 |
For better or worse, patients often go online to gain medical information or to make decisions about their condition. Therefore, it’s necessary for patient-oriented websites to be readable to the layperson or have complementary patient education video content to promote better health literacy. Website accessibility accommodations are especially important to cataract surgery candidates, as these patients already have vision difficulties and may have other medical comorbidities due to older age that may limit their access online.
Researchers based at The Wilmer Eye Institute at Johns Hopkins University School of Medicine in Baltimore have determined that accessibility and readability measures need to be improved among informational patient-oriented health websites, especially for cataract surgery.1 The average reading level of the top 100 patient-oriented websites regarding cataract surgery was approximately the 12th-grade level, which is far above the American Medical Association-recommended 6th-grade level and the average 8th-grade reading level in the U.S. population.
Wilmer cornea specialist Esen Akpek, the study’s corresponding author, credits her mentees at the Institute for the idea. “I practice at a tertiary-care center and, most of the time, patients are somewhat educated about their condition—but not always,” Dr. Akpek says. “So, it’s a different kind of skillset to provide them with information in a meaningful, understandable way, and to not scare them about surgery, but at the same time inform them about the surgery’s risks. Also, we have to be able to recommend a lens implant while not influencing them to choose one implant over another.
It’s an art, actually, which I hadn’t realized until I started mentoring students and residents. These individuals sometimes take time off from their education and come and work for me for a year or two.
“It was actually their idea,” Dr. Akpek continues, “because I sometimes have trouble explaining things without using medical terms too much, to explain using lay language to present an accurate representation of pros and cons and the like.”
Dr. Akpek says accurate explanations can also counteract any wrong information patients may have learned about eye surgery.
“A lot of the time, patients have done some Googling, and come in with misinformation or a misunderstanding,” she says. “So, we wondered if the available information was understandable. Is the information suitable for the purposes of education? That’s when we started looking at the availalability of online information.”
The study, published in Ophthalmology, performed an incognito search for “cataract surgery” using a search engine. The top 100 patient-oriented cataract surgery websites that came up were included and categorized as institutional, private practice or medical organization according to authorship. Each site was assessed for readability using four standardized reading grade-level formulas. Accessibility was assessed through multilingual availability, accessibility-menu availability, complementary educational-video availability, and conformance and adherence to guidelines for web content accessibility. The team sorted 32, 55 and 13 sites to institutions, private practice and other medical organizations, respectively. These categories included the following sources of information:
• Institution: academic centers, medical societies and governmental websites;
• Private practice: for-profit medical entities providing care to patients;
• Other medical organizations: standalone health information service websites, health magazines, insurance companies and pharmaceutical or device firms).
The overall mean reading grade was 11.8, with higher reading levels observed in private practice websites compared to institutions and medical organizations combined (12.1 vs. 11.4). Fewer private practice websites had multiple language options compared to institutional and medical organization websites combined (5.5 percent vs. 20 percent). More private practice websites had accessibility menus than institutions and medical organizations combined (27.3 percent vs. 8.9 percent) Notably, 85 percent of websites violated what’s called the perceivable principle, which is the notion that “information and user interface components must be presented in a way that all users can recognize and understand,” according to experts in accessibility.
“These issues may negatively impact patient experiences by leading to medical misinformation, surgical hesitancy or refusal, increased frustration and poor satisfaction post-surgery,” the researchers wrote in their paper. “Cataract surgery can be made more equitable and understandable within the general population by providing usable online information to prospective recipients.”
Dr. Akpek says the accessibility of the information is even more critical in the ophthalmic realm, as opposed to patients researching heart surgery or information from another specialty, since the patients are dealing with vision issues. “It’s especially important to us as ophthalmologists because we deal with vision,” she says. “So, if the contrast or font size can’t be modified for patients with issues such as cataract or AMD, then the simple availability of the information may not mean that much, even if it’s accurate, because patients simply may not be able to view it.”
She adds that, in contrast to tertiary-care patients who usually come in armed with some knowledge of their condition and potential surgery, improvements in patient education could really make a difference for patients earlier in their eye-care journey. “Being able to educate patients in this way is key, especially in primary eye-care settings like optometry and general ophthalmology,. Good websites should be able to inform the patients about what cataracts are, how to instill eye drops after surgery, and such, which would save chair time for me, allowing us to talk more about such things as the risks and benefits of surgery.”
Dr. Akpek says that, if a practice could do one thing to help make their online information more useful, she thinks it would be a good thing for schedulers to provide online links to patients prior to them coming in. “Not everyone will read it, or understand it, but if some of them have some preliminary fund of knowledge before they come in for an evaluation, I think that would be helpful for both sides,” she says. “And if the information we’re asking the patient to read is accurate, understandable and adjustable for their disabilities—visual and otherwise—I think that would be even more awesome.”
The team proposed that an area of future research may include surveying cataract surgery candidates to evaluate whether these websites provide information that adequately addresses their needs.
1. Lin MX, Li G Cui D, et al. Usability of patient-education oriented cataract surgery websites. Ophthalmology. October 16, 2023. [Epub ahead of print].
Orasis Presbyopia Drop Gets Approval
Come the new year, ophthalmologists will have another medical option for presbyopia. Soon to join Allergan’s Vuity (pilocarpine 1.25%) on the market is another pilocarpine drop, this one at a lower concentration of 0.4%. Called Qlosi (pronounced “CLOH-see”), the drug’s FDA approval was announced in mid-October by Orasis Pharmaceuticals. The new drop is approved for daily or b.i.d. dosing as needed for patients with presbyopia. Given Qlosi’s lower concentration, clinicians will be curious to see whether it results in fewer adverse effects than Vuity. Another potential plus: the formulation is preservative-free, Orasis says.
In the drug’s two Phase III clinical trials, involving more than 600 patients, Orasis reports that the pupil-constricting drop demonstrated efficacy 20 minutes after administration and—with the benefit of a second dose two to three hours after the first—can last up to eight hours, as measured on day 15. Both trials also met their primary and key secondary endpoints on day eight, achieving a gain of at least three lines in distance-corrected near visual acuity without losing one line or more in distance visual acuity. The company adds in its press release that the drop had no impact on night vision.
Headache and instillation site pain were among the most common treatment-related adverse events, affecting 6.8 percent and 5.8 percent of participants, respectively. Moderate treatment-related adverse events were reported by 1.3 percent of participants, and all other adverse events were mild, the company reports.
Nick Mamalis, MD, co-director of the Intermountain Ocular Research Center at the University of Utah’s Moran Eye Center, says he expects patients’ and physicians’ experience with Vuity will inform their use of the new drop. “I think what will happen is it’ll be the same group of people who will benefit,” he says. “What I learned [with Vuity] is that a lot of my wife’s friends, now in their 60s, wanted to use it and insisted I write them prescriptions. But then it didn’t do anything. People in that older age range don’t have accommodative reserve and also have smaller pupils. So a medication like a low-dose pilocarpine that works to shrink the pupil to increase the range of focus, in these patients who have a smaller pupil to begin with, it keeps the potential for increasing that range lower. I think people realized that if you have some accommodative reserve, then you can get results from it. When they do the studies, though, they do get a good response from patients in the age range where you’d expect to see it—40s and 50s—and I think with a low dose of the pilocarpine, the side effects are low. With these low-dose pilocarpines, you don’t get headache from accommodative spasm or some of the other symptoms you’d get with the old high-dose pilocarpine. I think the experience [with this new drug] will be similar to the previous one: These drops will work well in younger presbyopes rather than older presbyopes.”
Orasis says the drug will be commercially available in the first half of 2024, Orasis says.
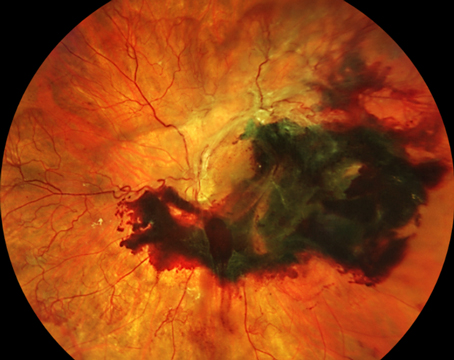
Anti-VEGF for AMD in the Setting of DR
The relationship between diabetes and age-related maculaar degeneration is both complex and controversial. Even though some authors have reported diabetes as a risk factor for AMD (i.e., especially for wet AMD), other studies didn’t find any correlation between these two disorders. Importantly, diabetic retinopathy and wet AMD share treatment options, as anti-VEGF intravitreal injections are used to treat both AMD-associated macular neovascularization and diabetic macular edema.
A recent optical coherence tomography angiography study conducted in Italy aimed at assessing whether the presence of diabetes and diabetic retinopathy could impact the baseline characteristics of treatment-naïve AMD-associated type 1 macular neovascularization.1 Also, the researchers assessed longitudinal changes occurring in type 1 macular neovascularization during anti-VEGF therapy in order to understand whether the presence of diabetes and diabetic retinopathy may impact such modifications. The team found that mild nonproliferative diabetic retinopathy eyes responded differently to wet AMD treatment. In particular, the diabetic group showed limited contraction of the macular neovascular lesion area after intravitreal therapy.
The study enrolled 50 treatment-naïve eyes with a diagnosis of wet AMD and type 1 macular neovascularization, of which 20 were affected by mild diabetic retinopathy. En face OCTA were examined for the macular neovascular lesion area (mm2), the macular neovascularization flow area (mm2), the central macular thickness and the best-corrected visual acuity. The OCTA acquisition was performed before the aflibercept loading phase (consisting of three monthly injections) and then one month after the last injection of the loading phase.
All morpho-functional parameters showed a significant change at the end of the study period compared with values in both groups. Furthermore, the researchers found a greater reduction of macular neovascularization after the loading phase in eyes without diabetic retinopathy. In the remaining parameters, no significant changes were found between the two groups. The study revealed a smaller reduction of macular neovascularization area after the loading dose of anti-VEGF therapy in eyes with diabetic retinopathy.
The researchers proposed two co-existing mechanisms behind the finding: (1) the presence of diabetic retinopathy in eyes affected by wet age-related macular degeneration could lead to higher levels of vascular endothelial growth factor, and therefore a worse response to treatment in terms of macular neovascularization downsizing; (2) diabetic retinopathy is known to be associated with choroidal hypoperfusion that might contribute to the macular neovascularization persisting as a mechanism of defense to the retinal pigment epithelium and outer retina ischemia.
“These results provide evidence that the diabetic retinopathy impact might play a fundamental role not only in the development and progression of macular neovascularization but also in evaluating reaction to anti-angiogenic therapy,” the researchers concluded in their paper. “Future larger studies using swept-source optical coherence tomography angiography and longer follow-up are needed to support our preliminary findings.”
1. Viggiano P, Landini L, Grassi MO, et al. Effects of diabetic retinopathy on longitudinal morphological changes in AMD-associated type 1 macular neovascularization. Sci Rep 2023;13:1:16337.
CORRECTIONS In the September article, “Dry-Eye Treatments Continue to Evolve,” the maker of Ivizia was incorrectly listed as Similasan. The drug’s maker is Thea. In the October article, “Tarso-conjunctival Flaps for Severe Keratitis,” author David Morcos was incorrectly identified as David Morcos, DO. His correct title is David Morcos, BA. Review regrets the errors. |