The start of the new year is a perfect time to review updates in place for 2024 and perhaps revisit your compliance efforts to help ensure continued accuracy in your billing procedures. Here, we’ll highlight important changes for coding, reimbursement and regulations that impact ophthalmic practices.
What are the changes to physician reimbursement?
The 2024 Medicare Physician Fee Schedule (MPFS) was published in the Federal Register on November 1, 2023. The MPFS conversion factor for 2024 is $32.7442, down 3.4 percent from 2023. This is the result of many factors, including a neutral MACRA (0 percent) update to physician payments for 2024, a positive (+1.25 percent) update from the Consolidated Appropriations Act and a negative (-2.18 percent) budget neutrality adjustment. The 2 percent sequestration payment adjustment applied to all Medicare Fee-for-Service (FFS) claims is also in effect. The result is a 5.4-percent cut to Medicare rates in 2024.
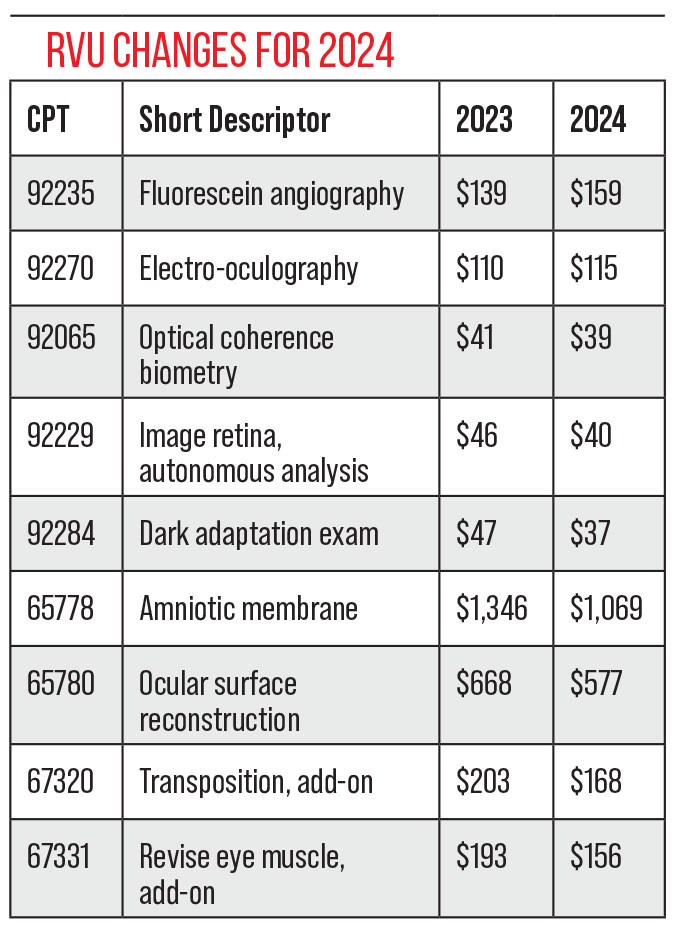
Changes in RVUs affect certain services more than others. We see increases in fees for a few codes and decreases in fees for others—the codes aren’t impacted equally.
A few of the more notable changes appear in the table below.
 |
What’s new in facility reimbursement?
Some aspects of reimbursement for facilities have been updated. Here’s a breakdown:
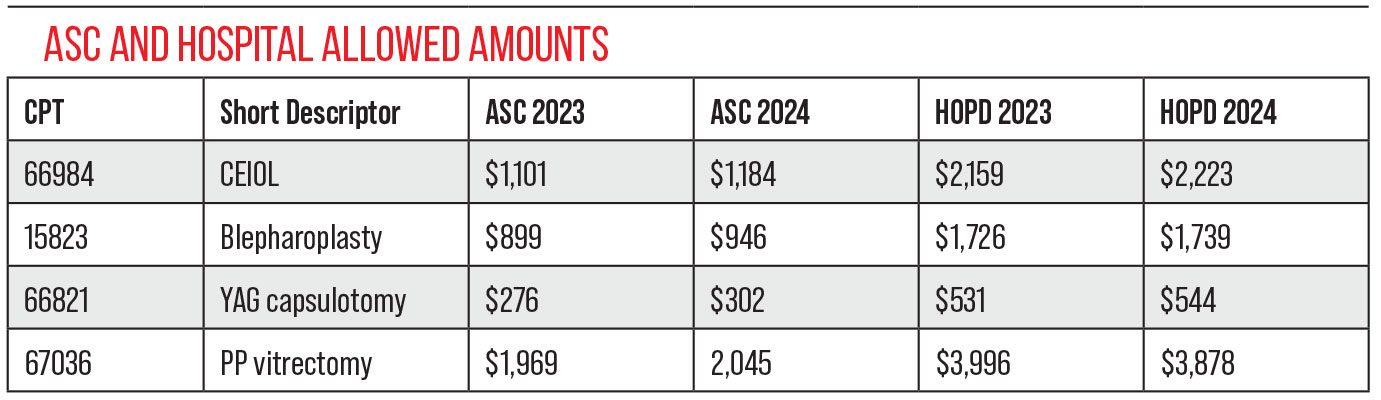
• Payment rates. For ASCs that met their quality reporting requirements there’s a 2.8-percent increase to the conversion factor; now $53.397.2 Those that failed to meet quality requirements in the most recent year will be paid based on a CF of $52.358.
Payment rates for hospital out-patient departments (HOPDs) also went up 2.8 percent. The table on page 18 lists the 2023 and 2024 Medicare ASC and HOPD allowed amounts for a few common ophthalmic procedures.
• ASC quality measures. For 2024, Quality measures ASC-1 through ASC-4 remain required. Providers will continue submitting through the HQR System for all patients, not just those on Medicare.3 Quality measure ASC-11 (Cataracts: improvement in function) remains voluntary in 2024.
• Reimbursement for Injectables in an ASC. There’s no change to ASC reimbursement for three frequently used ophthalmic drugs: Omidria (J1097); Dextenza (J1096); and Dexycu (J1095).
Omidria and Dextenza continue to be reimbursed separately in an ASC in 2024, under Medicare regulations for non-opioid pain management drugs and supplies. These won’t be paid separately in an HOPD. Dexycu doesn’t qualify as a non-opioid pain management drug; no separate reimbursement is made for it.
• New ASC eligible CPT code. The new ophthalmic surgery code (CPT 65716-Suprachoroidal space injection of medication) was added to the list of codes eligible for an ASC facility payment. The 2024 ASC allowed amount is $63.20.
• Patient surveys. The Outpatient and Ambulatory Surgery Consumer Assessment initiative was developed as part of a ‘patient experience of care’ survey, and will be required beginning calendar year 2025. For 2024, ASCs may voluntarily submit data for the survey. Facilities will contract with a CMS-approved vendor to conduct the survey. See the OAS CAHPS website for a vendor list and additional information.4
Are there notable changes to CPT coding?
The dawning of 2024 brought 230 additions to the CPT book. Forty-nine codes were deleted and 70 were revised. Code 65716, introduced above, is the only new category I ophthalmic CPT code. None of the revised or deleted codes were ophthalmic specific, although changes to E/M codes for physician time spent and the consolidation of more than 50 CPT codes related to COVID may have limited impact on ophthalmic practices.
Four category III codes that were set to expire but were renewed January 1, 2024, include:
• 0330T–Tear film imaging, unilateral or bilateral, with interpretation and report
• 0506T–Macular pigment optical density measurement of flicker photometry, unilateral or bilateral, with interpretation and report
• 0507T–Near infrared dual imaging (i.e., simultaneous reflective and transilluminated light) of meibomian glands, unilateral or bilateral, with interpretation and report
• 0509T–Electroretinography (ERG) with interpretation and report, pattern (PERG)
One new category III code was introduced, effective January 1, 2024:
• 0810T–Subretinal injection of a pharmacologic agent, including vitrectomy and one or more retinotomies
One category III code was deleted, effective December 31, 2023:
• 0456T–Suprachoroidal injection of a pharmacologic agent (does not include supply of medication).
What’s changed in HCPCS Coding?
The new HCPCS add-on code, G2211, is defined as:
“Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health-care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition of a complex condition.”
This is a CMS-generated add-on code. So far, CMS hasn’t issued instructions for its use. However, the CMS website includes a listing of pertinent “practitioner primary care specialties,” and it doesn’t include ophthalmology. Currently, it doesn’t appear that the new code will be helpful to ophthalmology in recovering any of the MPFS decrease.5
There are two other new HCPCS codes for covering the two new treatments for geographic atrophy:
• J2781 for Syfovre (pegcetacoplan injection)
• J3490 (unlisted drug) for Izervay (avacincaptad pegol intravitreal solution).
What’s new in ICD-10 coding for 2024?
Changes to diagnosis codes for 2024 are already in effect. ICD-10 changes and updates apply on October 1 each year. There were 842 new, revised or deleted codes. Those that affect ophthalmology are noted here. In many cases the code series were simply expanded to add more detail and laterality.
• H36–Retinal disorders in diseases classified elsewhere
• H36.8–Sickle-cell retinopathy
• H50.62–Inferior Oblique muscle entrapment
• H50.63–Inferior Rectus muscle entrapment
• H50.64–Lateral Rectus muscle entrapment
• H50.65–Medical rectus muscle entrapment
• H50.66–Superior oblique muscle entrapment
• H50.67–Superior rectus muscle entrapment
• H50.68–Unspecified extraocular muscle entrapment
• H52.51–Specificity added to eye and category
• H52.51–Internal ophthalmoplegia
• H57.8A–Foreign body sensation eye (ocular)
What coding requirements exist for anesthesia administration?
Since COVID-19, the shortage of anesthesia providers has impacted care at ophthalmic ASCs. Schedules had been disrupted with cases being postponed or canceled when no anesthesia provider was available. Costs have risen. Some ophthalmic surgeons and ASCs are looking for alternatives. If considering conscious sedation, know the requirements for moderate conscious sedation as detailed in the CPT handbook, including:
• qualified independent trained observer;
• continuous monitoring;
• sufficient work to support CPT billed;
• intraservice time of at least 10 minutes;
• adequate documentation;
• not MAC (Code 0014x);
• it meets state statutes; and
• the surgeon is approved for conscious sedation.
 |
What’s new in coverage for glaucoma surgeries?
Several Medicare Administrative Contractors (MACs) published revised policies for minimally-invasive glaucoma surgery in October, effective 12/24/23. One carrier, NGS, subsequently pushed the effective date to March 22, 2024. Others may follow suit. These proposed policies cover most areas in the country. Currently only First Coast Service Options, covering Florida and Puerto Rico, and Novitas Solutions—both jurisdiction JH in Texas and surrounding states and jurisdiction JL in and around Pennsylvania—are excluded.
The details of these policies are beyond the scope of this article; they affect almost all glaucoma procedures and, in many cases, greatly restrict coverage. Careful review of the policies is needed to understand the reimbursement implications.
Are there any changes to telehealth reimbursement in 2024?
The COVID-19 Public Health Emergency has ended and changes to telemedicine will take effect in 2024.6 For 2024, providers are no longer instructed to bill telehealth claims with the place of service they would have billed for an in-person visit. Instead, report claims with:
• POS 02–teleheath provided with an originating site other than the patient’s home; or
• POS 10–telehealth provided while the patient was in their home
Claims billed with POS 02 will be paid at the Physician Fee Schedule facility rate while those reported with POS 10 will be paid at the higher non-facility PFS rate. Modifier 95 is no longer needed on telemedicine claims.
Will any changes affect Medicare beneficiaries?
The Medicare Part B basic premium will increase to $174.70 for most beneficiaries. The Part B deductible increases to $240, a $16 increase.
Part C Medicare (Medicare Advantage) continues to grow. Fifty-one percent of all eligible beneficiaries were enrolled in an MA plan in 2023.7 The Congressional Budget Office estimates that enrollment will rise to about 62 percent of eligible beneficiaries by 2033.8 Penetration of Medicare Advantage plans varies widely by state.
In conclusion, coverage, coding and billing rules change each year. Staying educated on the current codes and instructions is an important aspect of your compliance efforts.
1. CMS-1784-F. CY2024 Payment Policies Under the Physician Fee Schedule. Federal Register November 16, 2023. https://www.federalregister.gov/documents/2023/11/16/2023-24184/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other.
2. CMS-1786-FC. CY2024 Outpatient Prospective Payment System. Federal Register November 22, 2023. https://www.federalregister.gov/documents/2023/11/22/2023-24293/medicare-program-hospital-outpatient-prospective-payment-and-ambulatory-surgical-center-payment.
3. CMS. Ambulatory Surgical Center Specifications Manual. Version 13.0 https://qualitynet.cms.gov/asc/specifications-manuals.
4. ASCQR Specifications Manual Version 13.0.
5. https://www.cms.gov/priorities/innovation/data-and-reports/2022/pcf-first-eval-rpt.
6. Federal Register / Vol. 88, No. 220 / Thursday, November 16, 2023 / Rules and Regulations.
7 KFF. Total Medicare Advantage Enrollment, 2007-2023. https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2023-enrollment-update-and-key-trends/.
8. May Congressional Budget Office Medicare Baseline for 2023. https://www.cbo.gov/system/files/2023-05/51302-2023-05-medicare.pdf.
Mary Pat Johnson is a senior consultant at the Corcoran Consulting Group and is based in North Carolina. She can be reached at mpjohnson@corcoranccg.com.



