Once surgeons become skilled at a particular type of refractive surgery, they may think they can easily move to another form of refractive surgery without complications, according to Ashvin Agarwal, MD, who is a cataract and refractive surgeon and the chief clinical officer of Dr. Agarwal’s Eye Hospital in Chennai, India. “When starting out with small-incision lenticule extraction, it’s easy to be bullish,” he says. “It’s like having a new toy in your hands and you want to explore the boundaries of it. The manufacturer has recommended parameters, and surgeons start testing how much further they can push those limits.”
The SMILE Technique
SMILE is being embraced by more refractive surgeons year after year for a number of reasons, including its lack of flap creation which significantly lowers the risk of flap dislocation and reduces issues that could occur during the healing process. The procedure, approved by the FDA in 2016, requires a specific femtosecond laser (Zeiss VisuMax) to create a disc-shaped lenticule inside the cornea. The lenticule is then removed through a 2- to 3-mm corneal incision.
There’s a learning curve to SMILE, as with anything, so some initial bumps are to be expected as you get to know the procedure, explains Dr. Agarwal. “When I began my SMILE journey, I was faced with several issues. These are commonly experienced by those within their first six months of SMILE, but don’t fret: You’ll learn quickly and soon enough you won’t have these complications,” he says.
“The key words to remember are: Abort mission. If something goes wrong and you can’t recover, just stop,” asserts Dr. Agarwal.
We spoke with him about some of the most common SMILE complications and what not to do if they happen to you.
 |
|
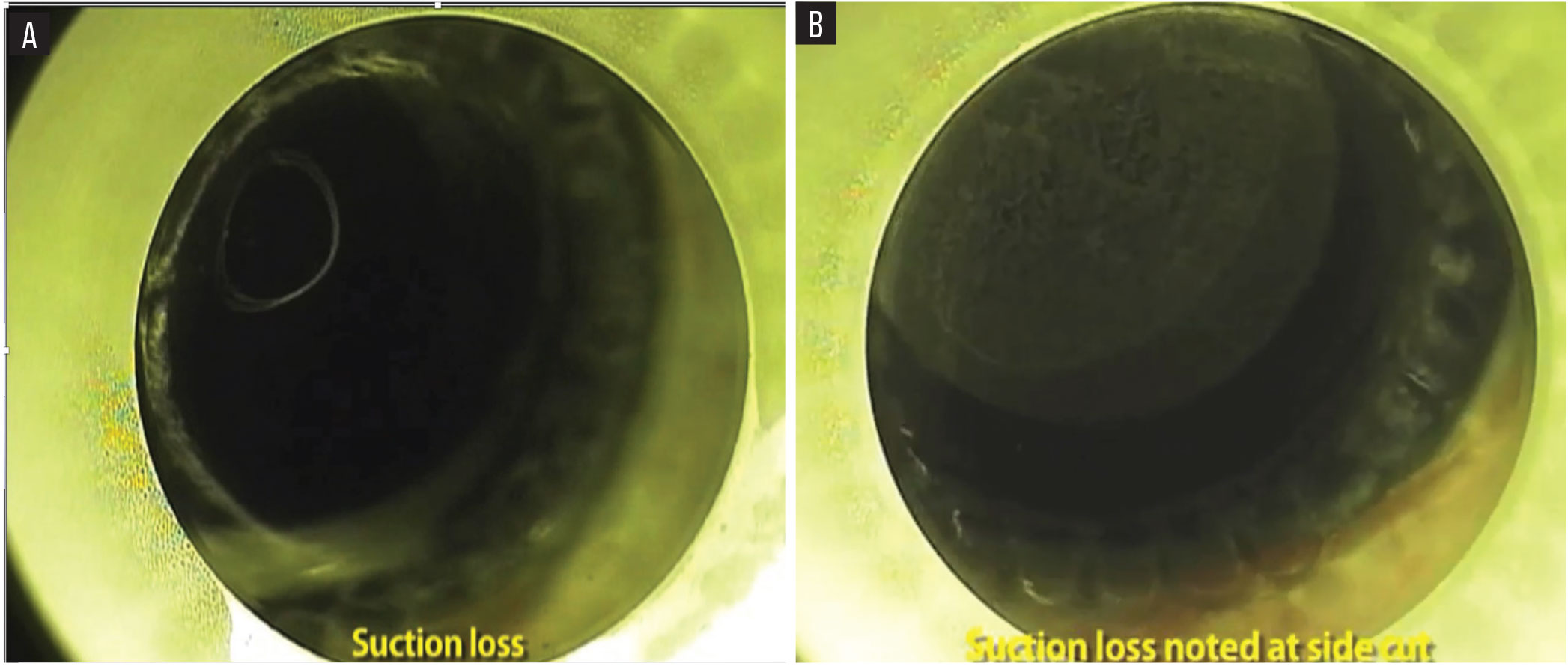
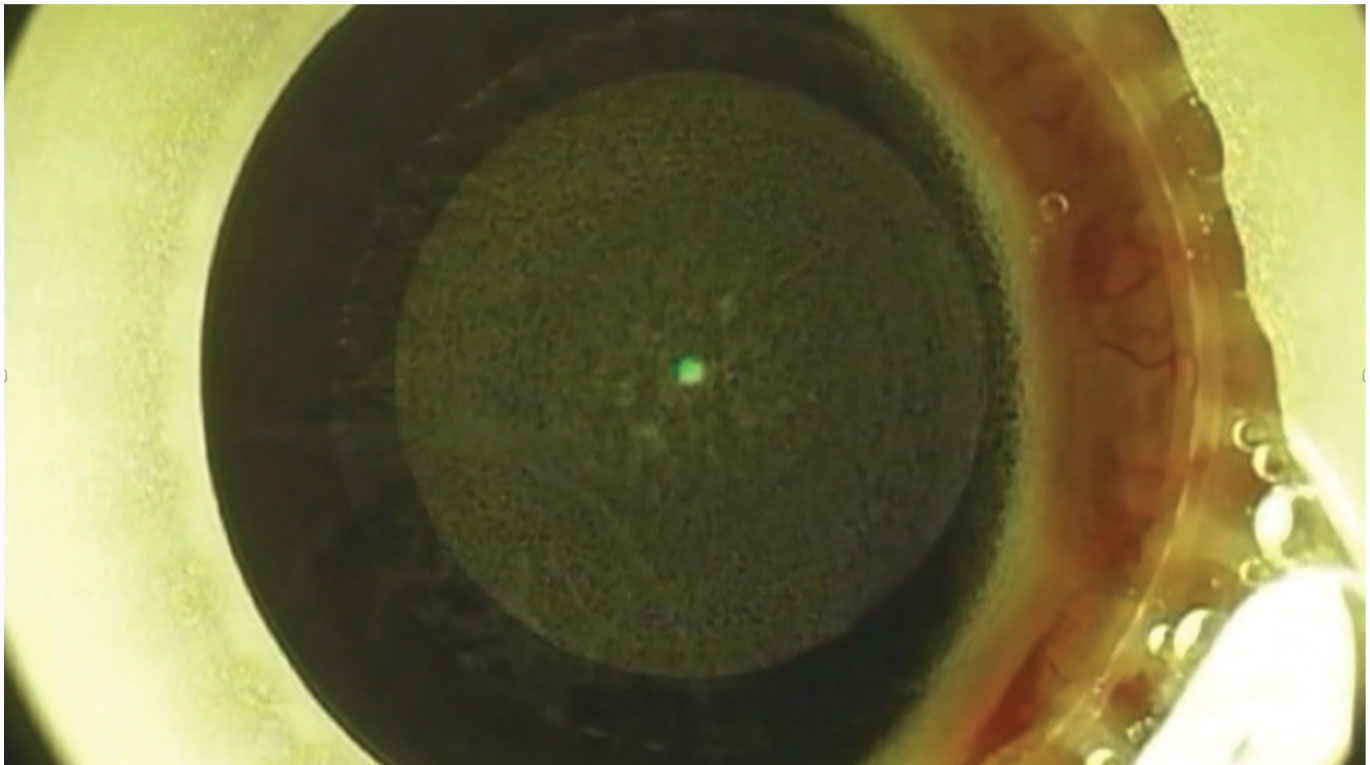
If suction loss occurs during the posterior lenticule cut after 30 percent (Figure A) or at the side cut (Figure B), it’s best to stop the SMILE procedure and wait a few months before performing LASIK or PRK, suggests Ashvin Agarwal, MD. |
 |
Problem: Suction Loss
Suction loss can happen at different stages, Dr. Agarwal says. “I personally wouldn’t recommend continuing the procedure if it occurs. However, I was fortunate to continue these cases successfully with great results for the patients,” he says.
“Let’s say your suction loss happens when the posterior lenticule is being cut, you’re safe if it’s between 10 and 20 percent. Anything after 30 percent, if you have suction loss, just abort. Come back after two or three months,” says Dr. Agarwal. “I’d recommend doing a PRK or LASIK procedure in that scenario.
“Next, what if you have suction loss between the posterior lenticule and the side-cuts? Once the laser crosses the posterior lenticule side-cut, you’re fine, but until then, there’s about 23 seconds with the VisuMax 500 and six seconds with the VisuMax 800 SMILE Pro,” he continues. “If suction loss occurs anywhere in between, you should abort the mission.
“In my case, I went ahead and did a repeat docking and a repeat transfer of spots, which led to issues such as a small skirt of tissue, which you have to actually peel off and use for your ablation in case you’re doing a flap,” he says. “You could consider a CIRCLE enhancement, which converts the SMILE cap into a larger-diameter LASIK flap with the creation of lamellar rings and junction cuts to connect to the primary cap interface. If you were to lose suction between the 20 percent and the side-cuts, if you re-dock and make the side-cuts separately, they will be dislocated at some point. That can lead to issues of transitional zones so you have to be careful about that area.”
Another issue is suction loss during the anterior lenticule cut, meaning the side-cuts are complete and the laser is starting on the anterior lenticulae. “If you try to re-dock at this point, no matter how well you center and position it, it’ll be off,” says Dr. Agarwal. “You can manage, but it’s going to be in a piecemeal format and you’ll be peeling out tissue from the side. It’s just not worth it.”
He continues, “Now, on the other hand, if just the anterior lenticule crosses the side-cut, you’re still in the scope zone. The lenticule is fine and the vision will be perfectly fine, but the problem is you’ll only have access to the lenticule through the external cut, which you need to make in the 2 to 4 mm zone.”
 |
|
If the lenticule becomes stuck to the cap, it’s important to know the cap recovery technique popularized by Dan Reinstein, MD, and Glen Carp, MD, which involves using a modified Sinskey hook to catch the edge of the stuck lenticule. |
Problem: Lenticule Stuck to Cap
This is very common. “In this scenario it’s important to know the rescue mechanism,” Dr. Agarwal says. “The cap recovery technique, popularized by Glen Carp, MD, and Dan Reinstein, MD,1 is an alternative to the traditional technique of dissecting in the plane. It describes dissecting the lenticule first with a modified Sinskey tip inserted through the superior end of the incision and rotated anteriorly to catch the edge of the stuck lenticule. Once you take a Sinskey tip and go into the cap to split the lenticule from it, then you hold and can dissect from there as you normally would. It’s a small technique but very important to understand in order to rescue yourself.”
In their study, Dr. Carp and Dr. Reinstein were able to show equivalent visual results of their technique compared to the traditional SMILE dissection, which first opens the primary small incision to separate the cap interface, followed by the lenticule interface.1
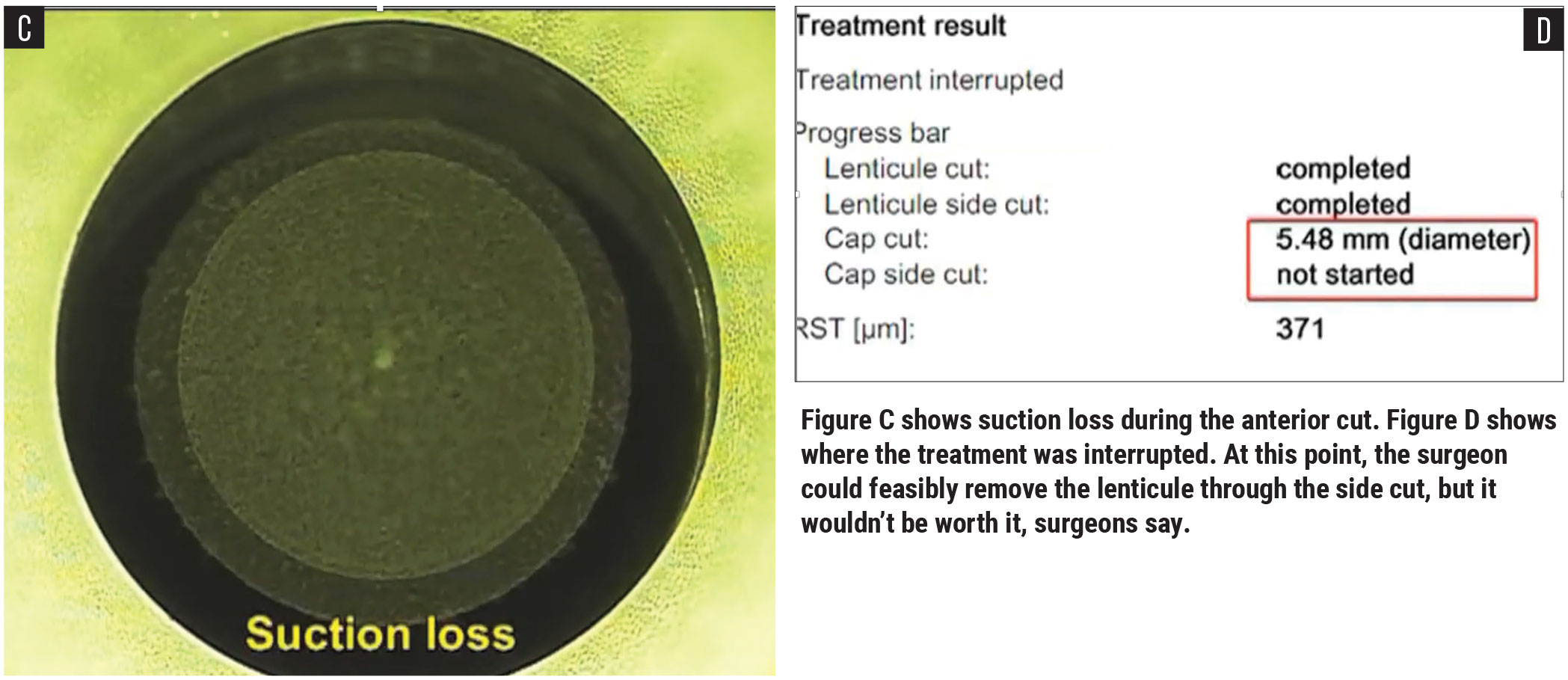
Problem: White Ring Sign
“This isn’t so much a problem in particular, but it can help prevent problems,” Dr. Agarwal says. “This was first described by Soosan Jacob, MD, and denotes the plane of dissection after the laser. An error in the plane can cause disaster. When dissecting in the posterior lenticule, the white ring sign is caused by the reflection of the microscope lights off of the dissection rod, making the edge of the lenticule clearly visible. When you’re doing an anterior dissection, you shouldn’t see a white ring sign. It’s a very interesting way to know that you’re in the correct plane.”
 |
|
|
The white ring sign is a way to confirm that the surgeon is in the correct plane of dissection. |
Once the lenticule is removed, the surgeon must piece it together on top of the eye to ensure all pieces were retrieved. |
 |
|
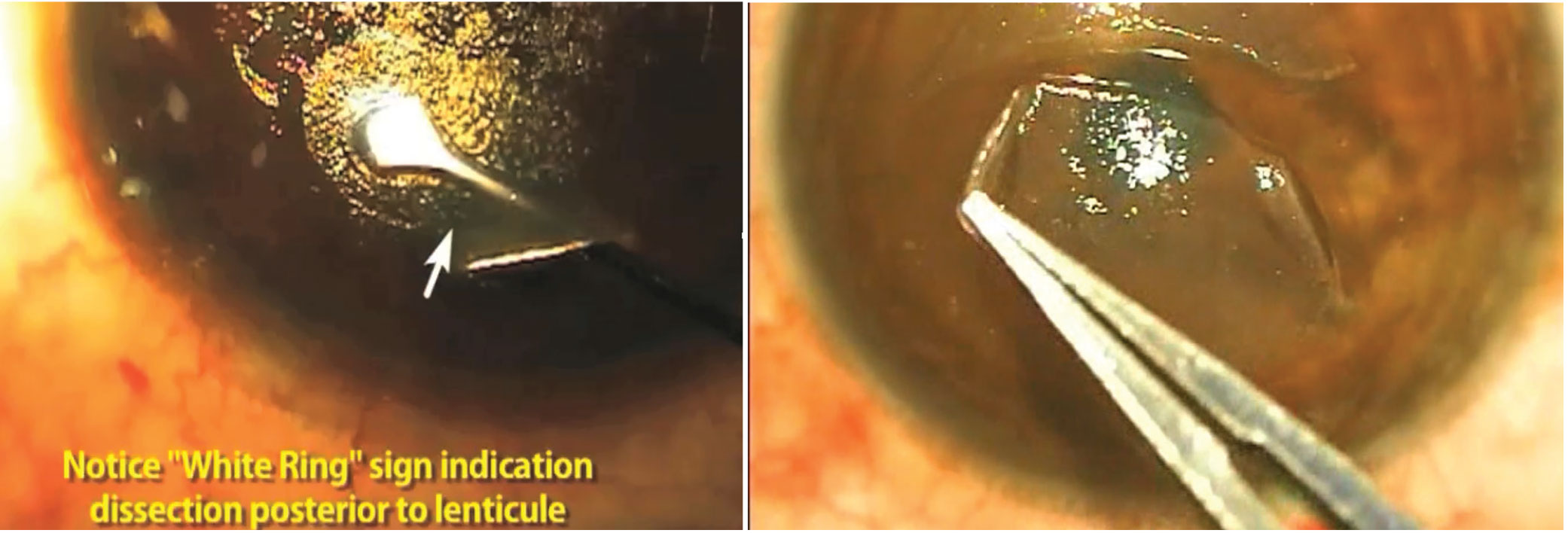
Although rare, if you notice conjunctiva bunching while the cut is being made, it’s best to abort and do a PRK three months later, recommend surgeons. |
Problem: Torn Lenticule
After retrieving the lenticule, you must ensure that you’ve removed it completely all the way around. “Don’t remove the lenticule and throw it aside because the minute you do that, there’s no way to know if something was left behind,” says Dr. Agarwal. “Always lay the lenticule on top of the eye and make sure it’s complete before discarding.”
Problem: Bunching of Conjunctiva
This is rare, says Dr. Agarwal. “If it doesn’t cross any part of the laser you were lucky and you can proceed,” he says. “But if it does cross the laser, just stop and don’t worry about it. Let it go and three months later do a PRK and you’ll be fine."
1. Carp GI, Reinstein DZ, Stuart A, Vida RS, Archer TJ, Finkel JN. Cap recovery technique and double-edge sign during small-incision lenticule extraction. J Cataract Refract Surg 2021;1:7:9:1191-1195.