Getting Back to Business
How some practices are reopening in states that have eased elective-surgery restrictions.
Several states have begun easing restrictions on elective surgeries in accordance with the guidelines issued by the White House and the Centers for Disease Control and Prevention. As practices restart important postponed care, safety is at the forefront of everyone’s mind. Screening, personal protective equipment, and social distancing are just a few of the necessary precautions being taken to continue to flatten the curve while reopening safely. Here, we’ll see how some practices in states that have begun easing their restrictions on elective surgery are going about reopening, what services they’re offering and how they’re reassuring patients that it’s safe to come back for care.
Meeting the Guidelines
The recommendation to shut down most medical services came on a specific day, but the decision to reopen isn’t as clear-cut. Academy CEO David W. Parke II, MD, noted that while the AAO issued a national recommendation to stop non-urgent treatment on March 18, decisions about resuming routine care and reopening would be made at the state and local levels and will be up to individual practices.1 Certain states have provided specific dates for reopening and resuming elective procedures, but regional restrictions may override these guidelines or impose additional criteria for businesses and hospitals to meet.
The state and regional gating criteria for Phase I reopening issued by the White House state the following:
• Symptoms: A downward trajectory of influenza-like illnesses AND COVID-like illnesses reported within a 14-day period.
• Cases: A downward trajectory of documented cases OR positive tests as a percent of total tests within a 14-day period (flat or increasing volume of tests).
• Hospitals: Treat all patients without crisis care AND have a robust testing program in place for at-risk health-care workers, including emerging antibody testing. (More information can be found at whitehouse.gov/openingamerica/#criteria.)
When it comes to meeting these gating criteria to enter Phase I reopening, “It depends how you look at it,” says Paul Sternberg, Jr., MD, G.W. Hale professor and chairman of the Vanderbilt Eye Institute and chief medical officer of the Vanderbilt Medical Group in Nashville. “The challenge with all the gating functions is testing. The number of positive cases is so linked to the amount of testing you do. If you want to have no new cases, you just don’t test people. We set up our own PCR test out of the gate, and we were testing 700 to 800 patients a day. If you look at a map of Tennessee, you’d think every single patient with COVID was in Nashville, but that’s because we were virtually the only people in the state of Tennessee who were testing.”
“We were closely following these steps and planning an opening date when suddenly most of the local hospital ASCs started operating on non-urgent elective cases,” says Daniel H. Chang, MD, of Empire Eye and Laser Center in Bakersfield, California. “As far as we could tell, some of the criteria had technically not yet been met. Then our local government announced that they would no longer enforce the statewide ‘shelter-in-place.’
“I think the most challenging aspect of this so far has been a lack of an official ‘green light’ for reopening. While the state said it was okay to resume elective surgeries, the interpretation of when it would be okay for each county and facility to reopen was not as well-defined. We’ve tried to get official guidance of when we can safely open from the local county health department, but they appear to be busy with managing other local aspects of the pandemic. Now, since most of the local hospitals and ASCs have begun opening up for non-urgent elective surgeries, the ‘standard of care’ appears to be to do elective cases.”
Opening Up By State: A Sample
Thirty-five states have eased restrictions on elective surgery.2 While reopening guidelines and requirements vary among and within states, they generally stipulate a sufficient supply of personal protective equipment; appropriate disinfection and social distancing practices; and COVID testing prior to surgery.2
California’s April 22nd stay-at-home order allowed providers to resume some elective surgeries. The state began easing more restrictions on May 1, allowing some routine and preventive care. “We started slowly with a light template to get update procedures and PPE practices in place,” says Dr. Chang, who personally survived a case of the coronavirus about a month ago. “In the ASC, universal precautions take care of most of what we do, but we still have to account even for rare scenarios that may pose a risk of aerosolized viral transmission. In the clinic, we trained our staff on things like how to use masks, how to disinfect, and how to conduct spacing in the office. During the shutdown we did no surgery and only saw medically necessary visits in the clinic on an on-call basis. Three weeks ago, we started scheduling patients in clinic. Last week we started seeing comprehensive eye exam and surgical consults. This week, we’ll do some YAG and SLT lasers, and next week, we start cataract surgery.”
The ban on elective surgeries ended on April 30 in Tennessee. “In the metro Nashville area, where the mayor’s guidance is primary, we’re limited to patients under age 70; outside the metro Nashville area, we don’t have that restriction,” says Dr. Sternberg, who is the physician lead for Vanderbilt’s COVID-19 Response Command Center. In this role, he develops guidelines and policy for a range of things, including addressing care of patients and workforce; serology testing; testing patients entering the workforce; universal masking policies; visitor policies; exemptions; and the redelegation of responsibilities in case there’s a surge of cases.
Procedures involving aerosolization, a major risk factor in the transmission of SARS-CoV-2, also require testing in his state. “Any patient who needs general anesthesia has to be tested for COVID before we do their procedure,” Dr. Sternberg says. “Other than that, some plastics cases that require sinus manipulation, such as a nasal lachrymal duct procedure or an orbital reconstruction, because of potential exposure to the nasopharyngeal pathway, also require COVID testing prior to the procedure. Those are higher risk procedures. For cataract and retina procedures, we’re not doing COVID testing.
“Right now we’re seeing a leveling off in our positives and a significant leveling off in terms of our inpatients, so we feel very good about flattening the curve,” he continues. “I think we’ve been successful in reaching the Phase I criteria. However, having said that I have great anxiety about what will happen in the next four to six weeks with the relaxation of social distancing and masking. Right now, our modeling suggests we’re going to have a significant uptick in mid-June, when we’ll feel the effects of relaxed restrictions.”
Ohio opened up for medically necessary surgeries on May 1, provided that the procedure uses minimal PPE and doesn’t involve an overnight stay. Rishi Singh, MD, a surgeon at the Cleveland Clinic’s Cole Eye Institute, and assistant professor of ophthalmology at the Lerner College of Medicine in Cleveland, says his practice is offering typical routine eye care alongside all other visits now. “We’re starting cataract surgery again and rescheduling patients who were delayed from before the shutdown. Unfortunately, many patients deferred their eye care despite significant vision issues. Patients with diabetes have lost vision due to vitreous hemorrhage and some with macular degeneration have had significant vision loss. They’re prioritized from a triage standpoint because they have significant disease that needs to be addressed right away.”
In Utah, elective surgeries were given the green light on May 4. Color-coded levels indicate local re-openings. “We went from red to orange, so that means we’re now able to consider doing elective surgeries again and open our practices a bit,” says Nick Mamalis, MD, at the Moran Eye Center of the University of Utah in Salt Lake City. “In addition to the state restrictions and guidance, the university has its own constraints. For example, we’re allowed to do routine cataract surgeries, but only on patients who are under 65. For patients over 65, we have to have a specific indication for routine cataract surgery, such as if it’s their only eye, they’re the driver for someone in the family who can’t drive or they have severe anisometropia. We’re also required to do COVID testing now before a patient can come into the office, and they must be tested within 48 to 72 hours before surgery. Patients must also complete a questionnaire, and they’re screened for fever.
“Right now, we’re slowly reopening our clinics,” Dr. Mamalis continues. “We’re taking fewer people per hour than we would going full blast, but we’re opening up to see more people, so long as there aren’t a lot of people at the same time. Right now, for example, we’re seeing only four patients an hour. In terms of surgeries, we have two rooms open instead of four, and only for certain hours during the day.”
Virginia Eye Consultants began elective surgeries on May 4, when the restrictions were eased. Karen Spencer, CEO of Virginia Eye Consultants, says that they’re offering all of their services, putting safety first. “We’ve done a very slow and careful ramp-up,” she says. “We have 20 providers, four clinic locations and one surgery center, so we’ve had to redesign our schedule templates and use capacity in satellite offices, for instance, to house a provider and patient, versus having them where they’d traditionally be, to accommodate social distancing.”
Spencer says that her region has only been mildly to moderately impacted by COVID-19. “We’re scheduling surgery in the same manner we always have,” she says. “The ASC is probably one of the safest places to be right now. The infection control measures—especially in a single specialty ASC that does only eyes—protects patients in many ways. We aren’t bringing in any sick or questionably sick patients. We’ve been able to ramp up our surgery operations pretty close to 100 percent, because we know we can do so safely.”
Document COVID Screening
Questionnaires, temperature screening, mask-wearing and extensive sanitation are ubiquitous at practices now. The Academy recently announced on May 7 that COVID screening requires proper documentation.3 All screening should be done in adherence to CDC guidelines, which include temperature checks, face masks and advance notice of fevers or COVID-19-related symptoms. More information is available on the CDC website.
The AAO says that patient screening (positive or negative) should be documented in the patient’s medical record, and the practice should develop a written protocol to outline the screening protocol. This demonstrates that the practice is working toward maintaining a safe environment for health-care workers and patients. The AAO notes that the following measures should be included in a screening protocol:
—For non-urgent positive cases, physicians should direct patients to contact their primary care provider; note specific ophthalmic conditions that need attention and schedule appropriate follow-up; and follow up with patients who have not rescheduled their appointments within two to four weeks of the positive encounter.
—For urgent positive cases, physicians should consider which ophthalmic conditions will require treatment despite a positive screening; develop scripts and train staff; encourage staff to ask questions about the protocol if unsure or if patients are anxious about their symptoms; the visit may need to be conducted at a hospital with increased safety measures; patients should contact their primary care provider for non-ophthalmic symptoms; and patients’ progress should be followed to reschedule the ophthalmic appointment for continuity of care.
Back at the Office
Dr. Singh says, “We’re trying to encourage the use of personal protective equipment with patients. They all wear masks in clinic and during the examination procedure. We’re also spreading out the schedule and having care-givers wait in the car.” In Dr. Singh’s clinic, patients are evaluated in a single room to reduce the geography of patient flow. “We’re taking a cautious approach,” he adds. “We know that at any given time, we could see another surge, so we’re trying to implement strategies that might reduce that potential as well as create long-lasting strategies to streamline workflow.”
Contactless check-ins, including pre-filling forms online and payments taken over the phone, are increasingly popular among practices and patients. At Virginia Eye Consultants, patients are sent a scheduling link that allows them to do all of their pre-registration online remotely. “Even if we get half the patients to pre-register in advance, it helps to reduce the number of patients at the front desk. It’s worked out well so far,” says Spencer. Dr. Chang’s practice in California is also taking contactless payments over the phone.
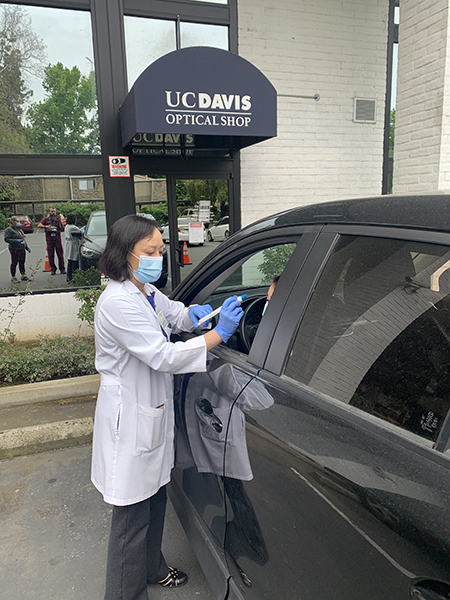
Several practices Review spoke with reported that they’re reducing their patient volume for the time being in an effort to maintain social distancing. Michele C. Lim, MD, professor, vice chair and medical director of ophthalmology at the University of California Davis in Sacramento, says her electronic health record, EPIC, has a built-in COVID risk score that she uses to keep clinic volume at 50 percent. “The COVID risk score is based on a patient’s comorbidity, so the more medical issues you have or the older you are, the higher your morbidity and mortality rate is if you were to be infected with COVID,” she says. “It’s a very easy menu that pops up for each patient on your schedule. We’re using this to triage who to keep on the schedule and who to keep deferring by balancing a person’s COVID risk score with their ophthalmic problem and how urgent or non-urgent that problem is.”
Some practices are also using a combination of telehealth and objective exams to reduce the amount of time patients are in the office. Dr. Lim says her practice has instituted drive-thru-style eye exams and pressure checks with video visit follow-ups. She says, “We check their vision and pressures while they’re sitting in their car, then the patient goes home. The doctor sets up a video visit to talk about their care during the work week. This way, we have some objective data to work with for the video visit.”
In addition to the drive-thru exams, her practice also began doing imaging-only clinics on Saturdays with video follow-ups during the work week to limit patient time in the office. “The imaging clinics decrease the amount of time a patient is physically here in clinic,” Dr. Lim says. “If the imaging were done as an in-person visit, the patient would have to come in, get their imaging—which already creates bottlenecks—then wait for the doctor to be ready to see them. This way, it’s very cut-and-dried. You come in, get your imaging done and go home. Then you do a video visit with your doctor without face-to-face contact. It also helps us keep our schedule templates down to 50 percent.”
The AAO also recommends dividing your staff into teams to reduce the incidence of exposure.4
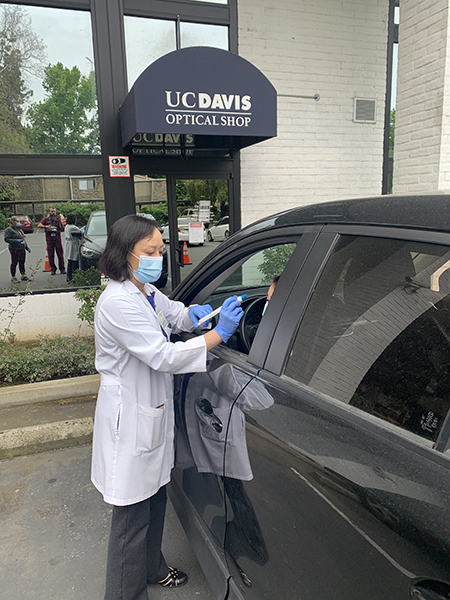 |
| UC-Davis ophthalmologist Michele C. Lim, MD, has instituted “drive-thru” vision and pressure checks at her practice. Patients follow-up later via telemedicine. |
Overcoming Patient Reluctance
Most practices have been making use of social media and electronic communications to let their patients know they’re open and what precautions they’re taking to ensure patient safety. However, there’s still a good number of patients who are reluctant to return to the office or request to reschedule their procedures for a later date. “We’ve had several patients say, ‘No, I want to wait,’ when we contact them about having their surgery done,” says Dr. Mamalis. “That’s reasonable that there’s patient reluctance. Many patients are opting to schedule for July.”
“This is something that’s quite honestly a work in progress,” says Dr. Sternberg. “There’s high variability in terms of patients’ interest and willingness to return for care. Some just feel great and say, ‘Let’s do it’; others say, ‘I’m not ready.’ We’ve found that the person who’s most effective at having that conversation is the doctor her or himself if the doctor will take the time to phone the patient. That’s the most reassuring and most likely way patients will come back for care. But even among the doctors, there’s high variability in terms of their level of comfort. They’re human as well. Some feel very comfortable going back to the OR and the clinic, and there are others who are anxious about it.”
At Virginia Eye Consultants, Spencer says patients receive links to a video by Elizabeth Yeu, MD, and to the 10 critical steps the office has put in place to create a safe environment. Both can also be found on the practice’s website. Dr. Yeu’s video instructs patients on what to expect when they come back to the office, including wearing cloth face coverings, daily employee and patient temperature screenings, the office’s extensive daily disinfection and routine exam room cleansing, limits on visitors, and availability of telehealth. Additionally, the practice’s hold music informs patients of the 10 critical steps.
On the Bright Side
“We’ve become much more efficient in the things we do prior to the patient visit,” says Dr. Mamalis. “Patients can fill in forms online or our technicians call them the day before to pre-fill out everything. Much of what the patient would do when they show up to the clinic is now done on the front end. I think as we do this more and more, a lot of practices will find this improves efficiency and decreases the amount of time the patient is actually in the clinic. Our staff and technicians like this as well, since it allows them to spend more time focusing on the actual patient history and complaints and conducting pre-testing before the doctor comes into the room. In the long-run, I think this will make clinics more efficient, and eventually when we can ramp up the number of patients we’re seeing, it’ll allow us to see even more patients.”
ASCRS “Turning the Lights Back On”
The 2020 ASCRS Virtual Meeting, taking place online May 16 and 17, will feature a two-part symposium on practice reopening, patient care during the pandemic and changes to your business model. Keynote speaker former FDA Commissioner Scott Gottlieb, MD, will share his views on the crisis and the next steps to take. For more information, visit annualmeeting.ascrs.org/programs/ascrs-program/special-sessions.
1. Parke, DW. Returning to ophthalmology practice. AAO. Accessed 11 May 2020. https://www.aao.org/about/governance/academy-blog/post/returning-to-ophthalmology-practice.
2. States begin easing elective procedure restrictions. Last updated May 7, 2020. Accessed 11 May 2020. https://www.aao.org/practice-management/article/states-begin-easing-elective-procedure-restriction.
3. Patient screenings require documentation and planning during COVID-19. May 7, 2020. Accessed 11 May 2020. https://www.aao.org/practice-management/article/patient-screenings-require-documentation-planning.
4. Develop employee teams to limit exposure to coronavirus. May 6, 2020. Accessed 11 May 2020. https://www.aao.org/practice-management/article/develop-employee-teams-to-limit-exposure.