Minimally-invasive glaucoma surgery is intended to lower intraocular pressure with less tissue disruption than traditional glaucoma surgeries. Current options include canal-based, subconjunctival and suprachoroidal procedures.
According to Manjool Shah, MD, who’s in practice at NYU Langone Health in New York City, nearly all glaucoma patients are potential MIGS candidates, unless they rule themselves out. “The discussion with patients regarding the likelihood of success and expectations will be tailored to the individual and his or her particular disease state,” he says. “If the kind of glaucoma that we’re dealing with will work really well with canal-based procedures, then we’re going to lean in a little bit harder. If not, then the conversation about intervention is going to be about using a tailored, stepwise approach to arrive at the least invasive surgical solution that optimizes safety and efficacy, recognizing the fact that there is a chance that we would have to return to the operating room and do a bigger procedure. The choice of a more invasive, but more powerful procedure versus smaller stepwise increments is often left up to the patient, with my guidance. Different patients have different goals and we want to optimize different attributes, such as time away from work, number of surgical interventions, comfort of the eye, etc.”
The Three Varieties of MIGS Procedures
Most MIGS procedures are Schlemm’s canal-based. Stents, goniotomies and canaloplasty all fall into this category. Dr. Shah lists the three versions of canal-based stents currently available to surgeons: iStent Inject (Glaukos); iStent Infinite (Glaukos); and the Hydrus Microstent (Alcon). Goniotomies can be performed with various devices like the Kahook Dual Blade (New World Medical), the SION (SightSciences), and the TrabEx (MicroSurgical Technology), or can simply be performed with a Sinskey hook or a bent needle (bent ab interno needle goniotomy, or BANG). Circumferential goniotomies can also be performed using devices like the Omni (Sight Sciences), iTrack or iTrack Advance (Nova Eye Medical), or with suture-based gonioscopy-assisted transluminal trabeculectomy (GATT). Canaloplasty, or viscodilation of Schlemm’s canal and distal outflow structures, can be performed with iTrack and iTrack Advance or Omni as described above, as well as with iPrime (Glaukos).
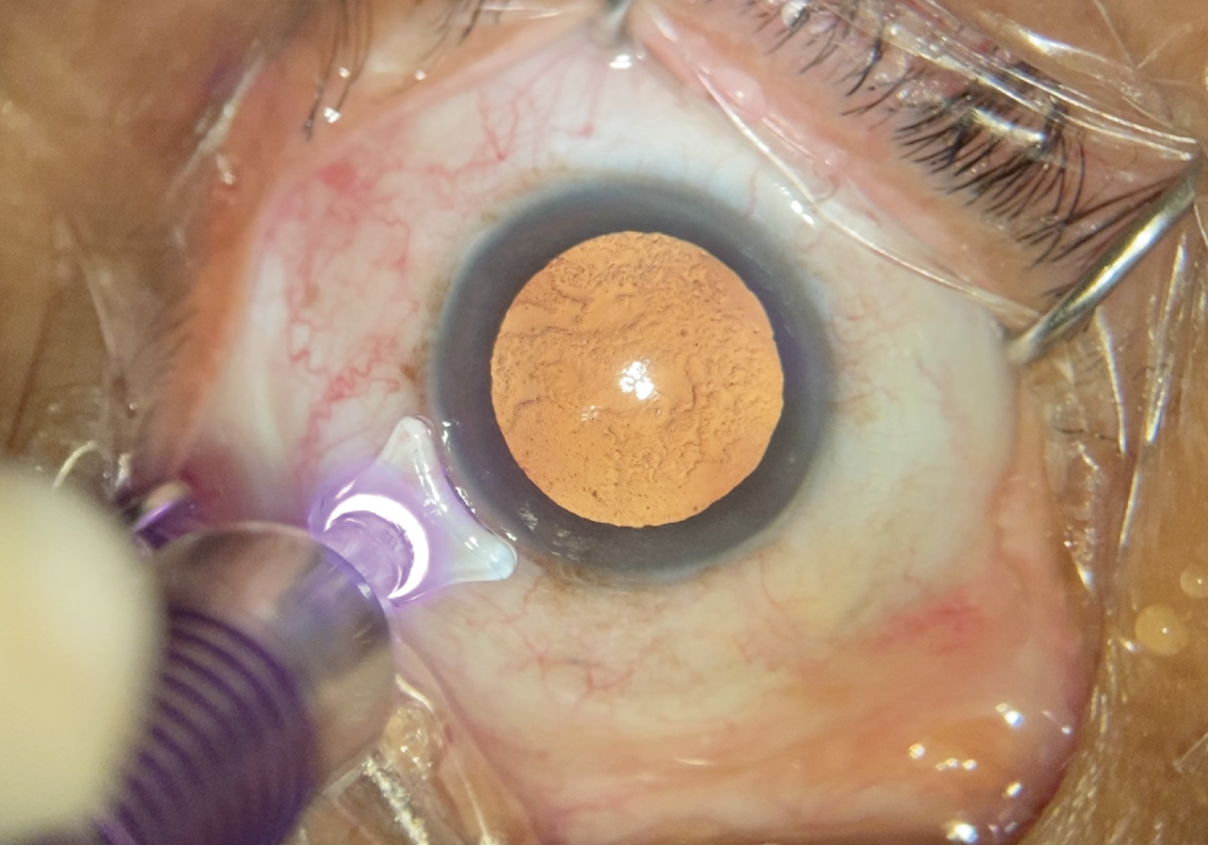 |
| Figure 1. Some surgeons combine Micropulse cyclophotocoagulation with the patient’s cataract surgery. (All images: James T. Murphy, MD) |
“There are also two laser-based procedures currently in clinical trials—femtosecond laser image-guided high-precision trabeculotomy (FLigHT) by ViaLase and excimer laser trabeculostomy (ELT) by Elios,” Dr. Shah adds.
Xen (Allergan) is the only subconjunctival MIGS device approved for use in the United States. “PreserFlo (Glaukos), which some would call MIGS, is available outside the United States,” Dr. Shah explains. Conventional procedures like trabeculectomy and glaucoma drainage devices also fall into the category of subconjunctival procedures.
Suprachoroidal procedures include the MINIject (iStar Medical) and Allopass (Iantrek), which are currently in clinical trials in the United States.
“I like to think about the three big families [of MIGS] as setting the tone because canal-based procedures may not cut it in some patients. In those situations, U.S. surgeons move to the subconjunctival set of options. Outside of the U.S., surgeons may consider the suprachoroidal option as an intermediary or in patients who aren’t good candidates for subconjunctival outflow procedures,” Dr. Shah says.
“Now that we have all of these tools to manage glaucoma, we need to broaden our definition of success. Pressure reduction isn’t the only marker of success,” Dr. Shah notes. “Reducing medications and achieving steadier IOP in terms of diurnal fluctuations could be an endpoint. Quality of life and patient-reported outcomes are also going to be relevant endpoints, because ultimately our goal as physicians is to help patients lead their best lives. As an example, you could have a patient who’s on two bottles of eyedrops with a pressure of 14 mmHg but, after surgery, he or she is on no medication with a pressure of 15 mmHg. By conventional criteria, that would be a surgical failure, but I would argue that’s a huge win because you took that patient from two bottles to zero bottles of medication. I’m sure that patient would be thrilled.”
“While we definitely incur a little bit more risk as we move up the algorithm from canal surgery to subconjunctival surgery, we have to balance that level of risk tolerance with the likelihood of success based on the individualized success criteria we have for that person, that eye, and that disease state. I am hopeful that, with improvements in big data and AI, we will continue to develop more powerful decision support tools that enable surgeons to make these nuanced surgical choices more confidently,” he explains.
 |
| Figure 2. The iTrack Advance performs 360-degree canaloplasty and doesn’t involve the implantation of a stent. |
Matching Patients To Procedures
When choosing a procedure, James T. Murphy, MD, who is in practice in Hamden, Connecticut, says that he considers the severity of the glaucoma, the IOP, corneal thickness/hysteresis, the number of medications that the patient is taking as well as their efficacy, and the patient’s ability to tolerate any side effects of his or her current medications, which affects the likelihood of drop compliance. “Field characteristics are also important,” he says. “Someone with severe glaucoma or a fixation-threatening field deficit is at higher risk of snuff-out and is more likely to require a bleb. For others, the more severe the glaucoma is and the more eyedrops he or she is on, the more likely I am to combine MIGS procedures synergistically.”
Leonard Seibold, MD, who is in practice in Aurora, Colorado, also considers the target pressure and whether or not the patient has controlled pressure on medications or uncontrolled pressure. “That changes things a little bit,” he says.
He also considers whether the angle is open or closed and whether or not the patient has a cataract. “The severity of a patient’s disease and his or her tolerance for risk are important,” Dr. Seibold adds. “For milder disease, we’re not willing to tolerate a huge risk in the procedure that we choose, whereas for more severe disease, we’re willing to tolerate higher risk to get a more robust reduction in pressure.”
He also assesses any risk factors that a particular patient may have. “For example, if a patient is at risk for blood reflux or bleeding, you may want to shy away from a goniotomy procedure that is more likely to result in a hyphema,” Dr. Seibold says. “If the patient is uveitic or has a history of macular edema, I would steer away from doing a micropulse laser or endoscopic cyclophotocoagulation procedure that would put the patient at higher risk for developing macular edema afterward.”
Patients with open-angle glaucoma have the full range of options available to them. However, having closed-angle glaucoma takes stents off the table. “I like ECP a little bit more in a closed-angle patient, but you can also perform goniosynechialysis using a Kahook Dual Blade and then perform a goniotomy,” he adds.
For patients who have very mild disease and who are on one or two medications, Dr. Seibold chooses a procedure that’s less invasive, lower risk and less disruptive to the tissue. “Choices include iStent, Streamline (New World Medical) or even Hydrus,” he says. “Canaloplasty can also be a good option. But for more moderate disease, I’m turning more toward goniotomy, with the Kahook Dual Blade, with or without canaloplasty. I don’t think stents or canaloplasty have as much of a role when you get to severe disease, and I think goniotomy or ECP, or perhaps a combination of the two, can be used—so you combine an inflow and an outflow procedure. Again, when you have more severe disease, you’re willing to tolerate more risk, so combining two procedures to really maximize the effect for MIGS is what I’m typically turning to in those scenarios. I’m trying to avoid or push traditional surgery further down the line if possible.”
Dr. Shah says he almost always chooses canal-based surgery as his first attempt, unless he feels like it won’t produce the desired result. “Canal-based procedures may not work as well in patients who have severe primary open-angle glaucoma,” he says. “The two-year outcomes from GATT show that the efficacy trails off as the severity of the disease goes up, but that assumption is being challenged a little bit by the most recent iStent infinite data, which show a decent efficacy in reasonably severe patients who have a pretty complicated history. They’d had multiple procedures, pretty severe disease, high pressures, a lot of medications, and they actually did well. This book is being rewritten constantly, but the standard belief is that canal procedures don’t work as well in severe primary open-angle glaucoma. This, however, is in contrast to how well they work in secondary open-angle glaucoma.”
He adds that patients with pseudoexfoliative glaucoma, pigmentary glaucoma, uveitic glaucoma and steroid-induced glaucoma do remarkably well with canal-based procedures, often even when they have severe disease. “So, the type of disease, as well as the severity, play a role in whether we would try a canal-based procedure or would move to some of these other options, which are fundamentally not physiologic,” he explains. “So, there’s always an appeal to try to tap into physiologic pathways whenever we can, but, again, if that option isn’t available, then we go subconjunctival.”
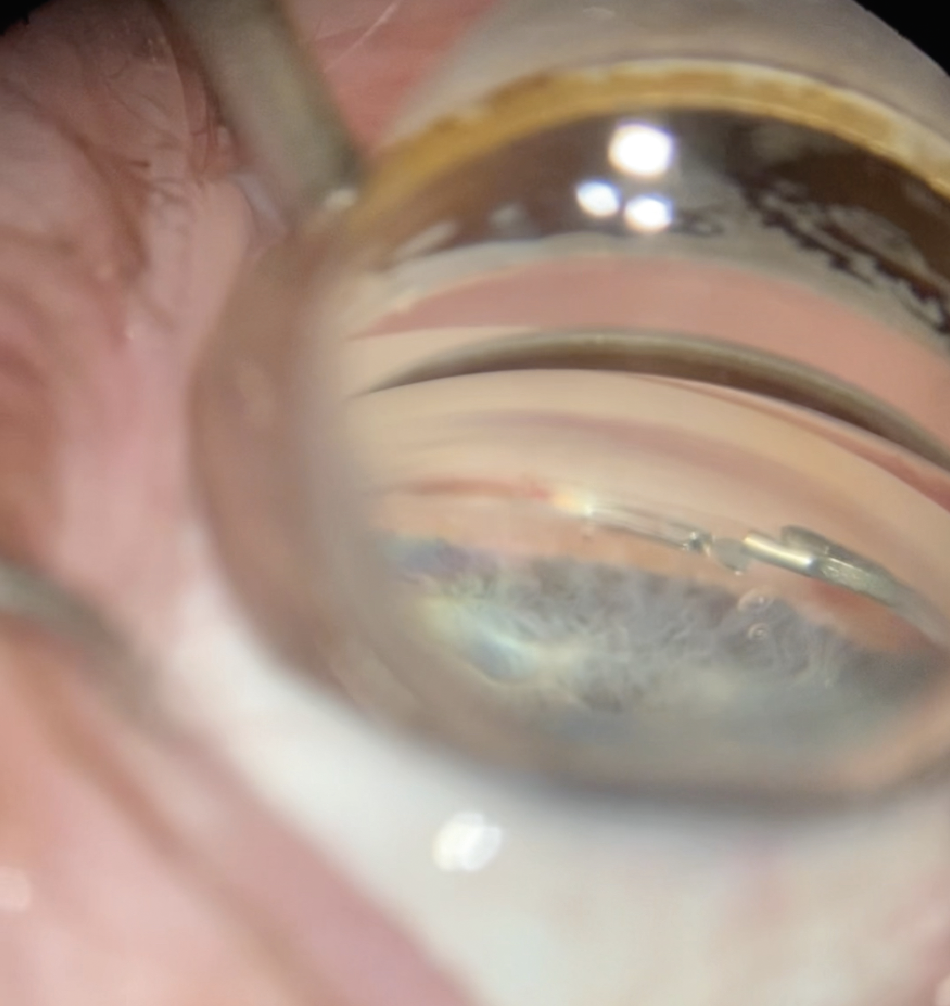 |
| Figure 3. Some surgeons combine the Hydrus micro-bypass stent with ECP, since the latter leaves the trabecular meshwork intact. |
Dr. Murphy often combines up to four MIGS procedures. “I will perform either micropulse, traditional transscleral cyclophotocoagulation, and/or ECP when I’m performing cataract surgery, and then I’ll subsequently perform either goniotomy or canaloplasty, but often a combination of both,” he says. “Leaving the trabecular meshwork intact in the nasal quadrant as a scaffold allows for placement of one of the trabecular meshwork micro-bypass stents, which I will consider in mild or moderate primary open-angle glaucoma patients, as I’m constrained by insurance coverage in the United States. These are my full-court-press patients.”
He explains that whether you’re considering one, two, three or even four MIGS procedures, patient expectations are important. “I like to do dropless surgery if and when possible, as one of the most significant barriers to success is ‘the patient factor,’ meaning the patient’s responsibility burden postoperatively,” Dr. Murphy says. “If dropless isn’t an option, I default to a 503A compounded postoperative eyedrop. Depending on the patient’s glaucoma severity, I will at a minimum streamline the patient’s glaucoma medications to one or maybe two, but often I simply perform a washout and add back as needed in the postoperative period.”
He notes that his goal is one or two drops per day while maintaining target IOP after combined cataract and MIGS procedures. “Let’s say you have mild glaucoma, you are on two, three, or four aqueous suppressants, and your pressure is upper teen or low 20s with an average corneal thickness. It’s entirely reasonable to reduce that patient’s drop burden to one or none while achieving a mid- to low-teens stable IOP for years after their surgery,” he adds.
What’s New?
Dr. Seibold says that Streamline (New World Medical), which came to the market in the past year or two, can be useful. “The device performs goniotomy and canaloplasty at the same time,” he says. “Streamline makes micro-goniotomies that can be widened to a more linear goniotomy. It’s effective and safe for mild to moderate patients, but it can also be used to extend to a longer goniotomy if more of an IOP reduction is needed. Then, there’s a new version of the Omni called the Omni Ergo (Omni Surgical). It works the same, but has some ergonomic improvements to make the procedure a little smoother. Also, the iTrack device, a lighted catheter which is used to perform a 360-degree canaloplasty, has a new version called iTrack Advance. Previously, the iTrack was a freestanding catheter that had to be fed in using forceps from a separate incision. Now, the catheter is fed through a single handpiece, which ergonomically makes the procedure easier. One fewer incision is required, allowing the procedure to be completed all through your main incision like most other MIGS.”
He believes that MIGS are here to stay and that there may be a few new approaches coming soon. “One would be in the suprachoroidal space,” muses Dr. Seibold. “Currently, some new stents are in clinical trials, and they’ll be placed in the suprachoroidal space. In the future, I think we’ll also combine MIGS with extended drug release, using a MIGS plus meds approach to maximize outcomes.”
Dr. Shah is a consultant to Glaukos, Elios, Alcon, and Abbvie/Allergan. Dr. Seibold is a consultant for New World Medical and Allergan. Dr. Murphy is a consultant for Sight Sciences and Nova Eye.
Article has been edited to provide the correct term for ViaLase's glaucoma procedure.



