Phacoemulsification has become the status quo for surgeons performing cataract removal in the United States. However, even this gold-standard technique has its drawbacks. Some patients cannot safely undergo a phaco procedure due to underlying endothelial issues or mature cataracts. Also, for many locations in the developing world, phaco is not an economical option. While phaco may be the current surgical approach of choice, techniques like sutureless manual small incision cataract surgery and devices like the miLoop can play a role in cataract removal for non-phaco candidates in the United States and in the developing world. Here, experts share their tips and techniques for cataract surgery in patients who can’t, or shouldn’t, undergo phaco.
The Non-phaco Candidate
Several factors can make a patient a better candidate for a procedure other than phaco. These include having a weak corneal endothelium or dense cataract, or living in the developing world with limited access to health-care resources.
Since phacoemulsification delivers ultrasonic energy as it breaks up the cataract, the procedure can cause stress to the endothelium. Nick Mamalis, MD, a professor of ophthalmology at John Moran Eye Center, University of Utah notes, “If you have someone with an endothelial dystrophy, you want to remove the lens nucleus with as little energy as possible.”
On a similar note, even if a patient has no existing corneal issues, if he has a very hard cataract, he’ll have to undergo extended phacoemulsification to break it up, which can still pose problems. Hunter T. Newsom, MD, medical director of Newsom Eye and lifetime visiting professor at the University of Iowa says, “When you have a cataract that’s extremely hard and dense, you have to use a large amount of phaco, and that’s going to cause a more significant amount of energy to be put inside the eye, which is going to damage the corneal endothelium.”
Patients in the developing world frequently present with advanced cataracts. “Oftentimes in the developing world you have patients with a relatively hard, dense, leathery nucleus, which requires a lot of ultrasound energy to remove,” says Dr. Mamalis. On a recent trip to South Sudan, Alan Crandall MD, the John A. Moran Presidential Professor, senior vice chair and director of glaucoma and cataract at the Moran Eye Center, says, “All we saw were dense, white, sometimes black cataracts.” Also, in some parts of the world, it’s not possible to set up a fully equipped phaco surgery suite, and other options need to be explored.
 |
| Figure 1. In the Dominican Republic, patients wait in long lines to be evaluated. Dr. Newsom says that doing surgery quickly and efficiently is important where there are a large number of cataract patients, and eliminating the need for sutures allows for rapid surgery. |
Manual Small Incision Cataract Surgery
As a viable alternative to phaco, MSICS uses little to no ultrasound energy and is very economical.
MSICS involves the use of a scleral tunnel incision. While the incision itself is only about 5 to 6 mm long, it’s created in such a way that it becomes larger as it nears the anterior chamber. This aids in the removal of the natural lens, which is accomplished using a syringe or a glide. The syringe creates suction, while the glide uses pressure to gently force the lens out. One of the other benefits, proponents say, is that sutures aren’t required with this technique, due to the small incision.
Here’s a closer look at MSICS’ advantages, disadvantages, potential pitfalls and results.
• MSICS’ advantages. While not as technologically advanced as modern cataract removal, some surgeons say that MSICS—sometimes called extracapsular cataract extraction—has several advantages.
-— MSICS can effectively remove cataracts without energy, therefore minimizing endothelial damage. “Extracap applies a lot less trauma to the corneal endothelial cells,” says Dr. Newsom.
— MSICS allows the cataract to be removed whole, which also helps protect the endothelium, since the surgeon doesn’t need to use energy to break it up. Dr. Mamalis says that the incision is actually wider as you’re coming out of the anterior chamber. “The advantage here is that you don’t have to disassemble a hard lens nucleus,” he says.
— MSICS can be economical. “The instrumentation for extracap includes things that can be used multiple times,” says Dr. Newsom. This reusability helps keep the technique inexpensive. This is one of the main reasons that MSICS is such a viable option for those in the developing world. Comparatively, Dr. Mamalis says there are challenges associated with using phaco in the developing world. “Since it’s relatively expensive, there are difficulties in just getting the phacoemulsification machine, he says. “There’s a significant expense involved with the necessary tubing, packs and tips.” Dr. Newsom expands on this idea, citing added costs associated with the disposable instruments and accessories. “Single-use is the way that all modern phaco machines are trending,” he says. “It’s very rare that you have things that are reusable, and this serves to drive costs up, not down.”
— MSICS allows you to use a sutureless incision, which Dr. Mamalis says adds to its feasibility in the developing world. “Sutures add an expense and take increased surgical time to place,” he says. “When you’re in a setting where there are a large number of cataract patients and you have to do surgery as quickly and efficiently as possible, eliminating the need for sutures allows for rapid surgery.”
Dr. Crandall emphasizes that MSICS still has a place in the United States. “In Utah, we treat refugees and people in the Navajo Nation, and at least once or twice we see a dense, white cataract or a morgagnian cataract. Those are unlikely to be phacoable, so we’ll go ahead and perform an extracap,” he says.
• MSICS disadvantages. While MSICS is inexpensive and effective, there are disadvantages to the technique. A cornerstone of MSICS is that the cataract can be removed whole. However, this can sometimes prove to be more complicated than it sounds. “Even though it’s called small-incision, you still make a fairly large incision through the sclera and the cornea,” Dr. Mamalis says.
Dr. Newsom notes other possible incision issues: “If you’re going into the sclera, you’re going to have to do a peritomy or go through the conjunctiva in some way,” he says. “You’re going to be cutting blood vessels at the limbus and pulling the conjunctiva, and that introduces blood and [the need for] cautery. The eye is going to look a lot redder and more injected.” For the entry wound, Dr. Mamalis prefers a scleral frown incision. “You want to make sure that, as you’re making the scleral incision, you’re at the correct depth and that the inside opening is large enough to allow you to remove the relatively large lens nucleus,” he says.
The capsulotomy size can also be a challenge. “Whether you’re doing a can-opener type opening or a continuous capsulorhexis, it can be difficult to get the large cataract out of the bag and into the anterior chamber,” says Dr. Newsom. As a result, Dr. Mamalis says, the surgeon needs to make a capsulorhexis that’s large enough to get the nucleus out of the bag whole. Dr. Newsom suggests using Trypan blue to help accurately perform the capsulorhexis.
Another consideration is that since extracapsular surgery preceded the advent of phacoemulsification, it’s not usually taught to surgeons anymore, especially in the United States. “Newer surgeons don’t do a lot of extracapsular surgeries,” says Dr. Mamalis. “To be honest, a lot of our residents aren’t trained on many extracapsular cases, so it’s unfamiliar territory to them.” Dr. Crandall adds, “It’s hard to teach people this technique. The problem is that the rate of seeing patients with non-phacoable cataracts in the U.S. is small.”
 |
| Figure 2. Minor surgery is conducted on a patient in the Dominican Republic by Hunter Newsom, MD, and his team. |
• Pitfalls. A few MSICS trouble spots to watch out for include complications with the procedure itself and the rate of postop astigmatism.
Dr. Newsom discusses some potential complications to be aware of. “You have all kinds of chamber-depth issues,” he says. “You’ve got everything coming up and it tends to bang on the cornea. With extracap, everything is shallower, and the iris can get damaged or try to come out of the wound, which can potentially create a hemorrhage.” He adds that there’s more corneal edema and inflammation, and that healing is slower for extracapsular surgery compared to phaco.
In terms of astigmatism, there’s only so much that can be done in certain countries. “In the developing world, you know there’s going to be a huge amount of astigmatism, but the cataract is gone and they can see again [which is the most important aspect of the surgery],” says Dr. Newsom. Dr. Crandall agrees, saying, “The priority is to restore vision. We’re talking about people who are seeing light perception; all they can see is light or dark. First and foremost, we’re interested in getting patients back on the chart and walking around. It’s not that we don’t care about astigmatism, but when you have 500 people who have light-perception cataracts, and you have five days to perform procedures, [you just can’t measure it].”
In reference to his past work in the Dominican Republic, Dr. Newsom says IOL selection was a challenge. “Determining what type of lens power to put in the eye and measureing astigmatism is difficult,” he says. “We didn’t have the precision of our usual keratometry measurements.” When comparing the developing world to the United States, he likens the IOL selection-process to getting a pair of shoes; he says that, in the United States you can choose from many different numbered sizes, but in the developing world, he says, you may only have sizes small, medium and large, “You have what you have, and there’s not a big selection to choose from,” he says.
• MSICS results. In a study that compared the efficacy and visual results of two different MSICS methods, called “modified Blumenthal and Ruit,” it was found that MSICS produces good visual outcomes and only minor complications.1 After three months, corrected visual acuity in the Blumenthal group was 0.73 (just under 20/25) and 0.69 (a little better than 20/32) in the Ruit group.1 The average postoperative astigmatism was 0.87 ±0.62 D and 0.86 ±0.62 D for the Blumenthal and Ruit groups, respectively, while mean surgically induced astigmatism was 0.55 ±0.45 D and 0.50 ±0.44 D, respectively.1 Otherwise, noted complications included minimal hyphemas and corneal edema.1
The miLoop
Surgeons say the miLoop device, from Zeiss, can help streamline some of the steps of MSICS.
The miLoop is a relatively inexpensive and disposable instrument made of nitinol, a strong material; it can be injected through a small, clear corneal incision. Once injected, the filament loop extends under the anterior capsule and goes around the nucleus to the equator and then the posterior surface. As the loop is withdrawn, it cuts through the nucleus, bisecting it. The device can then be used to rotate the nucleus and further break it into quarters or even smaller pieces. Doctors say no phaco is needed, just a manual irrigation/aspiration handpiece.
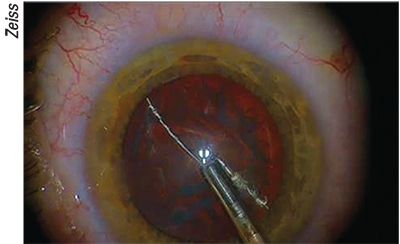 |
| Figure 3. miLoop ensnares the lens. |
• Advantages. As an alternative to phaco, some surgeons say miLoop is a viable tool for managing non-phaco candidates in the United States and for medical missions in the developing world.
In surgery, surgeons say certain patient presentations might benefit from the use of the miLoop. “MiLoop is useful for people who have a very dense, hard, leathery nucleus that’s difficult to disassemble and would require a lot of phaco energy,” Dr. Mamalis says.
Doctors agree that these patients could have issues associated with extended phaco time, so in an effort to see how gently the device could tackle the nucleus, Dr. Crandall aided in the creation of the Miyake/Apple technique. Using the technique, they confirmed that the device was very zonular- and capsular-bag friendly. “The beauty of the miLoop is that it can be used [to break up] really hard cataracts,” Dr. Crandall says, “since the energy is kept away from the bag and the zonules. It’s a great skill to know.”
Dr. Mamalis feels that an advantage of the miLoop is that the surgeon doesn’t have to make a scleral tunnel. “You can disassemble a hard nucleus into small pieces that you can remove through a clear corneal incision,” he says. When considering the usefulness of the device in the developing world, he adds that it’s helpful to be able to use a small, clear corneal incision. “Anything you can do to make the incision smaller, especially in a developing- world setting, is helpful,” he says.
Dr. Crandall adds that there are two advantages to using the miLoop in international settings. “One is that you have the ability to use a small incision, since you can break the nucleus in half, which can be critical,” he says. “Two, you can use foldable lenses.” He also states that since the miLoop incision is smaller than a conventional, 10-mm extracap incision, there may be less induced astigmatism to worry about postop, though the difference would be small.
When it comes to patients in the United States who may not be able to undergo phaco, Dr. Newsom says that the miLoop allows him to make on-the-spot decisions as to whether phaco will be too strenuous for a given eye, and therefore shouldn’t be used to perform cataract surgery. “MiLoop is a very interesting option that I think everyone should have access to in the operating room,” he says. “I want [miLoop] there, ready to be opened, so that as I’m doing my initial assessment I can determine whether I need it based on the case, intraoperatively. MiLoop has eliminated any reason for a potential extracap.”
Dr. Mamalis says that the miLoop can also be used as a training tool. “MiLoop could allow doctors who don’t have experience making a scleral-corneal incision to disassemble a nucleus into multiple, smaller pieces,” he says.
• Disadvantages. Since it’s the only device of its kind, Dr. Mamalis says there’s a learning curve. “The device works wonderfully but, like any other technology, it has to be used properly and it’s important that people are trained to use it,” he says.
Dr. Mamalis says visualization can be an issue, and there’s also a need to have an intact capsule. “Sometimes what’s difficult with the miLoop is that if you have a really dense nucleus, once the loop goes behind it, you sometimes can’t visualize it well,” he says. “Also, if you’ve got some tears in the anterior capsule or you’ve got an anterior capsular extension, you may want to reconsider the use of the miLoop.”
• Technique tips. To get a better handle on the miLoop, Dr. Mamalis suggests employing the Miyake/Apple technique to view it in action, using a cadaver eye. “You take a donated, human cadaver eye and section it coronally, at the equator, and glue the anterior segment of the eye to a glass slide,” he says. “That allows for simultaneous videoing both anteriorly and posteriorly, which is very helpful when you’re evaluating devices like the miLoop.” This has enabled Dr. Mamalis to video the device as it’s sectioning the nucleus, and see what’s happening to the capsular bag and the zonules. He notes that there are also many videos available online that can show you how to use the loop.
Using enough viscoelastic is also important. “Adequately use viscoelastic to ensure that the loop is going underneath the anterior capsule properly and then coming around the equator,” explains Dr. Mamalis. “Make sure that you’re going all the way around the nucleus without snagging or getting caught on anything in order to break the nucleus into multiple pieces and disassemble it.”
• miLoop results. In a randomized, controlled study, where several of the researchers were employees or consultants for the maker of miLoop, Iantech, the safety and efficacy of surgery with the miLoop was assessed in moderate to severe cataracts. The study found that miLoop fragmented every dense nucleus within the capsular bag.2 The miLoop filament completely transected the nucleus without any centrifugally directed instrument forces that would stress or stretch the capsular bag, the researchers said. In advanced cataracts and cases involving weak zonules, there were no instances of zonular dialysis or anterior/posterior capsule tears.2
Looking Ahead
Though cataract surgeons in the United States almost exclusively use phaco, Dr. Mamalis says reliable phaco is still difficult to access in the developing world, and alternatives will always be welcome. “[For phaco to be feasible] you need to be in a situation where maintenance can be performed on the machine so that it’s working consistently,” he says. Dr. Newsom adds that certain complications of phaco might be too much for surgeons in less-well-equipped countries, as well. “There are limited options readily available to fix a problem,” he says. “If you have healing issues in the cornea because of increased phaco energy, you probably don’t have access to corneal transplants. There’s also limited access to specialists who can potentially treat a patient that might have endothelial damage as a result of extended phaco time.”
Dr. Crandall expands on this idea, saying, “If you’re in a developing country and you have one of these big, expensive machines and a light bulb burns out, what are you going to do? They don’t have the back-ups that we do.” For this reason, doctors say that even donated phaco machines can be problematic.
That said, MSICS looks to continue as the main form of cataract removal in the developing world, with miLoop poised to find its niche. Dr. Mamalis says that patients with a relatively dense nucleus would benefit from both of these techniques, too. He adds that there’s a large overlap in MSICS candidates and miLoop candidates, and if properly done, you can get very good results using either. “[MSICS and miLoop are] very friendly to the cornea,” Dr. Mamalis says. “They will allow you to remove a relatively dense nucleus without requiring the high ultrasound energy that’s necessary when performing phaco.” REVIEW
Drs. Newsom, Mamalis and Crandall report no financial disclosures in the products discussed.
1. Kongsap P. Visual outcome of manual small-incision cataract surgery: Comparison of modified Blumenthal and Ruit techniques. International Journal of Ophthalmology 2011;4:1:62-5.
2. Ianchulev T, Chang DF, Koo E, et al Microinterventional endocapsular nucleus disassembly: Novel technique and results of first-in-human randomised controlled study. British Journal of Ophthalmology 2019;103:176-180.