Assessment of the patient’s anisocoria both in light and dark conditions revealed a worsening anisocoria in the dark (See Figure 1A & B). Instillation of one drop of 0.5% apraclonidine into both eyes resulted in reversal of the anisocoria (See Figure 1C), consistent with a left Horner syndrome. Urgent MRI/MRA of the head and neck revealed a left internal carotid artery dissection at the skull base (See Figure 1D). Dilated funduscopic examination of both eyes was unremarkable.
The patient was admitted to the Neurology service for inpatient anticoagulation. He was continued on aspirin and ramipril on discharge, with close follow-up for long-term monitoring.
Discussion
Acute Horner syndrome, which results from disruption of sympathetic innervation, can be recognized by the triad of ptosis, miosis and anhydrosis, but all three features are rarely present together.1 Of note, ptosis can be extremely subtle, and it is reportedly absent in 12 percent of HS cases. Because sympathetically innervated muscle is also found in the lower lid (the inferior tarsal muscle), the lower lid may be elevated in HS, producing a so-called “reverse ptosis.”2 Anisocoria due to sympathetic paresis is more pronounced in the dark because the affected pupil exhibits a dilation lag; in physiologic anisocoria, the difference in pupillary sizes would remain constant in ambient light and in the dark.
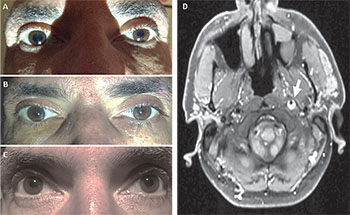 |
| Figure 1. View of the patient’s eyes (A) immediately after ambient light was decreased and (B) after ambient light was increased once again. (C) Is post apraclonidine testing OU. An axial T1 MR image (D) revealed a hyperintense, crescent-shaped thrombus (arrow) in the distal cervical segment of the left internal carotid artery (ICA) consistent with an ICA dissection. |
The causative pathology of the HS is generally apparent in more than 80 percent of patients at the time of the first neuro-ophthalmologic consultation based on history or clinical localization of the lesion.3 A “painful HS” is the most common sign of internal carotid artery (ICA) dissection, with an estimated sensitivity of 58 percent.4,5 Any patient presenting with ptosis and ipsilateral miosis associated with acute ipsilateral eye, face or neck pain should be considered to harbor an ICA dissection until proven otherwise; of note, the pain can be subtle, often described as a dull ache, and is often revealed only after specific questioning by the clinician.6 In the case presented, the patient had a history of sinus disease with a constellation of incidental symptoms and findings that led to delayed recognition of his underlying condition until his presentation to the emergency room.
The differential diagnosis of acute HS is broad and traditionally divided anatomically into first-order causes (central; which can include pituitary tumor, stroke, demyelination, neck trauma, etc.), second-order causes (intermediate; which can include brachial plexus injury, Pancoast tumor, mesothelioma, aortic aneurysm or dissection, etc.), and third-order causes (post ganglionic; which can include ICA dissection or aneurysm, skull base tumors, herpes zoster, etc.).1
When HS is suspected, one of several confirmatory pharmacologic tests may be employed. Generally these tests cannot reliably localize the lesion to a particular site and thus cannot guide imaging choice. Traditionally, cocaine has been highly effective at separating HS patients from controls, with an average post-cocaine anisocoria of reportedly greater than 0.8 mm.7 Cocaine’s biggest advantage over other agents is its ability to pharmacologically diagnose HS immediately after onset. Therefore, a negative cocaine test effectively rules out HS at any stage, including the acute phase. Unfortunately, cocaine drops have a short shelf life and are not readily available in clinical practice. Similarly, apraclonidine can confirm the diagnosis of HS within approximately 36 to 72 hours of symptom onset; however, a negative test prior to this time frame does not rule out HS.8 With an overall sensitivity of approximately 87 percent,9 the apraclonidine test remains a viable alternative to the cocaine test. Apraclonidine testing in HS has not yet been validated in a large sample, and several reports of false negative tests have been published.10,11 Diluted phenylephrine and hydroxyamphetamine are cumbersome tests that have no practical use in the diagnosis and management of HS.12
In one large series of 146 consecutive patients with extracranial carotid artery dissection, a nonreversible ocular or hemispheric stroke occurred in 27 patients, within a mean of 6.2 days among the 76 (52 percent) patients that had ophthalmologic symptoms or signs as the presenting findings of dissection. About 67 percent of these occurred within the first week of symptom onset, 89 percent occurred within the first two weeks, and none occurred after 31 days.6 This reinforces the importance of early diagnosis and initiation of treatment before a devastating stroke ever occurs.
Imaging can be targeted or non-targeted, based on the clinical presentation. One retrospective cohort study of 52 patients with HS who were being examined for the first time by a neuro-ophthalmologist revealed that the etiology was already known in most patients (62 percent) and that the most common etiology was surgical trauma to the head, neck or chest.3 Targeted imaging revealed the cause in 21 percent of patients (most commonly carotid dissection or cavernous sinus mass), and non-targeted imagining was required in the remaining 17 percent of cases. This has led Jonathan Trobe, MD, and colleagues to propose a relatively straightforward algorithm for evaluation of HS: (1) confirm that there is indeed HS using either topical cocaine or aproclonidine; (2) determine whether there has been previous accidental or surgical trauma that would explain the HS; (3) perform urgent targeted imaging guided by the presenting complaints (CT/CTA or MRI/MRA of the head and neck), especially if the HS has been present for less than than two weeks; (4) imaging of the lung apex, while important in uncovering rarer causes of HS such as lung tumors, can be performed as an outpatient.13
In conclusion, early recognition of acute HS is extremely important. Ipsilateral pain in HS represents ICA dissection until proven otherwise and calls for urgent soft tissue and vascular imaging of the appropriate anatomy (neck and skull base) if identified within the first two weeks from symptom onset, when risk for stroke is greatest. Pharmacologic tests (cocaine or apraclonidine) should be employed to confirm HS, but do not aid in localizing the underlying pathology along the sympathetic chain. Acute ICA dissection requires urgent neurosurgical or vascular evaluation and treatment. REVIEW
1. Davagnanam I, Fraser CL, Miszkiel K, Daniel CS, Plant GT. Adult Horner’s syndrome: A combined clinical, pharmacological, and imaging algorithm. Eye (Lond) 27, 291-298, doi:10.1038/eye.2012.281 (2013).
2. Maloney WF, Younge BR, Moyer NJ. Evaluation of the causes and accuracy of pharmacologic localization in Horner’s syndrome. Am J Ophthalmol 1980;90:394-402.
3. Almog Y, Gepstein R, Kesler A. Diagnostic value of imaging in horner syndrome in adults. J Neuroophthalmol 2010;30:7-11. doi:10.1097/WNO.0b013e3181ce1a12.
4. Mokri B. Traumatic and spontaneous extracranial internal carotid artery dissections. J Neuroophthalmol 1990;237:356-361.
5. Guillon B, Levy C, Bousser MG. Internal carotid artery dissection: An update. J Neurol Sci 153;1998;146-158.
6. Biousse V, Touboul P, D’Anglejan-Chatillon J, Lévy C. Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol 1998;126:565-577.
7. Kardon RH, Denison CE, Brown CK, Thompson HS. Critical evaluation of the cocaine test in the diagnosis of Horner’s syndrome. Arch Ophthalmol 1998;108:384-387.
8. Lebas M, Seror J, Debroucker T. Positive apraclonidine test 36 hours after acute onset of horner syndrome in dorsolateral pontomedullary stroke. J Neuroophthalmol 2010;30:12-17, doi:10.1097/WNO.0b013e3181b1b41f.
9. Koc F, Kavuncu S, Kansu T, Acaroglu G, Firat E. The sensitivity and specificity of 0.5% apraclonidine in the diagnosis of oculosympathetic paresis. Br J Ophthalmol 2005;89:1442-1444, doi:10.1136/bjo.2005.074492.
10. Kawasaki A, Borruat FX. False negative apraclonidine test in two patients with Horner syndrome. Klin Monbl Augenheilkd 2008;225:520-522, doi:10.1055/s-2008-1027349.
11. Dewan MA, Harrison AR, Lee MS. False-negative apraclonidine testing in acute Horner syndrome. Can J Ophthalmol 2009;44:109-110, doi:10.3129/i08-162.
12. Moster ML, Galiani D, Garfinkle W. False negative hydroxyamphetamine test in horner syndrome caused by acute internal carotid artery dissection. J Neuroophthalmol 2003;23:22-23.
13. Trobe, J. D. The evaluation of horner syndrome. J Neuroophthalmol 2010;30:1-2.



