 |
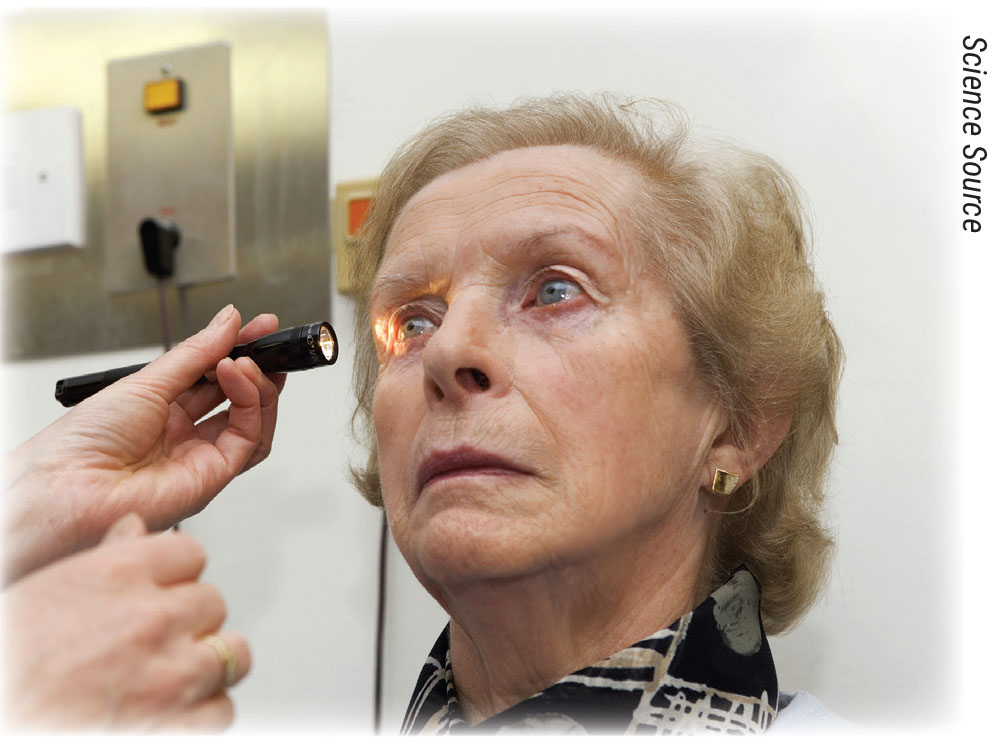
The suggested workforce-to-population ratio required for adequate delivery of neuro-ophthalmology services has been estimated to be one specialist per 1.2 million people. However, in 2022 only eight U.S. states met this threshold; in the worst-served areas, six had no neuro-ophthalmologists in the entire state. With increasing outpatient demand, and the subspecialty’s scarcity, one new study wanted to determine what the typical presentations to the emergency department for related issues look like.
The prospective study published in Ophthalmology included one academic care institution’s ED and inpatient neuro-ophthalmology consultation patterns and patient outcomes over one year.1 Of the 494 consecutive adult consultations, 49 percent took place at night or on weekends. Of the emergency consults (65 percent), 39 percent of these occurred during weekdays, 39 percent on weekends and 22 percent on weekends/holidays. Of 322 ED consultations, 70 percent presented with a chief neuro-ophthalmic complaint.
Referrals to the ED by health-care professionals were primarily made by eye-care specialists (76 percent, 196 patients). Most commonly encountered questions for emergency referral were due to papilledema at 23 percent and vision loss at 22 percent. A sizable 68 percent had a final active neuro-ophthalmic diagnosis, 69 percent had high or very high complexity and 44 percent needed admission.
Of the remaining 172 inpatient consultations, most were requested by hospitalists, including neurologists (41 percent) and oncologists (12 percent) for vision loss (25 percent) and eye movement disorders (20 percent), as well as neurosurgery (33 percent) to examine for mass or preoperative evaluation (11 percent). Active neuro-ophthalmic diagnosis was confirmed in 67 percent of patients, and a striking 90 percent of cases found neuro-ophthalmic assessment appropriate to make a diagnosis or evaluate for ophthalmic manifestations of disease. Follow-up with outpatient neuro-ophthalmology was required in 59 percent of patients.
The study authors note that overall, 61 percent of patients were diagnosed with a life- or vision-threatening pathology. Of the 49 percent of consultations occurring during off-hours, only 25 percent of these were urgent—highlighting “the paradoxical relationship between the additional burden generated by these unscheduled urgent neuro-ophthalmology consultations and the genuine need for these patients to be examined by a neuro-ophthalmologist, to whom limited access generates more such consultations.”
Driving the spikes in neuro-ophthalmology referrals or consultations are factors of delayed consultations resulting in diagnostic errors, increased cost and worse outcomes, made worse by associated risk for litigation for the provider if not done promptly. Further motivation for patient referral to hospitals than outpatient clinics is that ED or hospital evaluation is time efficient, which allows for immediate multidisciplinary care and testing which may be delayed otherwise with outpatient settings.
To deal with the rising rates, the authors propose that increasing the number of available outpatient neuro-ophthalmologists may be one solution. They also propose that “there is a need for expanded development and utilization of technological and diagnostic aids such as nonmydriatic fundus cameras in EDs as well as telehealth delivery processes for integration into health-care settings. Finally, creating and implementing standardized neuro-ophthalmology ED and hospital protocols for commonly encountered presentations and diseases should facilitate rapid diagnosis and treatment of common neuro-ophthalmologic disorders.”
1. Smolar ALO, Ray HJ, Dattilo M, et al. Neuro-ophthalmology emergency department and inpatient consultations at a large academic referral center. Ophthalmology. August 4, 2023. [Epub ahead of print].
Apellis Gives Update on Syfovre Safety Issues
On the heels of several class action lawsuits filed against it as a result of reported safety events involving Syfovre (pegcetacoplan injection), Apellis Pharmaceuticals provided an update on company-supplied injection kits and an update on events of retinal vasculitis reported in real-world treatment with Syfovre for geographic atrophy secondary to age-related macular degeneration.
According to Apellis, eight events of retinal vasculitis (five occlusive, three non-occlusive) have been confirmed. The last confirmed event of retinal vasculitis occurred on June 20. There are also two other cases of unconfirmed retinal vasculitis from May and August.
Here is an update on the injection kits from the company:
As part of the company’s investigation into real-world safety events, internal structural variations were identified in the specific 19-ga x 1.5-inch filter needle included in certain injection kits. Filter needles are used to withdraw treatment from the vial when preparing for an injection procedure. A causal relationship has not been established between the structural variations in this 19-ga filter needle and the rare events of retinal vasculitis in the real world. The company recommends that practitioners immediately discontinue use of any injection kits that contain the 19-ga filter needle and use injection kits with the 18-ga filter needle, which are already in distribution. While injection kits previously contained one of two types of filter needles (either 18- or 19-ga), Apellis is now exclusively distributing injection kits with the 18-ga filter needle.”
Durango, Colorado, retina specialist Sara Haug says she’s following the company’s guidance, but that others might seek other options. “I can’t imagine the filter needles were the culprit but I have switched to using the 18-ga filter needle they suggest,” she opines. “I have also not stopped using Syfovre due to the cases of vasculitis, since the number of patients having this complication has been so low. Compared to brolucizumab which had a 1 to 2 percent complication rate, the complication rate so far with Syfovre is around 0.01 percent, I believe. I have colleagues who have stopped using Syfovre, however, due to the complications, and haven’t restarted even with the information about the filter needle. Honestly, it’s a bit hard to know what to make of it all, and I’m guessing a lot of us will switch to Izervay, as that is now approved.”
Weak Relationship Between Dry Eye Signs and Symptoms
The list of potential ocular manifestations associated with dry eye disease (DED) are non-specific, comprising redness, burning, stinging, foreign body sensation, photophobia and pruritis. While DED diagnosis is dependent upon reports of ocular symptoms and measurements of signs, literature has not clearly demonstrated a link between signs and symptoms. One new study assessed this need by determining correlations among symptoms and signs of dry eye in the Dry Eye Assessment and Management (DREAM) study.1
Moderate to severe dry eye was assessed in a total of 535 patients, using the Ocular Surface Disease Index (OSDI) for symptoms. Four DED signs were tested in both eyes, including conjunctival lissamine green staining, corneal fluorescein staining, Schirmer’s testing and tear breakup time following standard protocol at baseline and follow-up visits at three, six and 12 months.
The researchers found OSDI scores at baseline didn’t correlate with signs, but OSDI subscale score of ocular symptoms was weakly associated with corneal staining score and Schirmer test score. There were correlations among the four signs. Correlations among changes in signs and symptoms were weaker, with the highest correlation being between change in conjunctival staining and corneal staining. Overall, the results yielded low correlation of DED symptoms with signs, even weaker correlation among changes in symptoms and signs, but low to moderate correlation among the four signs.
The study researchers, as part of their discussion, relay that the weak associations observed may be due to comorbidities that could increase the perception of ocular symptoms in dry-eye patients, such as with neuropathic pain or other chronic pain conditions. They also mention that although the OSDI subscale and ocular symptoms displayed weak association with corneal staining and Schirmer’s test scores, these correlations didn’t differ with sex or depression status, although were stronger in patients with Sjögren’s syndrome.
Similarly, despite low correlations among the four signs of dry eye, the highest correlation was seen with corneal and conjunctival staining and was higher in the population of patients with Sjögren’s.
The authors discuss how mental health disorders can also contribute to the symptom level experienced with DED, which aren’t consistent with the severity of DED signs. One previous study outlined that DREAM participants with depression experienced more severe dry-eye symptoms than those without. Another observed depression to be more prevalent in DED patients and was associated with symptoms of dry eye but not signs. The current study found that the correlation was weaker between dry-eye signs and symptoms for those with depression than those without. As such, this may play a part in some of the discordance seen between signs and symptoms, but offers no complete explanation, and is likely not the majority of causation of these findings.
These observations prompt the authors to convey that “better objective minimally invasive metrics that capture biologic changes in the eye might lead to a better assessment of the severity of ocular surface changes in DED and perhaps a better correlation with symptoms.”
1. Tawfik A, Pistilli M, Maguire MG, et al. Association of dry eye symptoms and signs in patients with
dry eye disease. Ophthalmic Epidemiol. August 17, 2023. [Epub ahead of print].
Cataract Surgery a Boon in Acute Angle Closure Glaucoma
Sudden pressure increases that accompany acute angle closure can have devastating visual consequences. Prompt treatment is required to re-open the angle, often consisting of laser peripheral iridotomy to improve pupillary block. This approach doesn’t always open up narrow angles, however. Removing the lens via phacoemulsification is an alternative approach for deepening the anterior chamber, and in fact, a recent article published in the Journal of Cataract and Refractive Surgery reported that phaco was both safe and effective for this purpose.1
The study included 50 eyes of patients who underwent phaco within a week of presenting with acute angle-closure glaucoma and receiving IOP lowering treatment. All eyes were imaged and measured using anterior segment OCT and Pentacam.
The mean preoperative IOP was 40.3 mm Hg, which decreased to 14.9 mm Hg within one week of operation. Further pressure lowering was observed at postop weeks four and 12, to 12.4 and 11.44 mmHg, respectively.
The mean preoperative temporal angle width was 18.13˚, which widened respectively to 32.6˚, 34.6˚ and 36.2˚ at one, four and 12 weeks postop. The mean preoperative nasal angle width also increased from 17.8˚ to 32.7˚, 34.5˚ and 36.2˚ at postop weeks one, four and 12, respectively.
The researchers conclude in their paper that “early phacoemulsification is very effective in treating acute angle-closure glaucoma cases immediately after medical control of high intraocular pressure and resolution of corneal edema.”
1. Anbar MA, Mahmoud HA, Abdellah MM. Angle, anterior chamber parameters and intraocular pressure changes after early phacoemulsification in acute angle-closure glaucoma. J Cataract Refract Surg 2023. [Epub ahead of print].
Industry news
Regeneron Pharmaceuticals announced the FDA approved Eylea HD (aflibercept) Injection 8 mg for the treatment of patients with wet age-related macular degeneration, diabetic macular edema and diabetic retinopathy. The recommended dose for Eylea HD is 8 mg (0.07 mL of 114.3 mg/mL solution) every four weeks (monthly) for the first three months across all indications, followed by 8 mg every eight to 16 weeks in wAMD and DME, and every eight to 12 weeks for DR. Iveric Bio/Astellas Receives FDA Nod for Izervay Treatment for GA Last month, Astellas Pharma announced that the FDA approved Izervay (avacincaptad pegol) for the treatment of geographic atrophy secondary to AMD. The company says Izervay, a new complement C5 inhibitor, is the only approved GA treatment with a statistically significant reduction (p<0.01) in the rate of geographic atrophy progression at the 12-month primary endpoint across two Phase III trials. Oculis Announces Findings for OCS-01 in Phase III OPTIMIZE Oculis announced topline results from its Phase III OPTIMIZE clinical trial with OCS-01 eye drops, which the company describes as a novel, once-daily, high-concentration, preservative-free, topical Optireach formulation of dexamethasone for the treatment of inflammation and pain following ocular surgery. Harrow To Sell Vigamox in the United States Harrow received the rights to the New Drug Application for the antibiotic Vigamox (first approved in 2003). Harrow purchased the U.S. commercial rights to Vigamox in January 2023. |



