According to researchers in Canada and Singapore, recessing or resecting Müller's muscle and levator aponeurosis but leaving a central pillar of Müller's muscle intact, occasionally including a temporal tarsorrhaphy or superior tarsal strip where needed, and performing tissue dissection with a hot-wire cautery instrument, is effective even in severe cases of eyelid retraction. The 10-year retrospective chart review included 99 patients (161 eyelids, 62 bilateral and 37 unilateral) with a mean age of 47 years (range, 21 to 82 years). Statistical analysis was performed using an unpaired t test. The mean follow-up was 61 months.
The mean preoperative and postoperative margin reflex distances (MRD1) were 7.3 mm (range, 4.5 to 10 mm) and 4.3 mm (range, 2 to 7 mm), respectively. Eighty-nine percent (144/161 eyelids) achieved the target result of an MRD1 of 4 ±1 mm after one procedure. Fifteen eyelids (9 percent of operated eyelids) required a second procedure, and in this group, two (13 percent of reoperated eyelids) underwent a third procedure. Although bilateral cases were more likely to achieve symmetry (p=0.0071), 90 percent of either unilateral or bilateral achieved a postoperative MRD1 of 4 ±1 mm. Both mild (MRD1 of 5 to 7 mm) and severe (MRD1 >7 mm) cases of eyelid retraction achieved similar operative outcomes. In the first six months after surgery, complications included undercorrection (eight eyelids), overcorrection (two eyelids), and pyogenic glaucoma (two eyelids). None had a flattened upper eyelid contour. Late recurrence of retraction was seen in nine eyelids. Mean operative time was 16 minutes per eyelid.
Minimal complications were encountered, and upper eyelid contours were well-preserved. The use of hot-wire cautery dissection proved useful in shortening operative time. The high levels of patient satisfaction with the results further indicate the effectiveness of this technique.
(Ophthal Plast Reconstr Surg 2006;22:434-437)
Looi ALG, Sharma B, Dolman PJ.
ISNT Rule Helps Detect Glaucoma
The ISNT rule is useful in differentiating normal from glaucomatous optic nerves say researchers from
One hundred nine eyes of 109 patients were randomly enrolled in the study. Sixty-six (33 white and 33 black) subjects had normal eyes and 43 (28 white and 15 black) had glaucoma. Subjects with normal eyes were younger than those with glaucoma (46.1 ±13.6 vs 61.3 ±10.7 years; p<0.001). Sex distribution (p=.55) and refractive error (p=0.37) were similar between the two groups. Normal eyes had a shorter axial length than those with glaucoma (23.6 ±0.09 vs. 24.1 ±1.1 mm; p=0.01).
All subjects underwent complete eye examination, including achromatic automated perimetry, simultaneous stereoscopic disc photography and confocal scanning laser ophthalmoscopy. Subjects with normal eyes had no evidence of glaucoma or ocular hypertension and had normal perimetry measurements. Subjects with glaucoma had a reproducible visual field defect. The ISNT rule was assessed by masked evaluation of disc photographs at the 3, 6, 9 and 12 o'clock positions.
The ISNT rule was intact in 52 (79 percent) of 66 normal eyes and 12 (28 percent) of 43 glaucomatous eyes (p<.001). Multiple logistic regression indicated that the odds ratio for glaucoma associated with violation of the ISNT rule was 6.04 (95 percent confidence interval, 1.74 to 20.95) after adjustment for age; the study found that race was not a confounding factor in this association.
The researchers say that the results can only be applied to patients with a similar range of refractive error. They say future studies should address the use of the ISNT rule for glaucoma suspect eyes and preperimetric glaucomatous eyes.
(Arch Ophthalmol 2006;124:1579-1583)
Harizman N, Oliveira C, Chiang A, Tello C, Marmor M, Ritch R, Liebmann JM.
PDT and Avastin Treats Neovascular AMD
treatment combining photodynamic therapy with verteporfin and intravitreal bevacizumab may enhance the treatment of neovascular age-related macular degeneration by reducing retreatment rates and improving visual acuity, say researchers from
This retrospective study included 24 eyes with juxtafoveal or subfoveal choroidal neovascularization secondary to AMD. Patients were treated with PDT with verteporfin and 1.25 mg of intravitreal bevacizumab. All patients were naïve to treatment and were treated within a 14-day interval. Main outcome measures were visual acuity stabilization (defined as no change or a gain in visual acuity) and retreatment state.
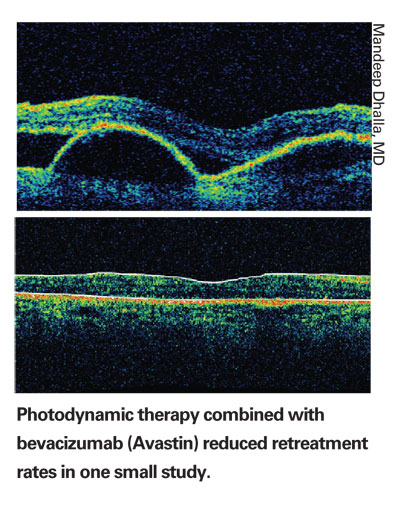
Twenty (83 percent) of 24 eyes had stabilization of visual acuity at the seven-month follow-up. Sixteen eyes (67 percent) showed an improvement in visual acuity. Mean improvement in visual acuity (n=24) was 2.04 Snellen lines. Fifteen eyes (63 percent) required only a single combined treatment for CNV resolution. There were no complications, including no endophthalmitis, uveitis or ocular hypertension.
The researchers acknowledge that the study is limited by many factors, including retrospective design, small series of patients and limited follow-up time. The study affirms the need for further investigation with larger, controlled trials that will outline the appropriate treatment paradigm for approaching neovascular AMD.
(Retina 2006;26:988-993)
Dhalla MS, Shah GK, Blinder KJ, Ryan Jr. EH, Mittra RA, Tewari A.
Avastin Reduces Leakage In Diabetic Retinopathy
Intravitreal injection of bevacizumab achieved short-term reduction of fluorescein leakage from persistent active neovascularization– without loss of vision–in patients with diabetic retinopathy, according to researchers in
Patients were included in the study if they had persistent NV, defined as active NV, unresponsive to complete panretinal laser photocoagulation performed at least 4 months prior, and logarithm of minimum angle of resolution (logMAR) best-corrected visual acuity of .03 (Snellen equivalent, 20/40) or worse. Patients were excluded if they had a history of vitrectomy in the study eye, a history of thromboembolic event, major surgery within the prior six months or planned within the next 28 days, uncontrolled hypertension, known coagultion abnormalities or current use of anticoagulative medication other than aspirin.
Standard ophthalmic evaluation was performed at baseline and at weeks one, six and 12 (±1) following intravitreal injection of 1.5 mg of bevacizumab. Main outcome measures include changes in total area of fluorescein leakage from active NV and BCVA.
Fifteen consecutive patients (nine men [60 percent]; six women [40 percent]) were included and all completed the 12-week follow-up period of the study. The mean ±SD age of participants was 60.08 ±7.75 years (median, 59.5; range, 49 to 73 years). At baseline, mean ± standard error of the mean (SEM) NV leakage area was 27.79 ±6.29 mm2. The mean ±SEM area of active leaking NV decreased significantly to 5.43 ±2.18 mm2 and 5.50 ±1.24 mm2 (p<0.05, Tukey multiple comparisons post-test) at one and 12 weeks postinjection, respectively; at week six no leakage was observed. The mean ±SEM logMAR (Snellen equivalent) BCVA improved significantly from 0.90 (20/160) ±0.11 at baseline to 0.76 (20/125+2) ±0.12, 0.77 (20/125+2) ±0.11, and 0.77 (20/125+2) ±0.12 at weeks one, six and 12, respectively (p<0.05, Tukey multiple comparisons post-test). No major adverse events were observed.
The researchers suggest further studies to determine the safety and efficacy of intravitreal bevacizumab, the potential value of repeated injections, and the optimal reinjection frequency, and to compare the results of intravitreal bevacizumab with other treatment modalities for various disease entities.
(Retina 2006;26:1006-1013)
Jorge R, Costa RA, Calucci D, Cintra LP, Scott, IU.
Phacoemulsification Reduces IOP
Cataract removal by clear cornea phacoemulsification in glaucoma patients, glaucoma suspects and normal patients results in a small but significant decrease in intraocular pressure that is sustained at three years and a mean of five years, say researchers from
In this retrospective study, patients with clear corneal phacoemulsification and at least three years of follow-up were classified into three groups: glaucoma (G), glaucoma suspects (GS), and no glaucoma (NG). No patient had a history of intraocular surgery. Single factor analysis of variance, Fisher exact tests, two-tailed paired Student t tests and Kaplan-Meier analysis were applied.
Forty-eight patients (55 eyes) in the G group, 41 patients (44 eyes) in the GS group, and 59 patients (59 eyes) in the NG group were studied. At three years follow-up, IOP was significantly decreased in all groups; G decreased 1.4 ±3.3 mmHg (p=0.0025), GS 1.4 ±4.2 mmHg (p=0.004), and NG 1.7 ±3.1 mmHg (p=0.0005). At the final follow-up visit, (mean near five years for all groups) the IOP was significantly decreased in all groups, G 1.8 ±3.5 mmHg (p=0.005), GS 1.3 ±3.7 mmHg (p=0.025), and NG 1.5 ±2.5 mmHg (p<0.0001). The number of pre- and postoperative glaucoma medications in the G group did not show any significant change at three or five years (p=0.36, p=0.87). Kaplan-Meier analysis shows that at three years, 85 percent of the G group, 81 percent of GS, and 90 percent of NG had IOPs less than or equal to their preoperative IOP, with the same number of glaucoma medications or fewer. At five years, the percentages were 76, 79 and 85, respectively.
The researchers advise that cataract removal by phacoemulsification is not a substitute for a combined procedure but may be an appropriate procedure for certain patients based on medication requirements and extent of optic nerve damage.
(J Glaucoma 2006;15:494-498)
Shingleton BJ, Pasternack JJ, Hung JW, O'Donoghue MW.



