get them into a soft toric lens or to be more comfortable in a gas-perm lens. But for someone with mild ectasia, maybe our goals would be to actually improve his uncorrected acuity and allow good vision with glasses."
Regarding the limits of the effectiveness of the procedure, Dr. Boxer Wachler says they're "hard to quantify … It's kind of an overall culmination of the exam with how steep the corneas are or if there's any central scarring. But I think it's worthwhile in patients who have thick enough peripheral corneas to maintain the segments, so they don't shift or come out." He estimates that peripheral corneas that are greater than 500 µm can still be good candidates for an Intac, because that's the area of the cornea in which the segment will be placed.
Even with apparently promising results, two studies in particular recommend longer-term study of the stability of this treatment.2,3 Dr. Boxer Wachler is currently pooling the data from his 40 patients for analysis.
Riboflavin and UV Light
Surgeons are also trying a combination treatment of riboflavin and ultraviolet light to strengthen the cornea.
The work was pioneered by European surgeons who performed a prospective, nonrandomized study in which 23 eyes of 22 patients with moderate or advanced progressive keratoconus with a K value from 48 to 72 D received a central corneal abrasion, then drops of riboflavin.4 The eyes were then exposed to 370-nm wavelength (UVA) light at 3mW/cm2 for 30 minutes. The follow-up ranged from three months to four years.
In all eyes, the keratoconus's progression was stopped. In 16 (70 percent) there was a regression, with a reduction of the maximal K readings by 2.01 D and of the refractive error by 1.14 D. Corneal and lens transparency, endothelial cell density and intraocular pressure were stable.
Ronald Krueger, the Cleveland Clinic's director of refractive surgery, has been experimenting with the riboflavin/UV treatment in pig eyes, and measuring his results with a prototype instrument called the Sonic Eye (Priavision, Menlo Park, Calif.).
"The device is about the size of a cigar, and has two probes, one an ultrasonic transmitter, the other a receiver," explains Dr. Krueger. "The transmitter passes a surface wave across the cornea to the receiver, and the shorter the time of flight of the wave, the stiffer the tissue."
In eight pig eyes, he and Satish Herekar, vice president of Priavision, treated half the cornea with riboflavin/UV, and left the other half untreated. He found an increase in the speed of the surface wave of about 1.8 times in the treated sections. He then measured the stress/strain relationships of the corneas, and found the treated corneas needed 1.5 to 2.5 times more stress to achieve the same strain; their stiffness had increased. He says the magnitude of this strain relationship with crosslinking correlated well with the Sonic Eye data.
Dr. Boxer Wachler has also performed the riboflavin treatment on patients with post-LASIK ectasia, sometimes combining it with Intacs for more progressive cases. He says his riboflavin formulation is proprietary, and he applies the drops every three minutes during the half hour of UV light exposure.
He notes the results vary depending on the patient's condition.
"It increases the rigidity of the cornea, getting it closer to normal," he says. "What we've seen is that, depending on the severity, virtually everyone has improved. The key is to have the patient know what to expect. For patients who have to wear glasses, for example, we may be able to get them out of glasses if their ectasia is mild." He says there's been no corneal toxicity and endothelial cell counts haven't changed.
Glaucoma Drops
Finally, for a handful of LASIK patients whose ectasia was caught very early, which is usually a month or less after it appears, Dr. Boxer Wachler has used glaucoma drops to decrease the intraocular pressure with the hope of decreasing the deformity in the cornea. He got the idea after listening to a paper on changes in corneal shape induced by changes in IOP by Peter Pinsky, PhD, of Stanford, at the 5th International Congress of Wavefront Sensing and Optimized Refractive Corrections this past February. "I connected the dots to develop the use of glaucoma drops for early ectasia reversal," he says. There haven't been any controlled studies of the technique, however.
"If you imagine the ectasia as a hernia, you have a balance of IOP pushing out and atmospheric pressure pushing in, with corneal shape being a balance between them," says Dr. Boxer Wachler. "Normal corneas don't have much shape fluctuation due to IOP, but a weak or ectatic cornea can have an increased amount. So, if you lower the IOP, atmospheric pressure pushes back, and it's possible to reverse the ectasia if treated early enough."
In the few patients he's used it in, there was only about 1 to 2 D of induced cylinder from the ectasia because they were caught early. Dr. Wachler says he was able to reverse the ectatic state. One possible drawback is that the patients have to stay on the drops; some have been on them for 14 months. However, he says there haven't been any complications from the drops so far.
1. Boxer Wachler BS, Christie JP, Chandra NS, et al. Intacs for keratoconus. Ophthalmology 2003;110:5:1031-40.
2. Pokroy R, Levinger S, Hirsh A. Single intacs segment for post-laser in situ keratomileusis keratectasia. J Cataract Refract Surg 2004;30:8:1685-95.
3. Kymionis GD, Siganos CS, Kounis G, et al. Management of post-LASIK corneal ectasia with intacs inserts. Arch Ophthalmol 2003;121:322-26.
4. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 2003;135:5:620-627.