With more than three million Americans undergoing cataract surgery each year, it is one of the most common—and safest—procedures performed in the United States. And ongoing advancements in surgical techniques and intraocular lens technology support the efforts of ophthalmologists who continuously strive to ensure their patients have the best possible visual outcomes.
Maximizing outcomes depends on a number of factors and doesn’t end with the removal of the cataract and the implantation of an IOL. “The key aspects of patient satisfaction after cataract surgery today include a meticulous preoperative evaluation, judicious patient selection and a comprehensive patient education to set the appropriate postoperative expectations,” says Garden City, New York’s Eric Donnenfeld, MD, while noting that postoperative management also plays a crucial role in successful cataract surgery outcomes, and part of that is addressing patient concerns and complaints.
However, what do you do if you have run the appropriate tests and everything (i.e., the macula, IOL, cornea) looks normal yet the patient is still having an issue with their vision? In this article, we’ll explore various strategies to maximize vision after cataract surgery and IOL implantation as well as how to help their patients navigate the process.
Clinical Pearls for Surgeons
When the standard exams all come back normal, taking a step back and carefully considering how best to proceed can help ophthalmologists uncover the underlying issue and appropriate intervention. Below ophthalmologists offer advice on how they approach these cases.
If a patient isn’t satisfied with their visual outcome post-surgery, Daniel Chang, MD, of Empire & Laser in Bakersfield, California, begins by making sure he has a clear understanding of the issue. Is it quality of vision? Range of vision? Dysphotopsia?
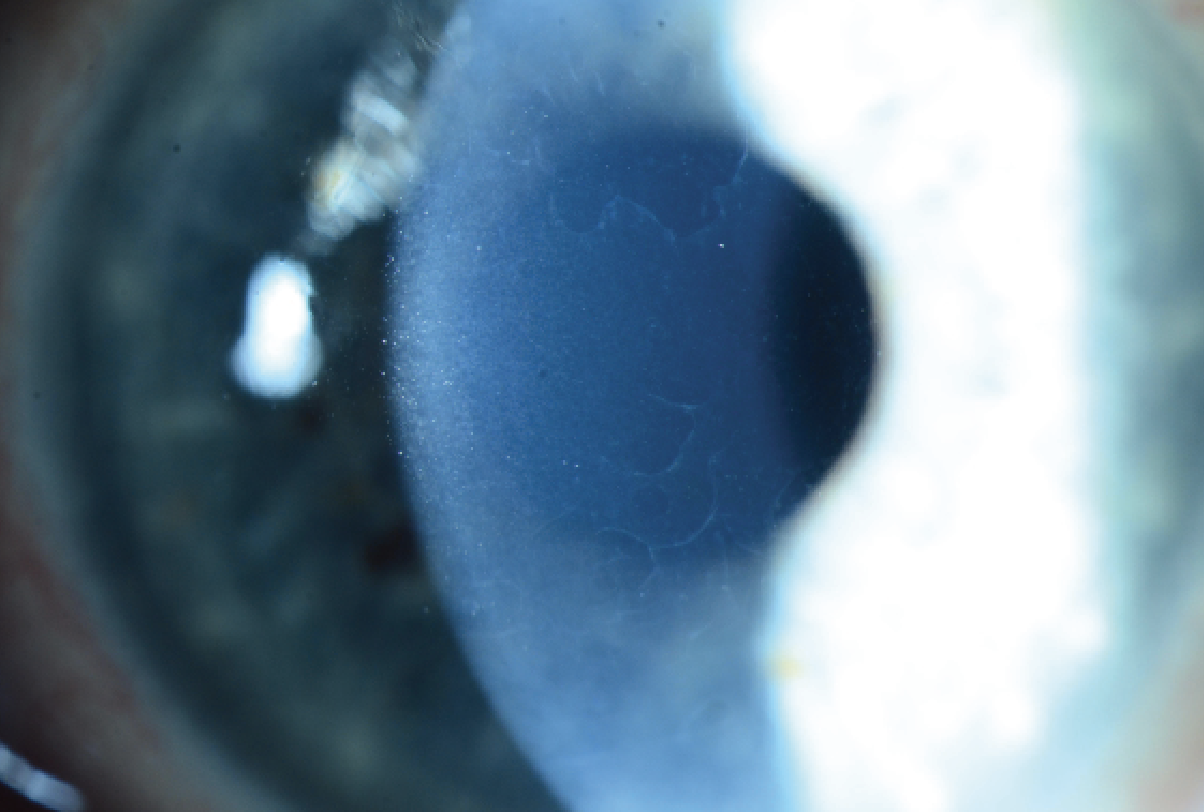 |
| A slit lamp photo of subtle epithelial basement membrane dystrophy. (Courtesy Beeran Meghpara, MD) |
To determine next steps, it’s important to get as much detail from the patients as possible. Dr. Chang will often ask questions like, “What specific thing are you doing and when does it specifically bother you?” This allows you to get a detailed picture of the problem and from there you can figure out the cause and best treatment approach.
Don’t overlook dry eye, advises Dr. Donnenfeld. “Even if the patient’s cornea looks normal, very commonly you will find irregularities that explain the vision, and I look for a history of visual fluctuation. Any time the vision fluctuates, I consider ocular surface disease,” he explains. “In addition to a visual inspection of the ocular surface, I add lissamine green to highlight any staining irregularities in the conjunctiva and provide a more in-depth evaluation of the ocular surface.”
Additionally, Dr. Donnenfeld will use topography to find slight irregularities that may be compromising a patient’s vision. “When I see these problems, I will often take a more aggressive approach to manage the ocular surface.” This includes perfluorohexyloctane (Meibo), which he has found stabilizes the surface and is a good refractive solution. Punctal plugs can also have a role as well as some low-dose steroids, he notes. “Even the mildest tear film abnormalities, which can be very easily missed, can cause significant patient dissatisfaction.”
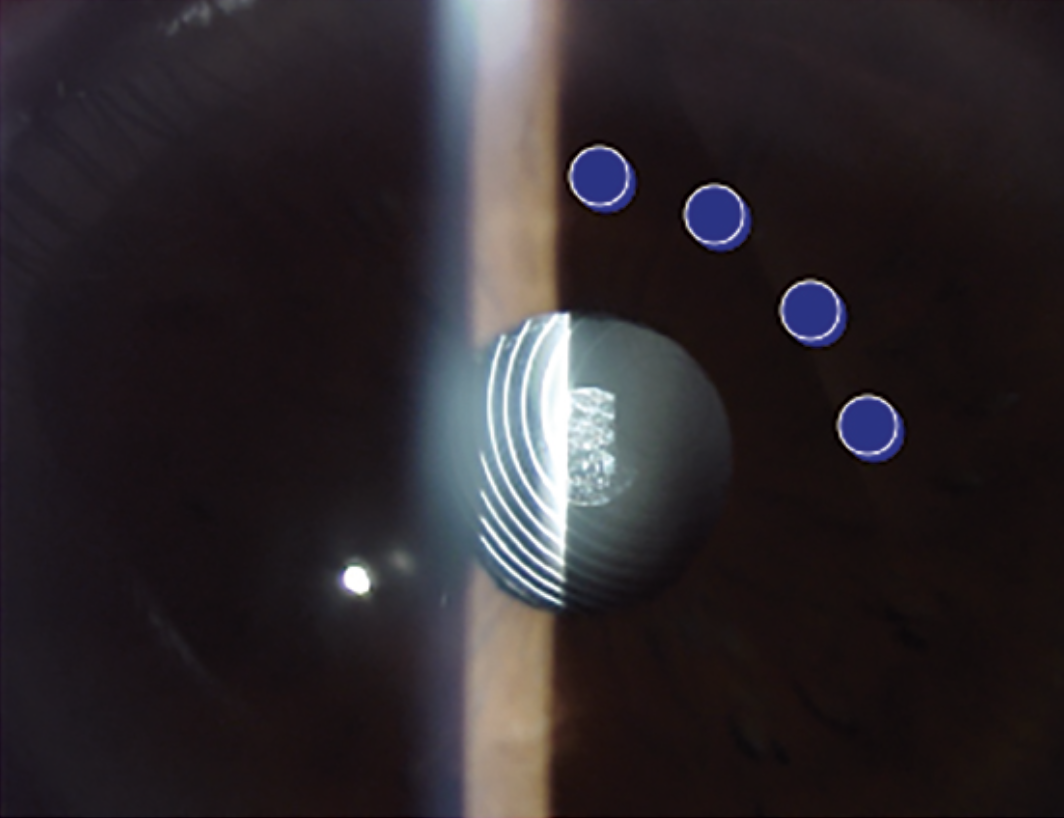 |
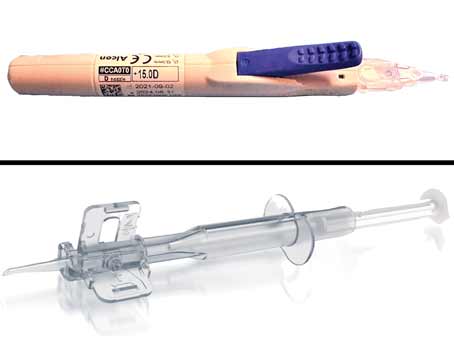
| For patients whose pupil isn’t coincident with the center of the lens, Eric Donnenfeld, MD, says laser iridoplasty can help pull the pupil over the center of the lens. He places four or five spots where he wants to move the pupil, with a setting of 500-milliwatts, 500 microseconds, 500 millijoules. (Courtesy Eric Donnenfeld, MD) |
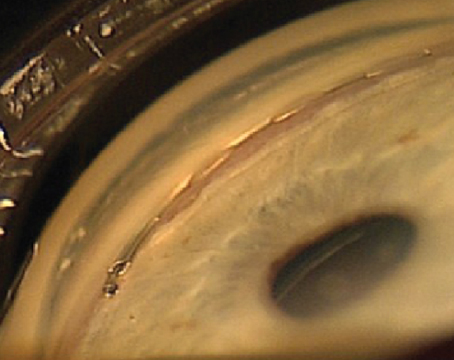
Wills Eye’s Beeran Meghpara, MD, reiterated the value of a corneal topography for these cases. “It’s very easy to miss subtle changes, especially if you’re a doctor who doesn’t specialize in the cornea. Therefore, I always perform a corneal topography on these patients, which can help pick up issues such as subtle epithelial basement membrane dystrophy that you may not be able to see or subtle areas of irregular astigmatism,” he says, noting the importance of looking at the Placido ring image when using this tool.
Dr. Meghpara will also get an OCT of the macula when trying to determine the reason behind a patient’s vision complaints. “Even if the retina appears normal, there are some changes, such as a subtle epiretinal membrane, that you can’t see when using a slit lamp,” he explains.
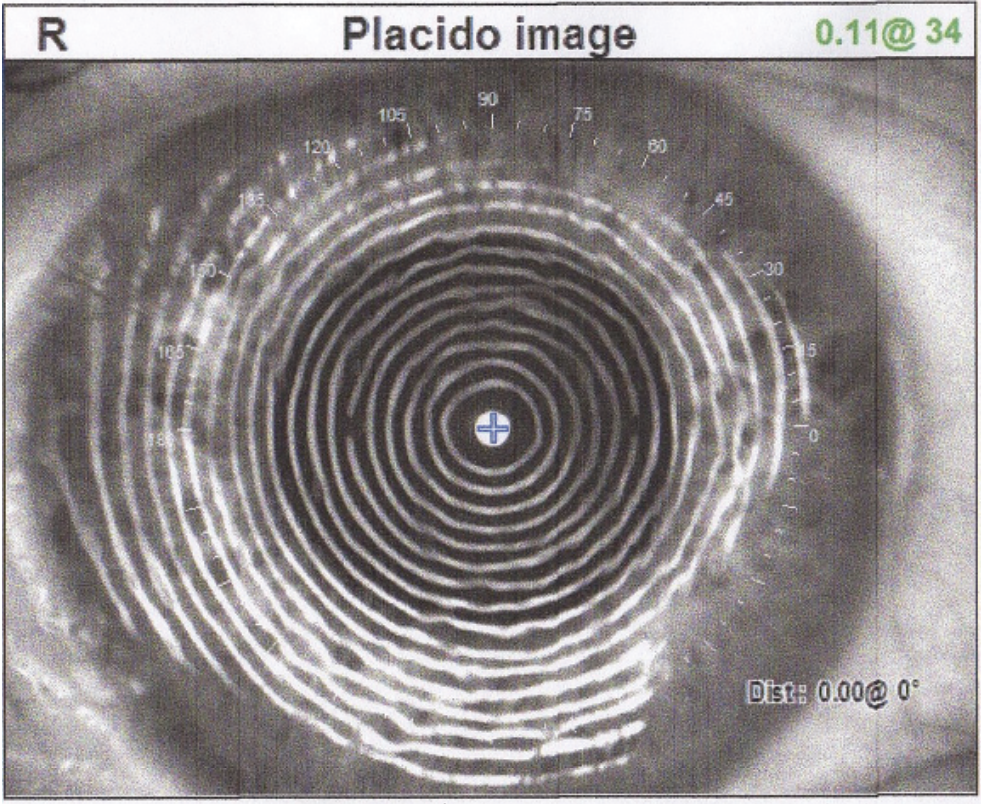 |
| A Placido ring image on topography can help pick up subtle changes on the cornea. (Courtesy Beeran Meghpara, MD) |
A very commonly overlooked problem, according to Dr. Donnenfeld, is one that wasn’t always on his checklist either. “In the past I didn’t always include the vitreous in my standard workup, but what we’re seeing now is that a lot of patients, particularly those with multifocal lenses, who have even mild vitreous opacification can have significant loss of quality of vision,” he says, while emphasizing the need for a dilated eye exam.
“Vitreous floaters are an often underdiagnosed reason for patient dissatisfaction after multifocal IOL surgery,” adds Dr. Meghpara. “In our practice, we’ll refer patients to a retinal surgeon for vitrectomy. Afterwards, patients are very grateful and happy with the results. Some ophthalmologists may opt to address floaters with an office-based approach, such as a YAG laser.”
When addressing visual concerns post-surgery, Dr. Meghpara suggests tools like iTrace can be helpful. “This diagnostic tool performs both corneal topography and wavefront aberrometry,” he says. “If you conduct this test on a patient after cataract surgery, the image quality should be excellent (9 or 10 on a scale of 10). However, if that image quality is low, say a 5 or 6, but everything looks crystal clear then you are missing something. Oftentimes, that is the vitreous.”
Another easily missed abnormality, notes Dr. Donnenfeld, is related to the angle kappa—the angle between the pupillary axis and the visual axis. “When the pupils aren’t coincident with the central lens that will induce coma, glare and some halo as well.”
In those cases, when other options have been exhausted, Dr. Donnenfeld will perform an argon-laser iridoplasty. “I can actually put laser spots onto the iris and pull the pupil over the center of the lens to make the lens more productive. Using a 500-milliwatt, 500 microsecond and 500 millijoule procedure, I place four or five spots in the area of the iris where I want to move the pupil. So, if the pupil is decentered temporally, I place the spots nasally and you can move the pupil very effectively into the area.”
Refraction is another key component, notes Richard Davidson, MD, of Aurora, Colorado. “Our team will always conduct a thorough eye exam. This includes visual acuity and refraction. We will refract every one of these patients and really try to nail down a good refraction because even if someone is ‘20/20,’ they still may have a little residual astigmatism, for instance, and that may be enough to bother them.”
Another consideration for surgeons is when additional procedures, such as a YAG laser capsulotomy or PRK enhancement, are warranted. For example, Dr. Davidson recently saw a patient who was one-week postop in her right eye and three-weeks postop in her left eye. She has multifocal lenses and was happy with the vision in her right eye but was complaining of blurriness in her left.
“Based on our discussion, this was not a lens adaptation issue,” he says. “We refracted the left eye and even with refraction the vision quality wasn’t as good as she wants it to be.
“I know she doesn’t have any macular edema,” he continues. “So, I looked at her capsule and she’s got a little wrinkling. It’s not a lot but enough that it can drop her vision enough, especially compared to the other eye. Therefore, I recommended a YAG laser capsulotomy. We know that with patients who have multifocal lenses there’s going to be a lower threshold to do a YAG compared to someone with a monofocal lens.”
Dr. Davidson notes that it can be challenging to determine if, and when, these types of interventions are necessary. This is particularly true when they have only had surgery in the first eye. Are they unhappy with the lens? Are they unhappy because they have a cataract in the other eye? Are they unhappy because they have posterior capsule opacification and need a YAG?
“This is always one of the surgeon’s most frustrating and challenging dilemmas,” says Dr. Davidson, while adding that there is no one-size-fits-all approach. “It really comes down to a variety of factors, including how the patient did immediately postop, how bad the cataract is in the other eye, do they have a lot of anisometropia, etc. If the patient is happy with the type of lens and I’ve done everything else, I’d consider a YAG capsulotomy.”
When it comes to PRK enhancement, Dr. Davidson waits a minimum of six weeks before considering it. “I want to see how they’re functioning as well as make sure that the lens has settled in and that they have consistent refractive error,” he explains. “If we’re going to move forward to a PRK enhancement, I want to have a complete picture to ensure we’re providing our patients with the approach that best fits their individual needs.”
Determining if a lens exchange is the best option is also on the table, surgeon say. “There can be a temptation to just do a treatment, such as a YAG laser capsulotomy when the capsule is actually quite clear, because a lens exchange is a much more involved procedure. However, there are times when it may be necessary,” says Dr. Chang.
If you’ve done everything you can—and ruled out other issues—and the patient just isn’t happy, for whatever reason, with the lens, Dr. Meghpara suggests discussing a lens exchange. “Sometimes you just have to bite the bullet and acknowledge that this lens is not perfect,” he says. “While, for instance, multifocals work well for the majority of patients, in some patients they’re just not well-tolerated.”
This holds true for monofocal lenses as well, he notes. “Perhaps your patient is experiencing dysphotopsia such as shadows, streaks and starbursts and you’ve done everything you can to address the problem. This is another situation that could be attributed to the lens and, while uncommon, this can happen with an IOL placement.”
In these cases, Dr. Meghpara would offer a lens exchange as long as their symptoms and dissatisfaction can clearly be attributed to the lens. “On the other hand, if you can’t explain their symptoms and their unhappiness by the lens, we won’t simply do a lens change and hope that it’ll improve a patient’s vision because there are risks associated with that procedure.”
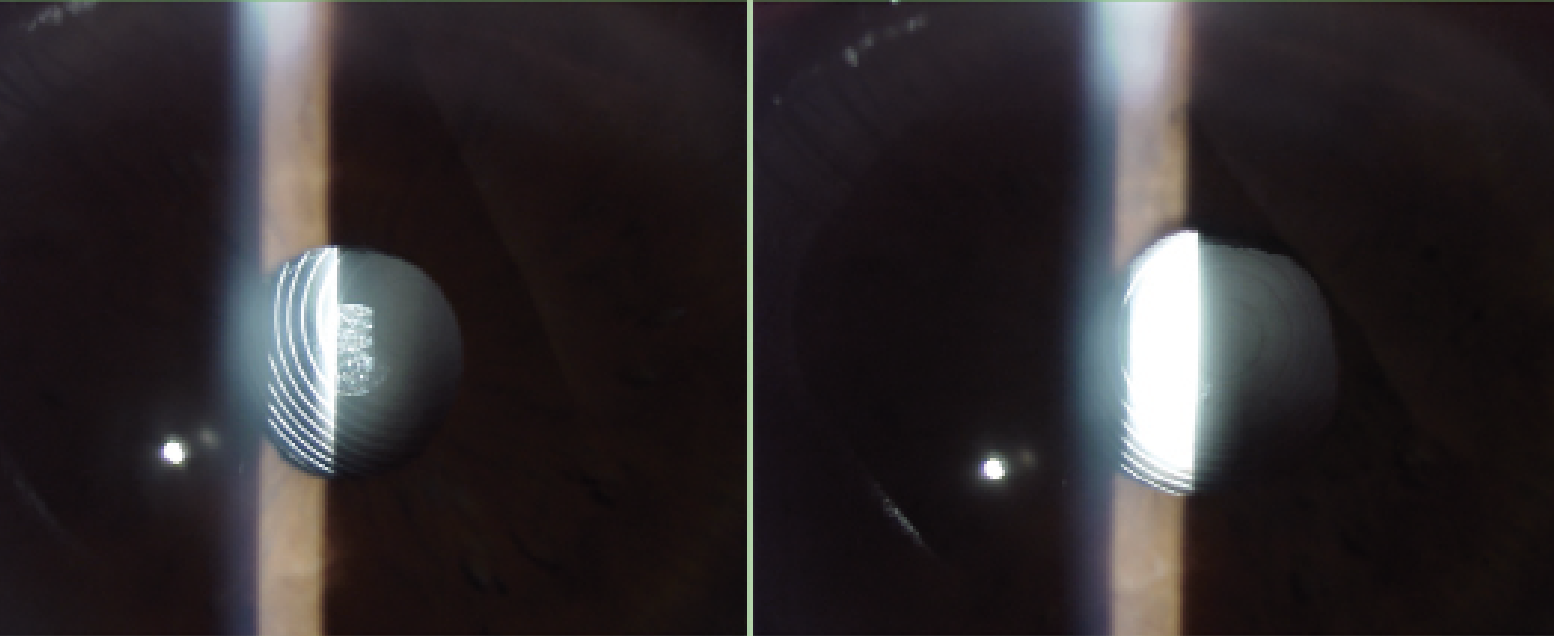 |
| The eye in the previous figure before laser iridoplasty (left) and after (right) showing the pupil has moved to a position that allows the center of the lens to be more coincident with the center of the pupil. |
Expectations & Education
Beyond taking the appropriate clinical action, success also depends on how you approach your patient and respond to their concerns. “Don’t dismiss their complaints,” urges Dr. Davidson. “Try not to get defensive or frustrated. I always do my best to reassure patients and validate their concerns, letting them know that I am there to help and will do everything I can to address the problem.”
Fostering understanding and cooperation with your patients depends—in large part—on education and expectation management. Ophthalmologists must communicate openly with their patients during the entire cataract surgery process from the first preoperative appointment throughout the postoperative stage.
“Setting expectations in advance is critical,” says Dr. Meghpara, who encourages his patients to have someone with them during the evaluation and also sends them home with a written record of the key discussion points. “Help your patients understand what’s realistic and what isn’t. I also avoid absolutes such as ‘you’ll never have to wear glasses again.’ ”
“It’s important to remember that, in addition to the technical and clinical aspects of cataract surgery, there’s a personality and expectation component that must be managed as well,” Dr. Chang concludes. “We have to be prepared to problem solve and manage any challenges that arise to achieve the best possible visual outcomes for our patients.”
Dr. Chang (http://www.empireeyeandlaser.com) consults for Johnson & Johnson Vision and Carl Zeiss. Dr. Davidson consults for Zeiss, Johnson & Johnson Vision, Alcon and Centricity Vision. Dr. Donnenfeld consults for Allergan, Alcon, Bausch & Lomb and Johnson & Johnson Vision. Dr. Meghpara reports no relevant disclosures.