The movement to reduce the amount of ultrasound energy used to emulsify lens material during cataract surgery continues to produce new technology.
Technical advances in the control of fluidics are helping to reduce the amount of power used and to bring what is used under closer control of the surgeon. This article will discuss some of the ways surgeons are taking advantage of the ability to modify the machine parameters during phacoemulsification to improve their efficiency and surgical outcomes.
Refining Control
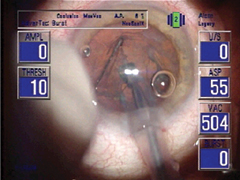
New York surgeon Robert Arleo, MD, has found several modifications to the Alcon Legacy system to be helpful.
Occlusion Power Management allows the surgeon to change the amount of power delivered postocclusion, so, for example, if you set the phaco power at 50 percent, you can program the machine to deliver only 25 percent once the tip has been occluded. "In the real world, most surgeons probably have the power set a little too high and this enables less power to be used," says Dr. Arleo, who is in private practice and is an assistant clinical professor of ophthalmology at SUNY Upstate Medical University.
 |
| New advances enable low, even no, ultrasound to remove some lenses. |
Burst mode phaco, previously available, has been improved, says Dr. Arleo. "Before you couldn't control the flow when you used burst mode phaco. You almost had a choice of having a slower aspiration rate than you would like in order to use burst mode, or you had no control over aspiration. Now you're able to do that plus you can add burst mode." This is a preset burst of phaco power, with the latent period between bursts controlled by how far you depress the foot pedal.
Dr. Arleo studied his own performance as he converted from the standard Legacy to the newer Advantec with the burst mode. "By the addition of burst mode, I went from 0.77 or 0.75 minutes average phaco time down to around 0.32 average phaco time," he says. "So it significantly reduced the amount of phaco time required."
Another benefit Dr. Arleo found with the burst mode was that, during that latent interval, the nuclear material can be repositioned on the phaco tip and led to better occlusion.
Finally, the addition of the NeoSonix handpiece offers the flexibility of a low-frequency, and, thus, low thermal energy phacoemulsification, with the standard ultrasonic modality. The subsonic oscillation on NeoSonix is slower than standard ultrasonic but can handle some denser lenses, says Dr. Arleo: "I've been able to do lenses up to a fairly dense 2+ lens with NeoSonix only, and no phaco power whatever. In the same study mentioned earlier, he found that the addition of NeoSonix cut his average phaco power from 16.6 percent with the Advantec down to 11.7 with the addition of Neosonix.
NeoSonix is adjustable in both amplitude and oscillation and threshold. The net result with Neosonix is that it improves phaco time both directly (the oscillations fracture the material instead of the ultrasound) and indirectly through improved surgical efficiency by repositioning a lens fragment as you're removing it.
| Maximizing Cavitation |
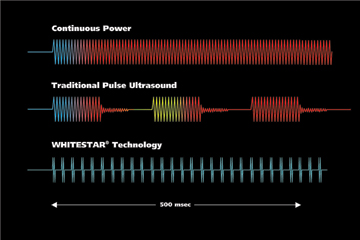 |
| Though there is a mechanical component, most of the cutting in phacoemulsification is done by acoustic cavitation. Mark E. Schafer, PhD, a physicist and expert in ultrasound, explained the process at last year's meeting of the American Academy of ophthalmology. Different phaco machines achieve cavitation at different power settings, depending on their stroke and tip size. Dr. Schafer described two types of cavitation. Transient cavitation leads to the violent collapse of microbubbles that exist in the fluid in which the cavitation is created. It's that explosive collapse of the bubble that disintegrates tissue, whether kidney stones or cataractous lenses. Transient cavitation quickly gives way to stable cavitation, in which there are fewer collapses and less energy released. Most standard phaco machines have pulse lengths of 50, 100 or 150 milliseconds. Transient cavitation lasts only few milliseconds of that time, and the remainder is the less efficient stable cavitation. The Whitestar technology of the AMO Sovereign energizes the tip for very small intervals, smaller than the pulse mode or burst mode on most machines, and then rests the tip, producing a "microburst" effect. These microbursts accentuate transient cavitation. There is no transition to stable cavitation, Dr. Shafer said. As a result the system retains the emulsification capability, while reducing phaco power and thermal energy. |
Though Dr. Arleo uses a quick chop technique, he adds that NeoSonix can benefit surgeons who still use divide-and-conquer. "In a procedure that depends on carving grooves into the lens with the ultrasound and manually cracking the lens into fragments, you need to use more phaco power, and very low vacuum and aspiration rates. "As you're making grooves deep enough to crack the lens, you can't have materials sucked into your needle, so you need very low flow settings. NeoSonix breaks up the material so you use less power, but it also disturbs the occlusion enough that you can use a bit more flow and vacuum. As a result, you reduce the amount of phaco power being used when you're making those grooves."
Cutting Power
Tucson, Ariz. surgeon William Fishkind points out that machine settings vary greatly from one machine maker to another, so direct comparisons are not practical. Given that, he starts with the manufacturer's recommendations and adjusts based on experience.
His surgical approach considers nuclear density and the various stages in the procedure.
"I use different settings for a hard, medium and soft nucleus," says Dr. Fishkind, a clinical professor of ophthalmology at the University of Utah. He generally uses a vertical chopping technique. "With a hard nucleus, I'm going to need to burrow into the nucleus with the phaco tip and hold it, so I can do vertical chopping. Generally speaking, I'm going to use high vacuums and usually a burst mode, which will allow me to use phaco energy to burst into the nucleus and then the vacuum to hold it onto the phaco tip," he says. He leaves flow at a moderate level. "I don't want to have extra cavitational energy (See sidebar), such as a long period of emulsification, because the energy will break the boundary between the nucleus and the phaco tip. This creates a space at the tip that allows fluid to flow in and won't allow a seal. So that's why I particularly like burst, high vacuum and moderate power. That gives me holding power."
Nuclear density is also a factor in intraoperative decisions about settings. "I may get into the center of a hard nucleus, and find that it keeps coming off the phaco tip," he says. "So I increase the vacuum for better holding power. With a hard nucleus you can do that; with a soft nucleus you can't because it will just suck everything in."
After completing 360 degrees of chopping, Dr. Fishkind brings the fragments to the iris plane for emulsification. "Now I will drop the vacuum but keep the flow moderate and move to pulse power, usually a slow pulse on a standard machine, and a Whitestar pulse on the Sovereign machine. This slow pulse allows material to come to the phaco tip. With standard phaco, you're going to let it occlude, hit a little burst of power, and bring a little piece in. The pulse will act like a ratchet wrench pulling pieces in and never letting go of them."
Other intraoperative developments may also impact settings. "As I remove fragments, I may get more surge than I want, whether from excess outflow from a wound that's not as tight as it ought to be, or an unstable chamber," says Dr. Fishkind. "Or a high myope with a thin sclera and less scleral rigidity may produce trampolining. I might either increase the bottle height or drop both the vacuum and flow parameters a little bit to stabilize the chamber."
After removal of the lens segments, Dr. Fishkind increases the flow slightly to deal with the epinuclear shell or the epinuclear cortical shell. This brings material to the phaco tip better, but holding is not as critical at this stage as during chopping, so a lower vacuum level can be used. "I will decrease vacuum a little more and, depending upon what's going on, I usually will leave the flow the same or drop it just a little bit, because at this point, the posterior capsule is exposed and I don't want trampolining," he says.
Surge Protection
Even with the ability to modify, surge can still present a surgical challenge. "The surgeon needs to be attuned to the fact that there is shallowing or instability of the anterior chamber," says Dr. Fishkind. "My first step is to lower the infusion bottle a bit. How much depends on so many factors, but just a few inches can make a big difference. Then, look at the vacuum and flow parameters and determine if they are excessive for the material being emulsified. I will tend to drop the flow first, in 2-cc steps. If I'm at 24 I'll go to 22; if I'm at 22, I'll go to 20, check the response, and see if the surge quiets down. I'll do that two times, or 4 cc's total. If that doesn't resolve it, I'll drop the vacuum by about 20 mmHg. Usually by just being aware and making some small adjustments, the improvement is amazing. All of a sudden thing stabilize and an unstable situation becomes a lot more comfortable."
As newer technologies continue to emerge, the ability to customize and modify phaco settings will continue to offer surgeons the possibility of improved outcomes and more efficient cataract surgery.



