Presentation
A 50-year-old male with no past ocular history presented to the Wills Eye Emergency Room with pain and foreign body sensation in his right eye. The patient works as a firefighter and had a shattered-glass injury to his eye while at work two days prior to presentation. He was found to have several small pieces of glass on his right eyelid and superficial cornea that were removed at the slit lamp. He was treated with Bacitracin/Polymixin ointment and instructed to return to the Wills Eye Cataract and Primary Eye Care clinic in one week. During his follow-up evaluation, the patient noted marked improvement of his symptoms.
Medical History
The patient had a past medical history of hypertension and hypercholesterolemia. His medications included an angiotensin receptor blocker. There was no significant past ocular history. Family history and review of systems were noncontributory.
Examination
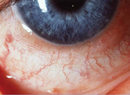
At the time of the patient's follow-up presentation, uncorrected visual acuity was 20/20- in the right eye and 20/25- in the left eye. Pupils were equal, round and reactive to light without an afferent defect. Motility and confrontational visual fields were normal in both eyes. Slit-lamp examination was significant for conjunctival nodules located diffusely within the conjunctiva of both upper and lower lids. Examination of the cornea, anterior chamber and lens were within normal limits. Dilated fundus exam was within normal limits in both eyes. Anterior segment photographs obtained at the present evaluation are shown below (See Figure 1).
Diagnosis, Workup and Treatment
The patient presented with a foreign body in the right eye and was incidentally found to have multiple nodules within the conjunctiva of both eyes. Further history revealed that these lesions were present for approximately one year and were asymptomatic. The differential diagnosis for these clinical findings includes chronic follicular conjunctivitis caused by organisms such as Chlamydia and Moraxella. Granulomatous etiologies such as sarcoid and tuberculosis were entertained, as were infiltrative conditions such as amyloid and lymphoma. Given the need for a tissue diagnosis, the patient was referred to the Cornea clinic for an excisional biopsy of the lesions. Further workup of the specimens by pathology using immunohistochemistry revealed that these tissues contained an infiltration of a predominately B-cell origin (See Figure 2).
Discussion
The patient was found to have a bilateral, lymphoid infiltrate within mucosa-associated tissue of the conjunctiva (MALT). MALT plays a role in regulating mucosal immunity and is therefore present along such mucosal linings as the GI tract, lung and conjunctiva. This tissue is composed of a B and T-lymphocyte aggregate whose function is to prevent the adherence of pathogens to the mucosal epithelium. Proliferation of atypical B-cells within the Marginal Zone of MALT can lead to MALT lymphoma, a low-grade but potentially systemic condition.
The etiology of MALT lymphoma is not certain, but may involve antigenic stimulation by pathogens such as H. pylori and B. burgdorferi. There also may be an autoimmune role, as this condition is found in association with Sjögren's disease and Hashimoto thyroiditis. Clinically, MALT lymphoma of the conjunctiva presents as an elevated, pink and fleshy mass commonly referred to as a "salmon patch." It is typically smooth, but can be multi-nodular and is often found in the fornix and bulbar conjunctiva. The clinical features of this condition make differentiation of benign from malignant disease difficult. An analysis of 117 patients with conjunctival, lymphoid infiltrates showed that unilateral infiltrates carried a 17-percent chance of systemic involvement, whereas patients with bilateral infiltrate had a 47-percent chance of having systemic lymphoma.
Management of conjunctival MALT lymphoma begins with a systemic evaluation to rule out disseminated disease. Small, circumscribed lesions may be treated with excisional biopsy with cryotherapy. Large lesions in the absence of systemic findings are treated with radiation therapy and sometimes chemotherapy. Systemic lesions require chemotherapy and are generally treated with additional rituximab. Ongoing research suggests that local treatment using interferon injections over several weeks can induce clinical resolution of conjunctival lesions. In addition to the aforementioned therapy, some ophthalmologists will treat these patients for H. pylori despite the lack of evidence in the literature suggesting clinical utility.
MALT lymphomas of the conjunctiva are low-grade, indolent tumors that tend to be very responsive to local therapy and radiation. They often undergo spontaneous regression and rarely undergo transformation to diffuse large B-cell lymphoma. As a result, the five-year survival rate is over 90 percent, thus making the prognosis very good for patients with this condition. Proper management of patients with MALT lymphoma requires a high index of suspicion when evaluating the conjunctiva in order to make an accurate and timely diagnosis.
The author would like to thank Ralph Eagle, MD, of the Wills Eye Ocular Pathology Department, Christopher Rapuano, MD, of the Wills Eye Cornea Service, Jerry Shields, MD, and Carol Shields, MD, and Sara Lally, MD, of the Wills Eye Ocular Oncology Service, and Steven Kanoff, MD, of the Wills Eye Cataract and Primary Eye Care Service, for their time and assistance with this case.
1. DomatoBE, et al. Systemic remission of non-Hodgkin's lymphoma after intralesional interferon alpha-2b to bilateral conjunctival lymphomas. Am J Ophthalmol 2004;138:672-3.
2. Isaacson PG, Berger F, Muller-Hermelink HK, Nathwani BN, Piris MA, Swerdlow SH, Harris NL. In: Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma). World Health Organization classification of tumours; Tumours of haematopoietic and lymphoid tissues, Jaffe ES, Harris NL, Stein H, Vardiman JW, editors, Lyon: IARC Press, 2001;157-60.
3. Nola M, et al. Outcome and prognostic factors in ocular adnexal lymphoma. Croat Med J 2004 Jun;45(3):328-32.
4. Shields CL, Shields JA, Carvalho C, et al. Conjunctival lymphoid tumors: Clinical analysis of 117 cases and relationship to systemic lymphoma. Ophthalmology 2001;108:979-984.
5. Shields JA, Shields CL. Eyelid, Conjunctival and Orbital Tumors. An Atlas and Textbook. Second Edition ed.
6. Tsai PS, Colby, KA. Treatment of Conjunctival Lymphomas.Seminars in Ophthalmology, 1744-5205, Volume 20, Issue 4, 2005, Pages 239-246.