Among the many advanced-technology intraocular lenses now available to ophthalmologists, one of the most commonly used is toric lenses. Originally only available in monofocal designs, torics have now expanded to include multifocal and expanded-depth-of-focus lenses. Here, surgeons with expertise in measuring astigmatism and implanting and aligning these lenses share strategies to improve your outcomes.
Using the Right Technology
The first step when deciding whether a toric IOL is appropriate for a given patient—and what power to implant—is measuring the astigmatism of the eye. In terms of which instruments should be used to make those measurements, a 2019 clinician survey conducted by the American Society of Cataract and Refractive Surgery found that most surgeons, both in the United States and around the world, rely on topography and automated keratometry to guide them in their toric IOL power selection.
“If you’re going to fix astigmatism, you need to be able to measure it and see it,” notes George Waring IV, MD, FACS, founder and medical director of the Waring Vision Institute in Mount Pleasant, South Carolina. “Astigmatism can be regular or irregular, and regular astigmatism can be against-the-rule, with-the-rule or oblique. You need to be able to see it because you won’t necessarily be able to tell whether your patient’s astigmatism is regular or irregular unless you can visualize it. So you need either a topography or tomography device to understand the quantity, quality and orientation of the astigmatism. That’s essential. Ideally, you’d also have the ability to evaluate the total keratometry, which includes the anterior and posterior corneal contribution to the astigmatism. Multiple devices can give you this, including the IOLMaster 700, the Lenstar, the Pentacam and corneal OCTs.
 |
“In our practice we factor in the topography by using a weighted mean of the topographic and IOLMaster astigmatism readings,” he continues. “Beyond that, because we’re doing lens surgery earlier and earlier, we also consider the manifest refraction in younger patients. In addition, Hartmann-Shack wavefront aberrometry can give you useful information to supplement the manifest refraction guidance in many cases, but wavefront information certainly isn’t essential.”
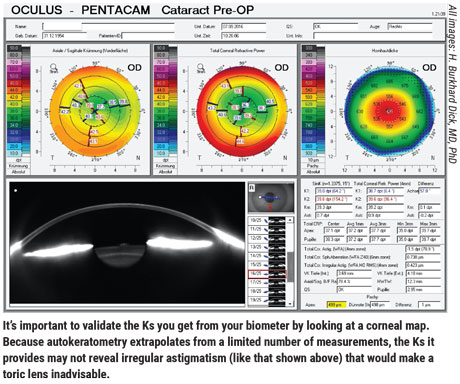
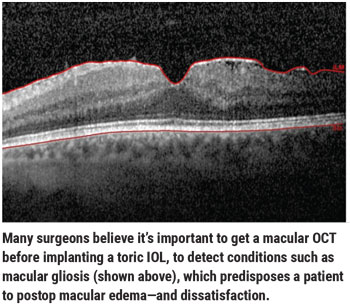
H. Burkhard Dick, MD, PhD, FEBOS-CR, director and chairman of the University Eye Hospital in Bochum, Germany, believes that corneal tomography, which assesses both anterior and posterior cornea, is very useful. “This is of prime importance when smaller degrees of astigmatism are at issue, which is true in most of our cases,” he notes. “A macular OCT is also valuable for checking to see if the patient has, for instance, macular gliosis, which predisposes to postoperative macular edema, and thus considerable patient dissatisfaction.”
Dr. Waring notes that whether or not a toric IOL is a good solution for an eye with irregular astigmatism depends on the specifics of the eye in question. “A toric lens may not be able to address irregular astigmatism adequately,” he points out. “However, in some cases it can. In the case of asymmetric bow ties, we’d be conservative and treat the least amount of astigmatism in the hemi-meridian, as opposed to the full amount in the opposing hemi-meridian. We also use the manifest refraction to guide us in our decision-making, in terms of what the patient will accept at the spectacle plane. Of course, if it’s a markedly skewed radial axis, as it could be in a case of keratoconus, then the patient might not be a great candidate for a toric lens because toric lenses have radial symmetry.”
Dr. Dick recommends using one of the established online calculators, such as the Donnenfeld calculator, to make a decision about whether a toric lens is really indicated for a given patient. “I’d hesitate to implant a toric lens if irregular astigmatism is involved,” he adds. “I’d also be reluctant if there’s a probability of keratoconus, or in the presence of major ocular pathologies like gliosis, macular degeneration or diabetic retinopathy.”
Interpreting the Data
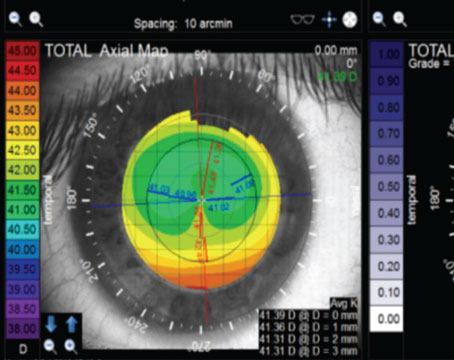
Warren E. Hill, MD, medical director of East Valley Ophthalmology in Mesa, Arizona, notes that when choosing a toric IOL, it’s helpful to first determine whether the type of astigmatism the patient has is appropriate. “Using a topographic or tomographic axial curvature map, look to see how the power is distributed across the anterior cornea within the central 4 mm,” he says. “A pair of symmetric, astigmatic power lobes straddling the corneal vertex, with each lobe aligned along the same meridian, represents regular, symmetrical astigmatism. This is the ideal situation for a toric IOL.
“Next, look to see if a line can be passed through the corneal vertex and the center of each astigmatic lobe,” he continues. “Where this line intersects the axis scale in the periphery is, by definition, the steep meridian. If we can’t draw a single line representing one meridian through both astigmatic lobes, the astigmatism is then termed irregular.”
Another fundamental aspect is determining whether the astigmatism is symmetrical. “If the power distribution on either side of the corneal vertex is very different, it’s termed asymmetric,” Dr. Hill explains. “Elevated coma values are often associated with this type of topographic map, especially if an astigmatic lobe is present on only one side of the corneal vertex. Placing a toric IOL in this situation may result in variable amounts of image duplication and displacement with larger pupil sizes.”
Dr. Hill says that if the astigmatism is both regular and symmetrical, and you’ve accurately identified the steep meridian, the next step is to determine the power difference between the two principal meridians. “Here, we use the steep meridian that was determined manually from the topographic axial curvature map to validate the power difference,” he notes. “This power difference is often best determined with the autokeratometry feature of the Lenstar, IOLMaster, or other similar technology; simulated Ks shouldn’t be used for this exercise. Note that if you’re confident about the steep meridian but the autokeratometer is telling you something different, the Ks are most likely being measured at an incorrect location.”
Dr. Hill notes that simply relying on a set of Ks from your biometer may lead to a poor outcome if you don’t also look at a topographic axial map. “The topographic axial curvature map tells you whether you’re dealing with regular and symmetrical astigmatism and lets you manually determine the steep meridian,” he says. “This helps to validate the power difference calculated by autokeratometry, which will be less accurate if the meridians aren’t correctly identified.”
Managing Posterior Astigmatism
Some instruments can now provide accurate measurements of the posterior corneal surface and its refractive power and astigmatism. Is it worth measuring this directly? “In a perfect world we’d specifically measure the posterior corneal astigmatism,” says Dr. Waring. “However, many offices don’t have the technology to do that. If you’re not going to measure that, it’s very important to use a population-based nomogram.”
 |
“At the present time, in normal eyes the mathematical models used by the Barrett and the Abulafia-Koch methods [to calculate optimum astigmatism correction] appear to be more accurate than using direct measurements of the posterior cornea,” Dr. Hill says. “However, you shouldn’t use mathematical models for unusual eyes—such as those with keratoconus, penetrating keratoplasty or prior refractive surgery—or with Ks determined by total corneal power. For unusual eyes, a direct measurement of the posterior cornea is preferable, along with the use of the Barrett True K toric calculator. This can be accessed at: calc.apacrs.org/TrueKToric105/truektoric.aspx.”
“In eyes with high astigmatism, the posterior astigmatism is virtually irrelevant,” Dr. Dick points out. “However, in astigmatism of 1.5 D or less, posterior astigmatism does play a role. A meticulous surgeon may choose to measure both anterior and posterior astigmatism and calculate the ‘true net power,’ which determines the refractive power, but some formulas, like the new Barrett formula, quite effectively predict posterior corneal astigmatism.
“I’ve seen a few cases where an eye had as much as 0.4 D of posterior astigmatism,” he adds. “That becomes relevant if the overall astigmatism that one is trying to correct is around, say, 1 D. However, in my experience eyes like that are rare.”
Marking the Axis
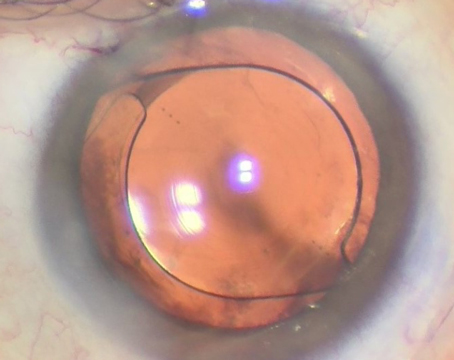
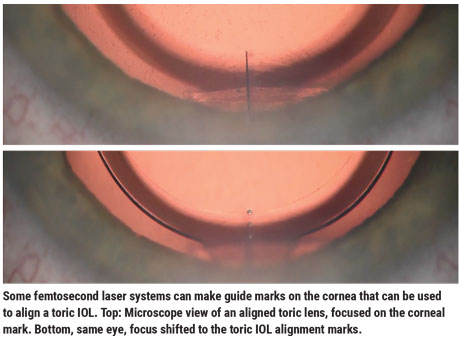
Many surgeons still rely on marking the cornea with ink to guide alignment of the implanted toric IOL, but higher-tech options are proliferating and becoming more widely used. For example, Dr. Hill says that his practice guides toric axis alignment by creating anterior capsule tags using the LensAR femtosecond laser, obviating the need to use external corneal marking.
Dr. Waring says that he uses a femtosecond laser to create 10-degree intrastromal femtosecond laser marks in the cornea. “These marks are archival,” he notes. “That means we not only have an intraoperative registration, we have a postoperative archival registration that makes it easy to see if the toric lens has rotated.
“Today there are more and more options to use for aligning the lens, such as intraoperative light and registration overlays,” he continues. “For example, Zeiss’ Callisto does a real-time overlay for toric marking; that’s one of the more elegant ways to align with corneal astigmatism. In addition, more and more femtosecond laser platforms are offering customized capsulotomies to identify and register the astigmatic axis to front end topographic diagnostic devices. However, we believe that using ink marks is still a great idea, particularly if you eventually transition into more advanced technologies. There’s certainly no harm in doing both.”
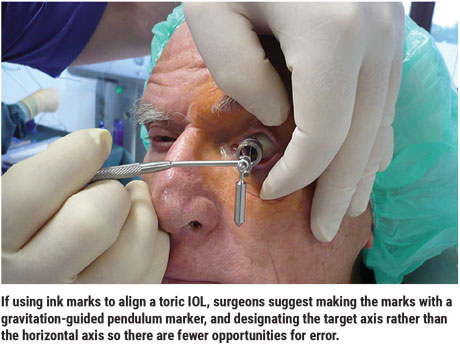
Dr. Dick says that while he appreciates the advantages of high-tech alignment technologies, he believes ink marks are still the gold standard. He offers several pearls for using this approach:
 |
“It’s important to use a gravitation-guided pendulum marker and designate the target axis rather than the horizontal axis,” he says. (See photo, facing page.) “When you have the patient sitting at the slit lamp and you mark the horizontal sector to use as a reference mark on the operating table, you may already be off by about five degrees. Having to then locate the alignment axis with a Mendez ring on the operating table means you have two opportunities for error. If you’re trying to correct 1 or 1.5 D, this might be clinically irrelevant; but with high levels of astigmatism, any additional error leads to ever greater deviation.”
Dr. Dick says using the right kind of marker makes a difference. “It needs to be a marker that makes slim markings and comes with four rather than two contact points,” he says. “However, remember that a very fine marking might fade away by the time of surgery.”
Dr. Dick believes the ideal option for alignment is laser-guided high-definition iris recognition, with an adjustment for measurements taken when the patient was sitting. “It’s also excellent to place laser marks in the capsulotomy, or mark the target axis on the cornea using a femtosecond laser, a technique we recently published about,” he says. “This method eliminates almost all sources of error, like confusing the left with the right eye. The software will intervene and tell you that you’re not targeting the correct eye.”
Minimizing Lens Rotation
It goes without saying that after going to great lengths to get the toric IOL aligned with the correct axis, the last thing a surgeon wants is to have the lens rotate.
“To ensure minimal rotation of the lens, you should take certain steps during the surgery and then counsel the patient about how to behave during the postop period,” says Dr. Waring. “Intraoperatively, you want to do several things. First, make sure you remove all viscoelastic from behind the optic. Second, place a small amount of posterior pressure on the optic, to seat the optic and haptic in the posterior portion of the capsule. Third, use the I/A tool to hold the IOL in place during irrigation and aspiration. Fourth, ensure that you’ve adequately sealed your wounds.”
Dr. Hill says that when he implants an Alcon AcrySof toric IOL, he seats the IOL with gentle downward pressure, using the I/A tip to initiate an interaction between the posterior surface of the optic and the posterior capsule. “Also, at the end of the case, don’t over-inflate the eye with BSS,” he adds.
Dr. Waring adds that it’s also important to educate the patient about postop behavior. “It’s critical to explain to your patients that they need to avoid rubbing or wiping their eyes, especially during the first week postop,” he says. “Any outside pressure can increase the likelihood of toric rotation. Typically, if the lens is going to rotate it will happen during the first week, with the first 48 hours being the most critical.”
 |
Of course, despite all of your efforts, some toric IOLs may rotate postoperatively. Dr. Waring says he considers four metrics when deciding whether or not to go back in and correct the alignment of a toric lens. “First of all, is the patient aware of a visual problem?” he says. “Second, is their measured uncorrected visual acuity being affected by the alignment offset? Third, can we see under the microscope that the alignment is off by five degrees or more? Fourth, can we show with advanced technology, such as the ray-tracing technology in the iTrace toric check or the Berdahl-Harden toric calculator, that rotating the lens would improve things?”
Dr. Waring notes that he would typically check these things if the patient had a subjective complaint. “Of course, my team always checks the IOL position under the microscope on day one postop,” he says. “That’s especially easy to do if you have the archival femtosecond laser marks.”
Pearls for Success
These strategies will help to ensure that your toric IOL patients get the best possible outcome:
• Always validate the Ks you get from your biometer. Dr. Hill notes that failing to do this is one of the most common mistakes clinicians make. “Autokeratometry extrapolates from a limited number of measurements,” he points out. Therefore, it’s important to verify that the steep meridian manually obtained by autokeratometry agrees with what you know to be correct.”
• Look for signs of amblyopia. Dr. Dick points out that testing the visual acuity in both eyes is the first step to take with a potential toric IOL patient. “This is mainly to exclude amblyopic eyes,” he explains. “Using a toric IOL in an amblyopic eye is questionable, especially in very amblyopic eyes. If the first eye is amblyopic, then fixation will be insecure, making it possible to have measurement errors in both refraction and tomography. Moreover, dissatisfaction with the result in the first eye may lead the patient to refuse a toric IOL for the better eye, where it would really make sense if that eye has greater corneal astigmatism than the first eye.”
• Be aware of pupillary distortions. “Pupillary disturbances and distortions—like constantly large pupils—are also reasons to refrain from implanting toric IOLs,” notes Dr. Dick. “Pupil distortion can have an impact on the physiological compensation for existing or postoperative astigmatism, in terms of optics. Pupil distortion can decrease or increase the astigmatism, depending on the orientation of the distortion in relation to the steep corneal axis. A small oval mask in the IOL (analogous to the small round mask in the IC-8 from Acufocus) is definitely capable of compensating for corneal astigmatism if appropriately oriented.
“Pupillary distortion,” he adds, “as well as non-uniform medical mydriasis, can have an impact on astigmatic axis detection if it’s based on digital iris recognition.”
• Be prepared to use special means to prevent rotation in cases of high myopia. “High myopes may have a large capsular bag with a diameter greater than the standard total diameter of a toric IOL,” notes Dr. Dick. “Therefore, there’s a greater chance of rotation in these eyes, especially with a plate haptic IOL.
“One option in this situation is posterior optic capture following a posterior capsulorhexis or capsulotomy,” he continues. “An optic capture makes any rotation virtually impossible. Using a posterior optic capture would be critical in case of a one-piece IOL, because a sharp anterior edge could cause problems such as iris shaving. Alternatively, a three-piece IOL can be implanted into the sulcus with an optic capture through a well-sized anterior capsular opening.”
• Don’t withhold offering toric options because you don’t have high-end equipment. Surgeons agree that high-end equipment isn’t necessary in order to offer your patients toric lenses. “What is essential,” says Dr. Dick, “is having the ability to perform proper marking, and the availability of corneal topography and tomography and retinal OCT.”
 |
A Great Option
“I think toric lenses should be thought of as another way to improve your patient’s vision, much like removing the cataract,” says Dr. Waring. “You should present the option to your patients accordingly. This gives them the opportunity to go beyond just fixing the cataract; they can also fix the focus of the eye.
“We believe every cataract surgeon should be offering toric lenses,” he adds. “Implanting a toric lens isn’t technically very different from normal IOL implantation, except for the biometric considerations and rotation-related considerations I’ve mentioned. It’s primarily a way to offer your patients more options and give them even better vision. It’s also a good way for surgeons to become more comfortable with advanced-technology IOLs such as presbyopia-correcting IOLs, particularly since more and more of those now come in a toric version.”
“It’s essential that we avoid implanting toric lenses in the presence of pathological conditions,” observes Dr. Dick. “However, given the prevalence of astigmatism in the general population and in our cataract patients—astigmatism that could easily be corrected with a toric IOL—we should probably be implanting far more of them than we are.” REVIEW
Dr. Dick is a consultant to LensAR, Johnson & Johnson Vision, Zeiss, Bausch+Lomb and Hoya. Dr. Waring reports financial ties to Oculus and Johnson & Johnson Vision. Dr. Hill reports no financial interests in any products mentioned.