The advent of accommodating, multifocal and toric lenses has enabled us to provide better visual outcomes for our patients and a decreased dependence on glasses. While these aren't quite the fountain of youth, we can give patients a wide range of vision and a better refractive result than ever before.
However, these enhanced outcomes come at a price, both for the patient, in terms of increased cost, and the surgeon, in terms of increased effort. For the surgeon, once you start charging patients out of pocket, you really set the bar high for the surgery and you have to be prepared to go the extra mile to deliver the best experience possible. For me, this means giving extra attention to patient preparation, as well as improving my phacoemulsification technique to create a visual system that lets the premium lens function optimally. Here are the factors I take into account.
The Surgery
Cataract surgery fixes the cataract, but refractive cataract surgery also requires that you deliver a specific postoperative refractive outcome. Steps that didn't seem as critical for routine cataract surgery, such as an exact determination of your surgically induced astigmatism, take on increased importance when you're implanting a premium lens, since the optics have to be just right in order for the lens to work correctly.
Here are the important issues to keep in mind, and some techniques you can use to ensure better outcomes.
• Know your induced astigmatism. We've all learned that, no matter what type of incision you make on the cornea for cataract surgery, it's going to cause some astigmatic effect, and you have to take that into account. This is even more crucial when you're implanting a premium lens that re--quires a sharp visual system.
To illustrate how important this issue can become, take the example of a patient with 0.5 D of astigmatism at 90 degrees. At first glance, this may not look like much to worry about. But if you make your cataract incision at 180 degrees (3 and 9 o'clock)—which we all do—you've just turned his 0.5 D of astigmatism into 1 D, and made him unhappy.
This is important for implantation of toric lenses as well. The Alcon toric lens calculator (acrysoftoriccalculator.com), for example, asks you where your incision will be and what the effect of the incision will be, which you need to know in order to deliver accurate results. The problem is, many surgeons haven't sat down and figured out the effect of their incisions. Fortunately, thanks to the excellent work of
Dr. Hill has made available a free computer program to help you calculate surgically induced astigmatism. You can get the program at doctor-hill.com. To use the program, you simply enter in key bits of data, such as your preop and postop steep and flat K values and meridians, and the program will calculate how much astigmatism you usually induce and at what meridian.
In terms of what would be a "tolerable" amount of spherical defocus for a premium lens, for most multifocal lenses and accommodating lenses the best results are when the patient has a sphere that's ±0.5 D of
• Consider smaller incisions. Though bimanual surgery never really caught on in the
There are astigmatism benefits to smaller incisions. When we did 3.5- to 4-mm incisions for foldable IOLs, there was nearly 1 D of astigmatic flattening because of our incisions. Then, with 2.8- to 3-mm incisions, this dropped to about 0.5 D. And now with 1.8- to 2.2-mm incisions there is only about 0.25 D of astigmatic effect.
Another advantage of small-incision phaco is that we have less fluid going through the eye. Large volumes of fluid running through the anterior chamber can knock off endothelial cells and affect other structures, and it's just not preferable to run this much fluid through the eye if we can help it.
Fortunately, in order to adapt to smaller-bore needles and tips, the phaco machines give us increased flexibility with parameters, particularly with the vacuum range. The machine settings need to be changed for micro-coaxial phaco due to the flow restriction from smaller tube sizes. Think of the analogy of a milkshake and drinking straws. Micro-incision coaxial is like drinking a milkshake with a narrow cocktail straw: High vacuum is required in order to achieve modest flow. Large-incision coaxial is like using a large-bore straw: Lower vacuum can be used and much higher flow achieved.
The adjustment for surgeons is to operate under higher vacuum and lower flow. Initially, this means things will be happening more slowly in the eye than when the flow rate is higher. Recommended settings include: increasing the bottle height to increase infusion pressure and inflow; keeping the pump outflow rate lower than the inflow rate to prevent surge; and increasing the vacuum level to improve aspiration of cataract pieces.
I think micro-phaco makes for more stable fluidics in the eye, since the lower flow means so little fluid is moving into and out of the eye. With appropriate inflow and outflow rates, the stability of the anterior chamber is better. This stability is key when implanting premium lenses, because a complication from an unstable chamber, such as a torn posterior capsule, can mean you can't implant the premium lens. For instance, a torn posterior capsule prohibits you from implanting a Bausch & Lomb Crystalens and any Alcon single-piece AcrySof lenses, including the toric and the one-piece ReSTOR.
Certain lenses, however, such as a three-piece ReSTOR lens or a three-piece Tecnis multifocal, can still be implanted by placing them in the sulcus with optic capture behind an intact capsulorhexis.
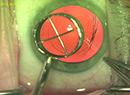
• Use the right size capsulorhexis. Like the foundation of a house, your capsulorhexis is the groundwork on which you build your premium lens implantation. The capsulorhexis must be the size you need for the particular lens you're using. We've determined that with the Alcon toric lens or any of the multifocal lenses, you've got to have a capsulorhexis that's consistently smaller than the optic. So, if the optic of one of these lens types is 6 mm wide, we want a 5- or 5.5-mm capsulorhexis. This allows the capsulorhexis to "shrink-wrap" down and hold the optic in place. If the rhexis is too large in a toric implantation, the lens will rotate because it's not held in place. If you have an irregular capsulorhexis for a multifocal lens, the lens won't be held in the patient's visual axis and instead may be decentered.
A larger sized capsulorhexis is preferred for the Crystalens. For this lens, you actually need a capsulorhexis that's larger than the 5-mm optic size. This is because the Crystalens' operation involves some motion, and you don't want it impeded. It's best with a 5.5- to 6-mm capsulorhexis.
One way to get a properly sized capsulorhexis is to use a 5.75-mm optical zone marker to leave temporary indentations on the cornea. If your capsulorhexis follows the marks on the cornea, the resultant capsule opening will be 5 mm. Mastel makes a 5.75-mm capsulorhexis marker that's useful for this method.
Personally, I use a Storz capsulorhexis forceps (Bausch + Lomb) that I designed that has hash marks 2.5 mm and 5 mm from the tip. So, as I'm tearing the anterior capsule, I can use my forceps tip to measure how big the capsulorhexis is. If I want it 5 mm, I make it exactly to that hash mark. If I want a 6-mm capsulorhexis I take it a millimeter beyond the 5-mm mark.
Another method that's in development for making an accurate capsulorhexis uses the femtosecond laser. The LenSx laser is currently FDA- approved for anterior capsulotomy, while its two competitors, LensAR and Optimedica, are working toward approval of their devices.
Viscoelastics also play a role in making a good capsulorhexis. Highly cohesive or visco-adaptive ophthalmic viscosurgical devices such as AMO's Healon5 and Healon GV make a capsulorhexis easier to perform because they flatten the anterior lens capsule and give you more control over capsulorhexis creation. These cohesive OVDs do a great job of holding space, but they can be washed out of the eye during phacoemulsification if a high flow rate is used. In contrast, the dispersives—often the OVDs with "coat" in their name—are like molasses in their ability to coat structures. Dispersives like Viscoat and OcuCoat are good for protecting the endothelium and posterior capsule during surgery. Because of the differences in OVDs, most surgeons end up using a two-viscoelastic system such as Abbott Medical Optics' combo-pack of Healon and Healon5 or Alcon's combination of Viscoat and ProVisc.
In order to combine the benefits of both dispersives and cohesives, I sometimes use the soft-shell technique described by Steve Arshinoff, MD. The technique involves injecting a dispersive viscoelastic first to coat the endothelium, and then putting in a mass of the cohesive viscoelastic centrally, which pushes the dispersive OVD out towards the cornea and flattens the anterior lens capsule. I may then put in an additional dispersive to recoat the endothelium and protect things later in the case. At the end of the surgery, I'll use a cohesive to open up the empty capsular bag to prepare for my lens insertion. I use the cohesive to open the bag because, once the lens is in, a cohesive OVD can be aspirated out quickly and fully.
• Minimize the phaco energy. Minimizing the energy placed into the eye helps to preserve the delicate corneal endothelium to achieve clear corneas immediately postop. If the surgeon performs a very traumatic surgery and on postop day one the patient can barely make out the big E on the Snellen chart, that patient is not going to be happy.
In terms of phaco settings, I don't think there's a magic number per se, but you must use some kind of phaco power modulation in your surgery, either a pulse mode or a burst mode. Pulse involves the machine automatically turning the energy on and off at a very fast rate, often more than 100 times per second. Burst mode delivers a very short burst of energy followed by another burst, with the rest interval between them decreasing as the surgeon steps down farther on the pedal. Both modes minimize the total amount of energy used.
So, with these modes, I can use just the bare minimum amount of energy and break up the pieces mechanically using my chopper. My goal is phaco-assisted aspiration of the cataract, with the ultrasound energy only used to assist the vacuum. This can give me effective phaco times that are a fraction of what we used in years past.
Of course, for harder lenses you'll have to use more power. However, by pulsing or bursting the energy, you'll still use relatively less power and be gentler on the cornea.
• Ensure watertight closure. Peter McDonnell, MD, did an interesting study several years ago in which he made a cataract incision on cadaver eyes and then put India Ink on the surface. He found that some of that ink was wicked into the eye, revealing that clear corneal incisions may not always seal as well as we think they do.1 Of course, this leakage is a risk for endophthalmitis. However, there can also be a slight flattening of the anterior chamber from the leak, and this is a real threat for a premium IOL, since it can cause the lens to shift.
In a toric lens, for example, if the anterior chamber slightly collapses, even minimally, and the pressure decreases, the lens is likely to slip from its correct axis and rotate out of alignment. For a multifocal that you took painstaking care to ensure was on the visual axis, when the eye deflates due to a leaky incision everything shifts and the lens decenters. A leak may be most problematic of all for the Crystalens, however, since it has to be posteriorly vaulted in the eye. If there's a leak in a Crystalens eye, the lens doesn't vault posteriorly. Instead, the lens comes forward and the patient becomes myopic. If you aimed for
Because of these issues, I check every incision using a Seidel test on the table at the end of the case to make sure the wound is watertight. If the incision's not 100-percent watertight, the solution is to place a suture, not to further hydrate the wound.
• Postop issues. The labeled indication of non-steroidal anti-inflammatory drops is just two weeks postop. Many surgeons, however, are using them for six to eight weeks postop. They're doing this not only to treat the inflammation, which is probably gone in a couple of weeks, but also to help prevent excessive fibrosis and contraction of the capsular bag. This is particularly important in younger patients and patients who are getting an accommodating lens. If these types of patients experience a lot of contraction of the capsular bag and fibrotic tissue in that area, the lens can move, shift or tilt. A longer course of postop NSAIDs, and maybe even steroids, can help prevent this and lead to a premium lens that's exactly in the position you want.
Ensuring a healthy, clear ocular surface doesn't just involve preop treatments. You have to be mindful of the surface after surgery, too. The incisions we make in the cornea during cataract surgery, which can include limbal relaxing incisions, can have an effect similar to creating a flap in LASIK in that they sever corneal nerves. This denervation makes it harder for the cornea to send the signal that it needs to produce tears. As a result, the cornea actually becomes drier, at least temporarily, which can affect the patient's postop acuity. Because of this, patients with any evidence of dry eye should be treated with artificial tears or other medications in the postoperative period.
• Manage any residual refractive error. Though this article is focused on how to alter your cataract surgery for premium lenses rather than refractive surgery techniques, it bears repeating here that you need access to some method for treating residual error. All of the premium lenses work best when you nail that
A popular way to address astigmatism is limbal relaxing incisions. The LRI nomogram I use when instructing residents, and which I think works well in general, is the nomogram of Kevin Miller, MD, a professor at the
The nice thing about Dr. Miller's nomogram is that it tends to undercorrect. As such, it's very user-friendly, especially for a first-time LRI user who may just be getting into premium lenses. For instance, say a patient has lived his entire life with 2 D of astigmatism. Now the surgeon, using this conservative nomogram, corrects 1.5 D, leaving the patient with 0.5 D. The patient will be very happy because his brain is used to living with astigmatism on this axis, and it can still process images with some astigmatic error, but now it has less to deal with.
However, if the surgeon overcorrects this patient by 0.5 D, which induces 0.5 D in the opposite meridian, the patient will be dissatisfied. This is because he's used to having astigmatism at the 12 o'clock and 6 o'clock meridian, but now he has it at a completely different meridian—3 and 9 o'clock—which is all new to his brain. It's almost as if patients have astigmatism of the brain, too. So undercorrecting the astigmatism isn't always a bad thing.
As surgeons get more comfortable with performing LRIs, they can advance to the Nichamin nomogram which is adjusted based on the patient's age and pachymetry.
For patients receiving premium IOLs, we need to elevate our surgical technique and planning in order to give them premium phaco. And patients who achieve excellent visual outcomes after surgery will be happy and inclined to tell their friends and family about the benefits of refractive cataract surgery.
Dr. Devgan is in private practice at Devgan Eye Surgery in
1. Taban M, Sarayba MA, Ignacio TS, et al. Ingress of ink into the anterior chamber through sutureless clear corneal cataract wounds. Arch Ophthalmol 2005 May;123:5:643-8.