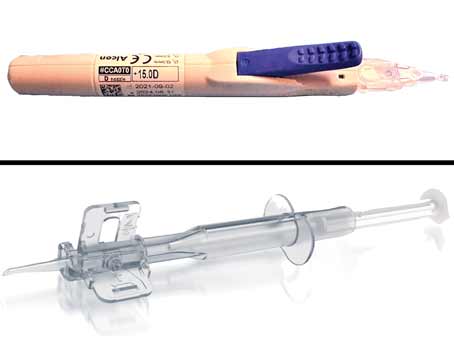
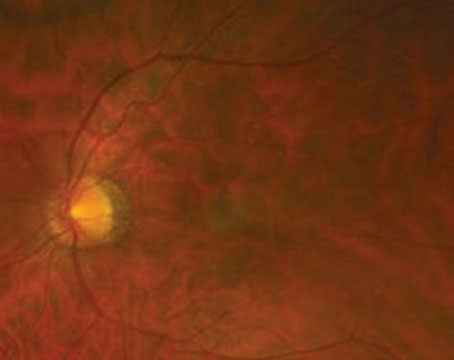
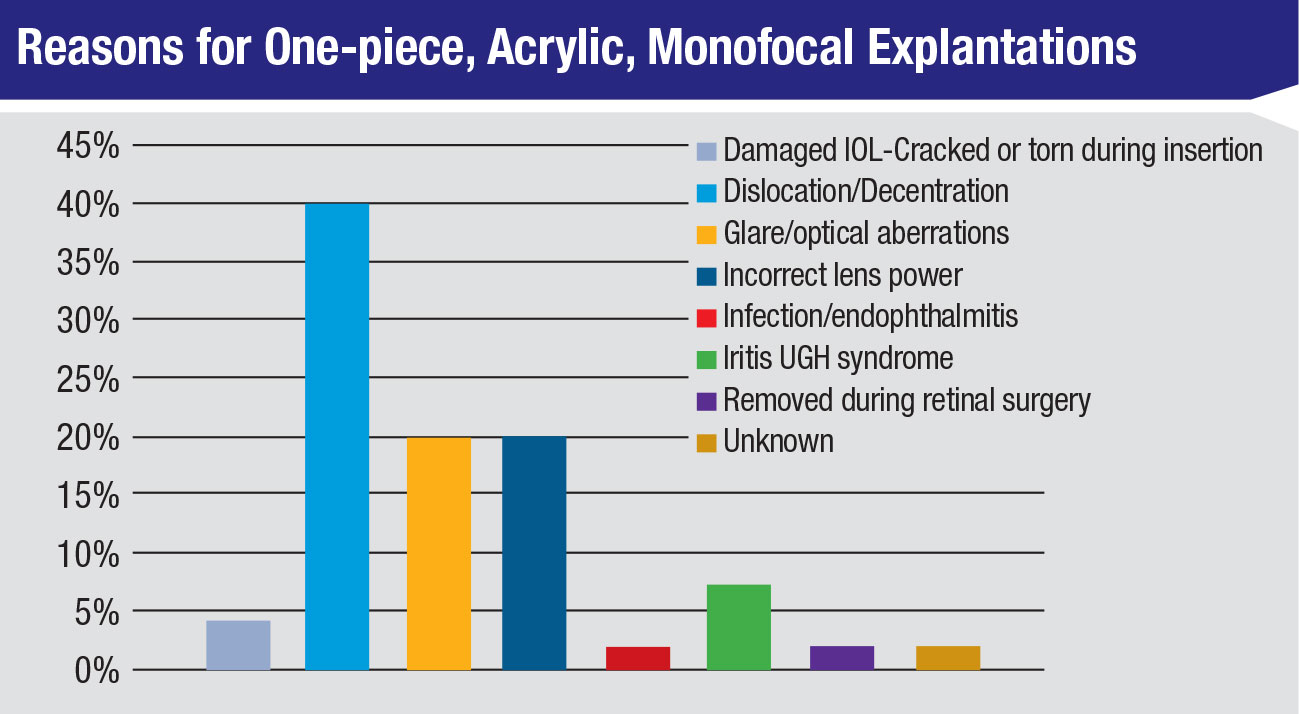
At the recent ASCRS meeting, Nick Mamalis, MD, professor of ophthalmology, co-director of the Intermountain Ocular Research Center and director of ocular pathology at the Moran Eye Center at the University of Utah, presented findings from his annual survey on foldable IOLs requiring explantation or secondary intervention. He began by noting that the type of lens with the highest rate of explantation is also the one implanted most frequently in the United States. “By far the most commonly explanted lens was a one-piece, hydrophobic acrylic,” says Dr. Mamalis. “But that really reflects the most commonly used lenses. Other materials are less frequently explantated because they’re just not used as much.”
Discussing the reasons for explantation, he says dislocation/decentration ranks as number one. However, he acknowledges that this complication doesn’t mean there’s an inherent problem with the design of the implant. “This implies either a complication during surgery, or some weakness of the zonules or the capsular bag that led to this complication,” he notes.
The second-highest reason for IOL explantation overall was glare/optical aberrations, though this was the most common reason for explantation of multifocals. “[Glare and/or optical aberrations] are usually the problems patients have with multifocals,” he says. “Since there may be difficulty tolerating these, people more commonly report these problems.”
 |
| Image courtesy of Dr. Nick Mamalis |
Dr. Mamalis discusses another noteworthy point in the data. “When looking at hydrophilic acrylic (hydrogel) lenses, we’re finding the most common reason for explanting is calcification,” he says. The incidence of explanting these intraocular lenses has gone down over the course of the survey, but Dr. Mamalis says this may be reflective of their less-frequent use in the United States.
Referring to previous surveys, Dr. Mamalis says it’s interesting that dislocation/decentration is still the number one reason for IOL explantations. “It’s always been [number one] and it stays that way,” he says. “Other complications sort of go up and down. Incorrect lens and power is still the third overall reason for IOL removal but it’s gone down over the course of the survey, which means we’re getting better at measuring IOLs and choosing the correct power.”
To avoid complications, Dr. Mamalis says good surgical technique is key. “An intact capsulorhexis with capsular bag fixation of the IOL will decrease dislocation and decentration markedly,” he says, adding that ensuring accurate IOL measurement is critical. He notes that this is becoming more difficult in patients who’ve previously had refractive surgery. Finally, Dr. Mamalis says that proper patient selection and preop counseling are necessary, especially to reduce complications with multifocal lenses.
Allergan Wins Small Victory vs. ImprimisRx
The drug-compounding company Imprimis-Rx was recently ordered to pay $48,500 to Allergan as a result of a false-advertising lawsuit Allergan brought against the company. How- ever, this was significantly less money than the millions Allergan had first sought.
Mark Baum, founder and board member of ImprimisRx, says the rul- ing was fair, stating that he doesn’t think Allergan was harmed. He says that ImprimisRx’s attorney made the case that the supposed false statements cited by Allergan didn’t seem to matter until Imprimis entered the glaucoma and dry-eye spaces. In regard to the alleged false statements, Mr. Baum notes that they weren’t made inten- tionally and were there for many years before Allergan sued.
Allergan declined to comment on the ruling, stating that the company doesn’t discuss litigation.
Tear Biomarkers and Systemic Disease
Screening for two debilitating diseases, Alzheimer’s and Parkinson’s, may become part of future eye exam protocols, according to two papers presented at the recent meeting of the Association for Research in Vision and Ophthalmology in Vancouver, Canada.
Researchers investigated the diagnostic potential of tears as a source of peripheral biomarkers for Alzheimer’s. They found that tear total-tau and amyloid-beta 42 (Aβ42) levels have reasonable discriminatory power for the AD state and could be diagnostic markers. They note, however, that studies with larger sample sizes are required to con- firm these results.1
The team investigated the tear biomarker level of total-tau and Aβ42 in a cohort of 25 patients with AD, mild cognitive impairment (MCI) or subjective cognitive impairment (SCI) and nine healthy controls.1 The results confirmed that the levels of tear total-tau and Aβ42 changed with increasing AD stage. They discovered a significant increase in total-tau in tears of AD patients compared with SCI patients and MCI patients.1
Future work on biomarkers must be able to characterize a patient’s underlying pathophysiology, the study authors argue. This requires an expansion of the current biomarker panel, a critical move to allow a broader characterization of pathology in patients with AD by identifying different subtypes.1
While the investigation into tear biomarkers for AD is in its early stages, biomarkers for Parkinson’s disease are already well-known. These patients often present with symptoms of cholinergic dysfunction years prior to showing motor symptoms. Tear secretion is greatly stimulated by cholinergic neurons; thus, specific proteins in tears may be altered by changes in the function of nerves regulating lacrimal secretion. Tear proteins are potential biomarkers for PD at different stages of the disease.2
Researchers from the University of Southern California found that tear levels of alpha-synuclein (α-Syn) may be able to discriminate between PD patients and healthy controls. They note that reflex tear α-Syn levels demonstrated a greater increase and sensitivity in distinguishing PD patients from healthy controls than basal tears and illuminated differences in lactoferrin that aren’t seen in basal tears, offering a more reliable and sensitive source of biomarkers for PD.2
The team collected basal tears from 93 PD patients of varying disease severities and 82 healthy controls with an anesthetized Schirmer’s test. Reflex tears were collected from 84 PD patients and 83 healthy controls with an un-anesthetized Schirmer’s test. They then pooled samples from both eyes to analyze their levels of total α-Syn, oligomeric α-Syn, LF and matrix metallopeptidase-9 (MMP-9).
They found total α-Syn was significantly decreased in basal tears in PD patients relative to healthy controls. On the other hand, oligomeric α-Syn was significantly increased in basal tears compared with healthy controls. The study findings indicated that there was no difference in LF or MMP-9 between PD patients and healthy controls in basal tears.2
In reflex tears, the researchers found oligomeric α-Syn was significantly increased in PD patients compared with healthy controls and that total α-Syn was unchanged. They note that a significant difference emerged in LF content in PD patients compared with healthy controls, but not in MMP-9.2
This work adds to the body of literature documenting the patterns and presentations of PD signals in human tear-film samples that may form the basis of future clinical testing protocols.
1. Gijs M, Nuijts RM, Ramakers I, et al. Differences in tear protein biomarkers between patients with Alzheimer’s disease and controls. ARVO 2019. Abstract 1744.
2. Edman MC, Janga SR, Freire D, et al. Tear biomarkers for Parkinson’s disease in basal versus reflex tears. ARVO 2019. Abstract 4196-B0554.
Novartis Nabs Xiidra
In early May, Novartis bought dry- eye drug Xiidra (lifitegrast ophthal- mic solution) 5% from pharmaceuti- cal company Takeda for $3.4 billion, with milestone payments of up to $1.9 billion.
For its part, Takeda says it made the sale in order to focus on other business areas, and to eliminate the debt it had amassed following its purchase of Xiidra’s original owner, Shire, which launched the drug in 2016. REVIEW