Traditionally, glaucoma treatment has consisted of medication, then laser if needed, and then, if it were necessary, surgery. However, laser proponents say that, due to medication’s drawbacks—such as non-compliance—and the safety and efficacy of selective laser trabeculoplasty being demonstrated in recent studies, SLT should be considered the first-line treatment. Of course, this is an opinion not shared by all. Here, glaucoma specialists review the pros and cons of laser as a first-line option.
The Medical Route
One of the disadvantages of glaucoma medication is patient non-compliance. “Like any other medication, it doesn’t work unless you take it. There are very few ocular medications that are used less than once a day. We know that our patients aren’t compliant in some cases. In other cases, they are extremely compliant because they’re very worried about losing their vision, if they’ve had good information as far as the necessity for treatment,” says Richard Lehrer, MD, who’s in practice in Canton, Ohio.
Overland Park, Kansas, physician Michael Stiles says one of the benefits of going the medication route is the fact that the effects are reversible. “If patients don’t like the medication, they can just simply stop taking it, go on to something else, or then consider laser,” he says. “In the real-world, we’re not bound to randomized trials. After hearing the pros and cons of both, some patients will just feel more comfortable trying medication. The reversibility of it, as compared to a one-time procedure, gives patients some comfort. Additionally, most medications don’t lose their efficacy over time, so it is something that can be used for a long period of time.”
Dr. Stiles adds, however, that one of the downsides to medications is the potential for side effects. “We’re finding more and more evidence that preservatives, like benzalkonium chloride, have an effect on the ocular surface, both short- and long-term, as far as quality of life is concerned,” he says. “For example, contrast sensitivity is less in patients who are on eye drops, and there can be long-term cosmetic side effects with the prostaglandins. Laser treatment has none of these issues. This is a concern because, if you need subsequent incisional filtration surgery, medication use can set you up for failure because of the beating the ocular surface has taken over the years with medications.”
 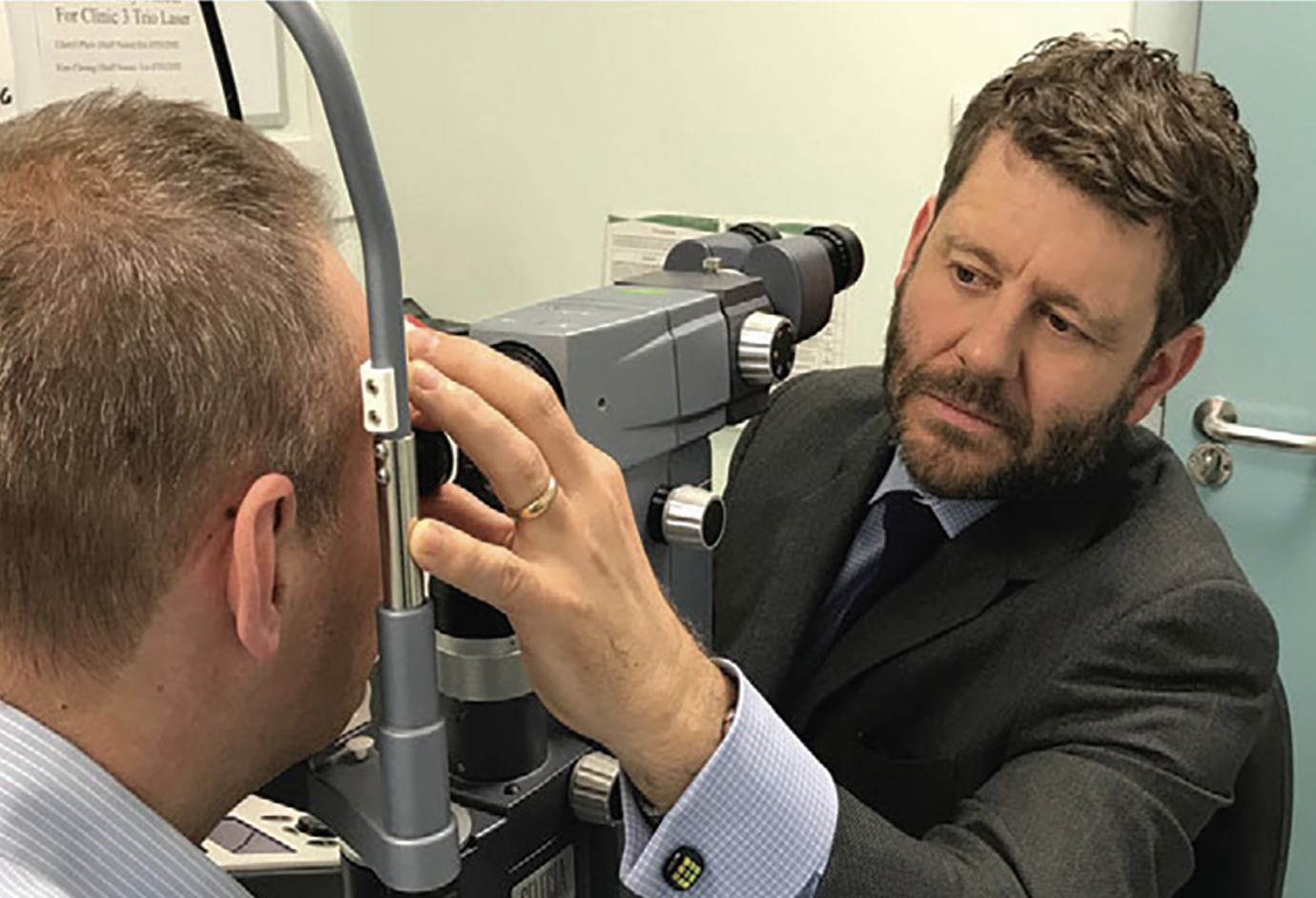 |
|
For patients with mild glaucoma, SLT may be all they need for years, proponents say. (Prof. Gus Gazzard) |
SLT
For proponents, SLT has several benefits over medication. According to Dr. Lehrer, “one pro of SLT is that it’s effective for a decent period of time, meaning at least one year. I’ve seen it last up to 20 years. In patients who have mild glaucoma and don’t require further therapy, that may be the only thing they need, and, therefore, they aren’t required to take daily eye drops or do other further treatment,” he says. “A con is that it sometimes doesn’t work. In my hands, the success rate is about 85 percent. Fifteen percent of the time, it won’t do anything, and very rarely, it may cause some inflammation or a transient rise in intraocular pressure.”
Dr. Stiles adds that SLT has been found in clinical trials to be as safe as medications, and has a good success rate. “Initial treatment is equal to at least one medication and, long-term, the visual field stability has been found to be superior to medications,” he says. “The downside is that it doesn’t work in all patients, and it doesn’t last forever. Additionally, it’s a ‘procedure,’ which gives some patients pause, but, to counteract that, we can safely say that it’s no more dangerous than starting medications.”
In an extension of the Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial,1 SLT was found to be safe for the treatment of open-angle glaucoma and ocular hypertension, providing better long-term disease control than initial drop therapy, with reduced need for incisional glaucoma and cataract surgery over six years of follow-up.
The LiGHT Trial showed that SLT is clinically effective and cost-effective as a primary treatment of both open-angle glaucoma and ocular hypertension at three years. A prospective, randomized, multicenter extension of the study examined health-related quality of life (HRQoL) and clinical effectiveness of initial treatment with SLT compared with IOP-lowering eye drops after six years of treatment. The study included treatment-naive eyes with open-angle glaucoma or ocular hypertension. Patients were randomly assigned to initial treatment with SLT or IOP-lowering drops. After the initial three years of the trial, patients in the SLT group were allowed a third SLT if needed, while patients in the drops group were allowed SLT as a treatment switch or escalation.
Of the 692 patients completing three years in the LiGHT Trial, 633 patients entered the extension, and 524 patients completed six years in the trial. At six years, no significant differences were found for the EuroQol EQ-5D 5 Levels, Glaucoma Utility Index, and Glaucoma Quality of Life-15. The SLT group had better Glaucoma Symptom Scale scores than the drops group (83.6 ± 18.1 vs. 81.3 ± 17.3, respectively). Of eyes that were initially treated with SLT, 69.8 percent remained at or less than the target IOP without the need for medical or surgical treatment. More eyes in the drops group experienced disease progression (26.8 percent vs. 19.6 percent, respectively). Trabeculectomy was required in 32 eyes in the drops group compared with 13 eyes in the SLT group, and more cataract surgeries occurred in the drops group (95 compared with 57 eyes). No serious laser-related adverse events occurred.
According to Paul Harasymowycz, MD, who’s in practice in Montreal, “the LiGHT Trial results have demonstrated that first-line SLT treatment may actually be beneficial for patients over a medical treatment, as well as being cost-effective. One should always remember, however, that SLT is not without potential complications itself,” he says. “Although very rare, someone did refer a case to me recently where a -9 myope who had bilateral SLT ended up with a hypermetropization, so the refraction changed to -4 in one eye and -5 in the other—a large shift. It seems to happen in patients who have pre-existing inflammatory conditions. If too much fluorescein is left in the eye, I’m concerned that the fluorescein on the surface of the eye may be up taken by the light, and that perhaps may be contributing to that process. When we’re checking the pressure before the SLT, we definitely make sure that there’s not too much fluorescein used, and we wash it out with artificial tears. You must weigh the pros and cons of both.”
Another study examining the results of eight trials found that SLT is safe and has a low incidence of ocular side effects.2 The researchers concluded that SLT can be the first-line choice of therapy for open-angle glaucoma.
This review article included randomized controlled trials conducted before August 2019 that compared the efficacy of SLT and medication only for open-angle glaucoma. Studies were selected using PubMed, Embase, Cochrane Library and Web of Science. Grading of Recommendations, Assessment, Development and Evaluations (GRADE) methodology was used to rate the quality of the body of evidence.
The eight trials comprised 1,229 total patients. Overall results revealed no significant differences between SLT and medication-only treatments regarding IOP reduction and the success rate of IOP control. The SLT group required significantly fewer medications compared with the medication-only group.
Which to Choose?
Both medication and SLT are great options for first-line therapy, so physicians say it can be difficult to choose between the two. Dr. Lehrer gives patients the option to choose. “If a patient has never been treated and has an IOP in the mid-20s, I think SLT is a very reasonable first-line option for them. Obviously, if they come into the office and their pressure is 45 or 50, they’re going to start on medication right away. But, for patients with mild to moderate glaucoma who have never been treated, I think SLT is a very good first-line option. I give patients all of the statistics. I tell them that the chance of the laser harming their eye is very low. I tell them that the chance of the laser working for at least a year is extremely good. Many of them do not want to take a medicine every day,” he says.
Dr. Stiles agrees and says he presents both medication and SLT to patients as options for first-line treatment. “I’m very honest with them about the LiGHT trial. With this evidence, I can safely say that I prefer laser first. But, they’re not bound to a trial. If they want to try the medications first, they can, but I do go over all of the pros and cons. I think the pros heavily favor laser first as opposed to medications first. That’s the way I lay it out, and the majority will pick laser first,” Dr. Stiles says.
Dr. Harasymowycz considers target pressure when recommending a treatment. “I would love for patients’ pressures to be 12 or lower with no side effects. Studies have suggested that the longer we follow our glaucoma patients, the more often we see some degree of progression, depending on the intraocular pressure,” he says.
For example, the Canadian Glaucoma Study identified four independent predictive factors for glaucomatous field progression in addition to intraocular pressure.3 This multicenter prospective longitudinal study included 258 patients (131 men and 127 women), with a median age of 65 years. Baseline systemic measures included assessment of peripheral vasospasm and markers for hematopathology, coagulopathy and immunopathology. Patients were followed up at four-month intervals with perimetry, optic disc imaging and a standardized interventional protocol for IOP control.
Patients were followed for a median of 5.3 years, with 167 patients (64.7 percent) being followed for five or more years and 67 patients (26 percent) being followed for seven years or more. Four factors were associated with progression: abnormal baseline anticardiolipin antibody levels; older age at baseline; female sex; and higher mean follow-up IOP before progression.
“If I have a newly diagnosed glaucoma patient, we really want to reach more aggressive IOP targets. It would be rare for SLT or prostaglandins to lower the pressure more than 30 to 35 percent. So, if someone comes in with a pressure of 30, he or she may not necessarily reach the target pressure that we want with only one treatment,” Dr. Harasymowycz explains.
He often prefers to start patients on a prostaglandin analog and reserve laser therapy for later. “After two months, we know the efficacy of that drop, and if we still haven’t achieved our target pressure, then we might add SLT as a second-line. However, if someone comes in with very little damage and doesn’t have a very high starting IOP, then SLT is definitely something worth trying first-line. The Canadian Glaucoma Study backs that,” Dr. Harasymowycz says.
He also considers SLT first if patients cannot afford medication or if they have been non-compliant in the past. “I think it’s important with both treatment options for patients to understand that this isn’t a curative treatment, and that they will have to be followed up. As long as they know the pros and cons of each, I think we can help guide them to choose the treatment that’s best for them,” he concludes.
Drs. Harasymowycz, Lehrer and Stiles have no financial interests to disclose.
1. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al; LiGHT Trial Study Group. Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial: Six-year results of primary selective laser trabeculoplasty versus eye drops for the treatment of glaucoma and ocular hypertension. Ophthalmology 2023;130:2:139-151.
2. Chi SC, Kang Y-N, Hwang D-K, Liu C J-L. Selective laser trabeculoplasty versus medication for open-angle glaucoma: Systematic review and meta-analysis of randomized clinical trials. Br J Ophthalmol 2020;104:11:1500-1507.
3. Chauhan BC, Mikelberg FS, Balaszi AG, et al; Canadian Glaucoma Study Group. Arch Ophthalmol 2008;126:8:1030-1036.