If this year’s survey on cataract-surgery techniques is any indication, surgeons appear to be warming up to different techniques—some new-ish, some more established but gaining a following. For instance, usage of horizontal phaco chop went up by almost 12 percentage points compared to last year’s survey, and the percentage of surgeons who use either the femtosecond or the Zepto for some aspect of their cataract procedures increased by about 5 percentage points. More surgeons have taken a liking to the Yamane IOL fixation technique, with the percentage who say they prefer to use it increasing by 13 percentage points compared to last year.
These are just some of the findings on this year’s survey on cataract surgery technique. This year, 4,159 of the 10,442 surgeons receiving the survey opened it (40 percent open rate), and 73 completed the survey. To see how your favorite surgical techniques and maneuvers compare with theirs, read on.
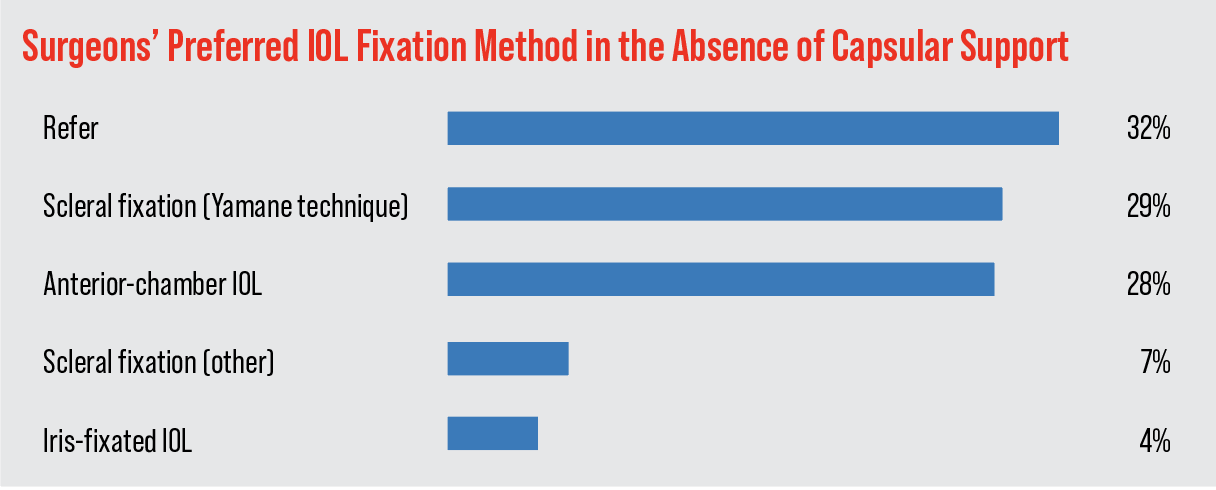 |
Suturing an IOL
When faced with an IOL that has little or no capsular support, a good number of surgeons (29 percent) turn to the Yamane technique. This is an increase of 13 percentage points compared to last year’s survey. Twenty-eight percent of the respondents use an anterior-chamber IOL and 7 percent perform a form of scleral fixation other than Yamane. The rest of the results appear in the graph above.
“I like the Yamane technique because of its relative simplicity,” says Robert Bullington Jr., MD, of Phoenix. “It’s the least-invasive and gives very stable IOL fixation,” says another surgeon. Jonathan Adler, MD, of Bradenton, Florida, notes, “[Yamane] places the lens in the best position and is stable.” A surgeon from Montana agrees, saying, “The Yamane technique is predictable.”
A surgeon from Virginia prefers to use an anterior-chamber IOL. “The outcomes are equal [to other methods] but it’s done quicker for the patient (they can see sooner),” he says. Richard Wieder, MD, of Missouri also uses AC IOLs in these situations, because the procedure is “Quick and very straightforward.” Mechanicsville, Virginia, surgeon D. Alan Chandler opines, “I would do an iris-fixated approach but sometimes it doesn’t work well.”
Managing Astigmatism
Surgeons also delved into the various ways they tackle a patient’s pre-existing astigmatism.
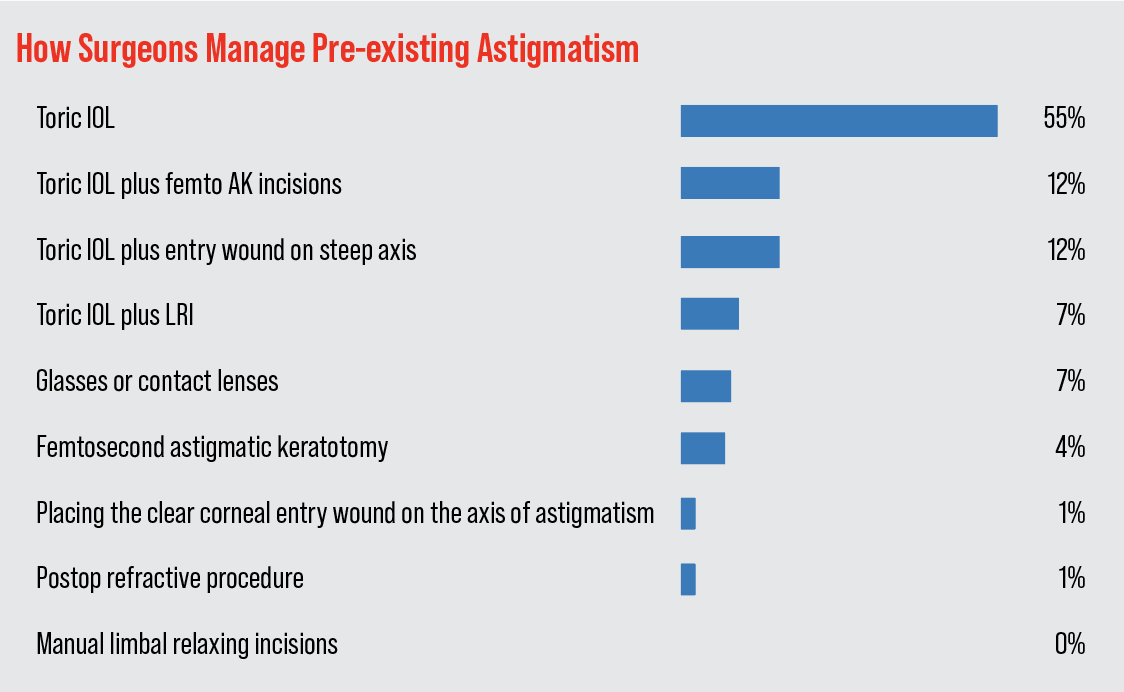 |
The most popular option is a toric IOL, chosen by 55 percent of the respondents. Combining a toric with placing the entry wound on the steep axis comes in second, with 12 percent, tied with combining a toric lens with femto astigmatic keratotomy. The rest of the options and their results appear in the graph above.
“Toric IOLs, when guided by intraoperative aberrometry, provide excellent astigmatism improvement,” says Dr. Wieder. A surgeon from California feels similarly, saying, “[Toric IOLs] are reliable and don’t weaken the cornea or require me to change my incision site.”
“Using a toric IOL typically provides a more predictable and better postoperative outcome,” Dr. Bullington says. “I’ll also place my incision along the axis of astigmatism, depending upon the amount and axis of the astigmatism.” Marc Michelson, MD, of Birmingham, Alabama, says he often goes the toric IOL route because, he says, it’s a “one-step process and there’s no alteration in the corneal architecture. Resort to postop refractive procedures as needed.”
Ligaya Prystowsky, MD, of Nutley, New Jersey, uses a toric lens but combines it with an entry wound on the steep axis. She says, “I’ve used the femto when available but with toric IOLs at a higher power now, [the remaining astigmatism] is not as significant and I can add sutures for the last diopter if necessary.”
Other Technology Options
Some surgeons rely on various technologies that they say enhance their results.
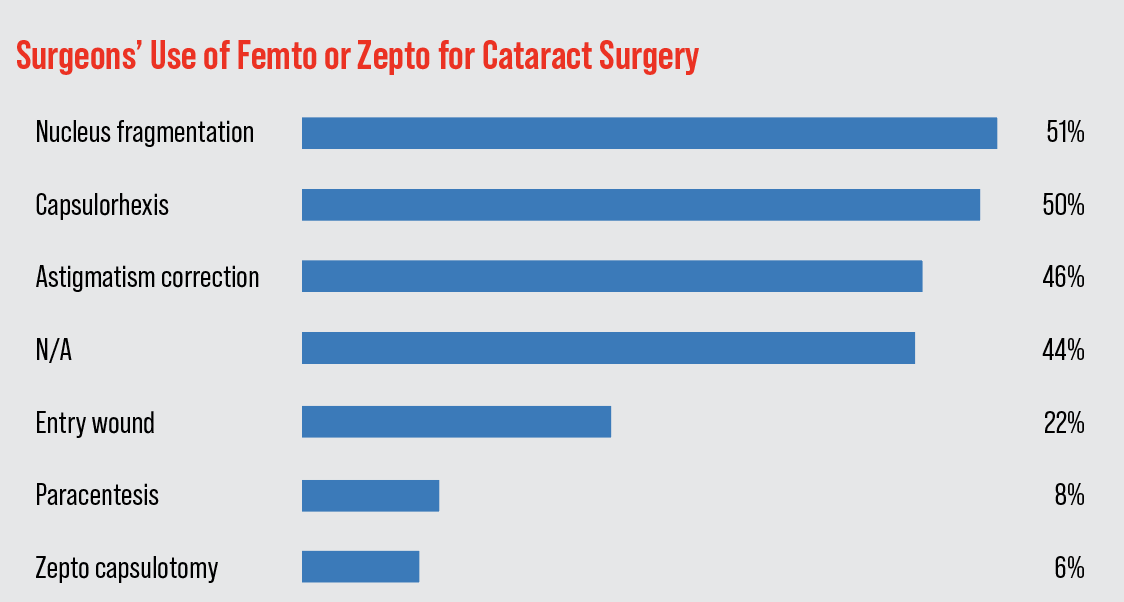
• Femtosecond laser and Zepto. On this year’s survey, 56 percent of the surgeons say they use either the femtosecond laser or the Zepto in their cataract surgeries. Of these, 10 percent use the Zepto device for capsulotomy creation, the rest use a femtosecond laser for one or more stages of the procedure. The most popular use of the femto is to create the capsulorhexis (chosen by 50 percent of the surgeons), followed by nuclear fragmentation (48 percent). The surgeons could choose more than one answer for this question. The breakdown for the rest of the uses appears in the graph below.
 |
 |
William Lipsky, MD, of Houston, says he sees both pros and cons to using the femtosecond. “It definitely makes it easier to fragment a very hard lens,” he says. “I use it for astigmatism. I didn’t find the main incision or paracenteses [creation] helpful.”
G. Peyton Neatrour, MD, of Virginia Beach, says he uses the Zepto for capsulotomies, and comments: “I like the precision, accuracy and safety that surpasses human hands.”
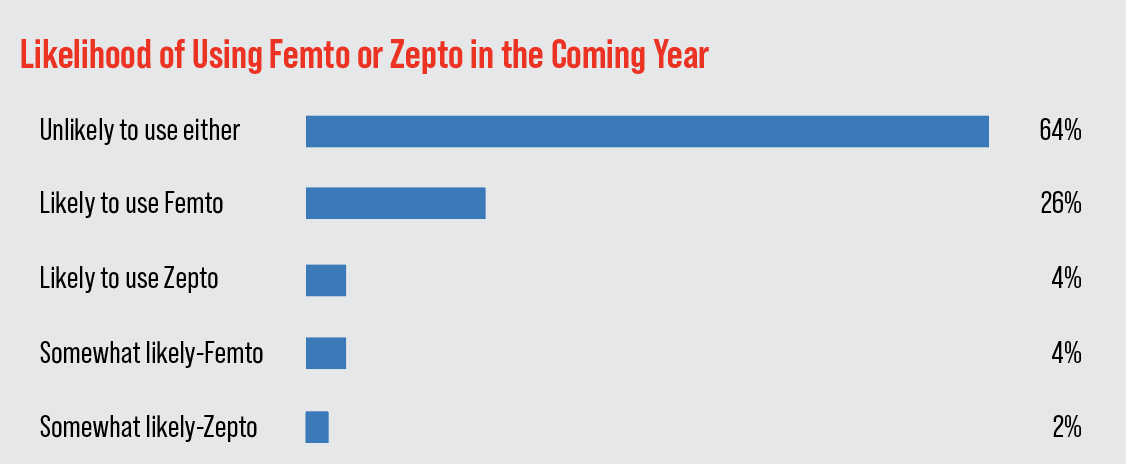
Looking down the road, of the surgeons who don’t use either the femto or the Zepto, 26 percent say they’re “likely” to begin using the femtosecond for some aspect of the surgery in the coming year, and 4 percent say they’re “somewhat likely” to do so. Four percent say they’re “likely” to use the Zepto for capsulotomy creation, and 2 percent say they’re “somewhat likely” to use it.
• Intraoperative wavefront aberrometry. On this year’s survey, 47 percent of the surgeons use this technology (ORA System, Alcon) to help them place the appropriate IOL. Fifteen percent say it’s “excellent,” 21 percent think it’s “good,” 8 percent say it’s “fair,” and 3 percent deem it “poor.”
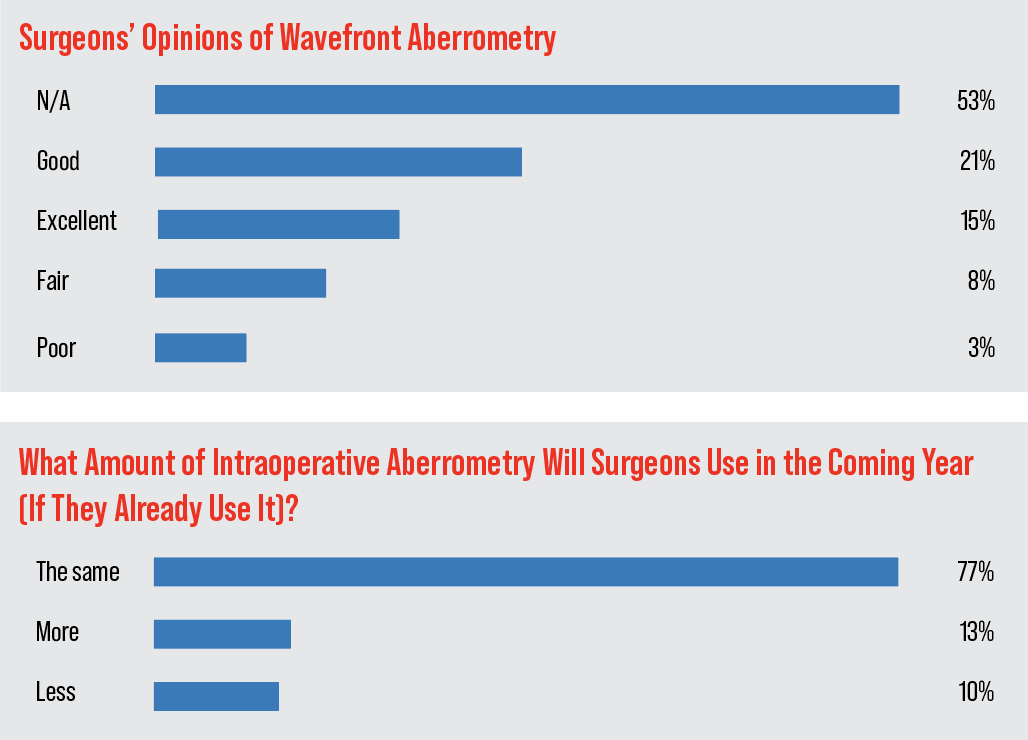 |
“It’s helpful to better determine the spherical power of the IOL in real time,” says a Michigan surgeon. “It’s also helpful with aligning toric IOLs.” A surgeon from Montana says the technology is “good,” but it’s not foolproof, and you still need to be ready to do some surgical decision-making. “I’ve used it for more than eight years,” he says. “Once an incision is made on the cornea and the incision is manipulated during phacoemulsification/use of instrumentation, the ORA measurements are affected… sometimes significantly. Like they say about bear spray, ‘it’s not brains in a can.’”
Opinions on Meds
Surgeons shared their perspective on maintaining an adequate pupil during surgery, as well as managing postop inflammation and preventing infection postop.
To promote a wide pupil during their procedures, the largest proportion of surgeons on the survey use an intracameral injection of epinephrine and lidocaine (49 percent). Twenty-three percent use Omidria (phenylephrine and ketorolac injection, Omeros), which is up from 17 percent on last year’s survey. Seventeen percent use some sort of mechanical means, such as the Malyugin ring, the I-Ring, or a Kuglen hook/Beckert rotator combination.
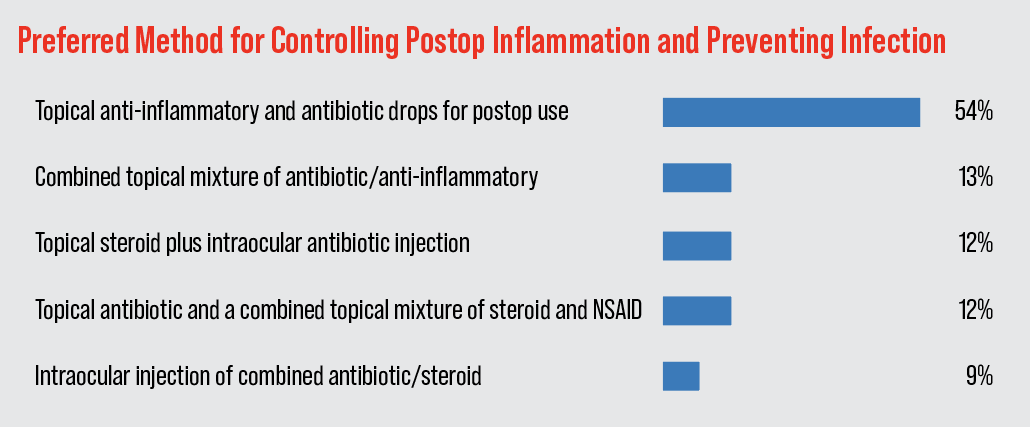 |
Topical is still tops when it comes to managing patients postop, say surgeons. Fifty-four percent of the respondents say they use separate topical anti-inflammatories and antibiotics postop. Jon S. Jacobson, MD, of Scottsdale, Arizona, says the all-topical route “is safe and effective.”
The percentage who use a combined topical mixture of these drugs was the next most popular option, chosen by 13 percent of surgeons. The breakdown of the popularity of the options appears in the graph above. Interestingly, an intraocular injection of combined antibiotic/steroid was more popular this year compared to last (9 percent vs 4 percent in 2022).
“The hospital forbids compounded drops,” says New Jersey’s Dr. Prystowsky. “The surgicenter where I operate allows intracameral Trimoxi.”
Breaking Up the Nucleus
Surgeons also shared their favorite methods for attacking the nucleus.
Quadrant division led the way again this year, but not by as much as in years past; 37 percent of the surgeons chose it, compared to 46 percent last year. “I have the most comfort level [with quadrant division] after doing it for many years,” says Dr. Prystowsky. “[I like its] safety, and the fact that it’s dependent on instruments that are available in the facility, both at the hospital and in surgicenters.”
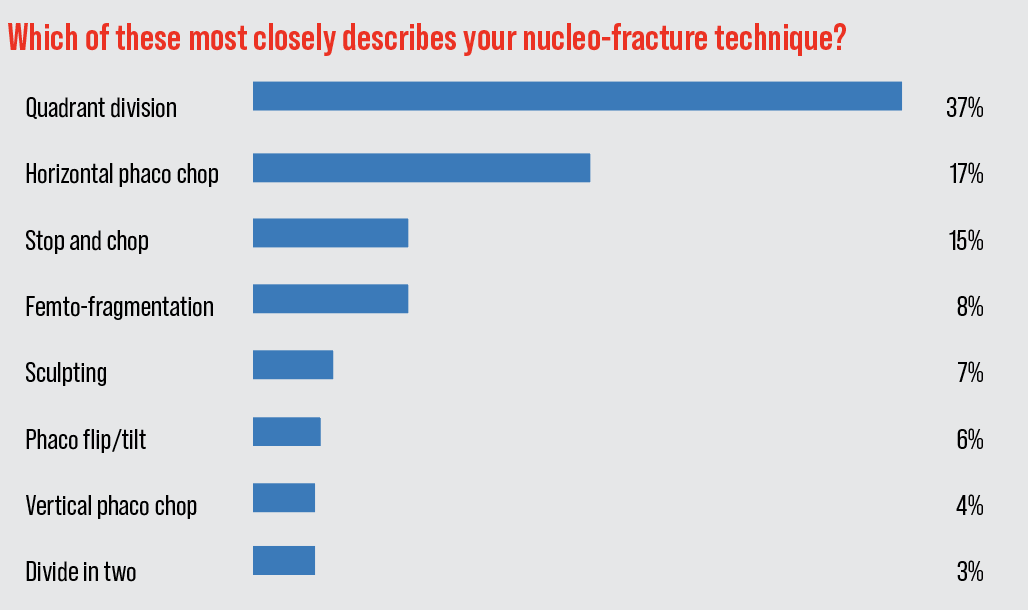 |
Though it may take a year or so to say this is a true trend, horizontal phaco chop made a big jump in the rankings, going from just 5 percent of surgeons choosing it last year to 17 percent on this year’s survey. “It’s useful for any density nucleus,” says Colorado Springs surgeon Steve Dewey. “It puts far less stress on the zonules than a technique involving trenching.”
The next most popular approach is stop-and-chop, chosen by 15 percent of the respondents. The full results of surgeons’ nucleo-fracture preferences appear in the graph above.
Pearls
Surgeons also shared their best pearls. Some of them include:
- Consider ECCE for rock hard nucleus cases.
- If there’s even minimal wound leakage at the end of the case, put in a 10-0 Vicryl suture. It’ll dissolve in four to six weeks, and any induced cylinder will resolve without further treatment.
- Adapt your technique to each case. One size does NOT fit all.\No premium intraocular lenses in super high anxiety/Type-A personality patients!
- Anchor your hands on the patient’s face so you can move in sync with him.
- Be prepared by knowing the AXL, ACD, CCT and lens thickness. It’ll guide your phaco settings and make surgery safer, barring zonular dehiscence, which you’ll feel during the capsulorhexis.
- Make sure nuclear hydrodisection is performed adequately to make the remaining surgery much more straightforward.
- Use dispersive viscoelastic to prevent PC tears. Re-inject frequently, especially in the later stages of nucleus removal.
- Be patient.
- Keep it simple.
This article has no commercial sponsorship.




