A broad differential diagnosis can be generated for unilateral optic disc edema. Common diagnoses can be broadly categorized as traumatic, demyelinating/autoimmune (multiple sclerosis, neuromyelitis optica, lupus erythematosis, thyroid eye disease), infectious conditions (tuberculosis, lyme disease, syphilis, herpetic, bartonella), infiltrative/inflammatory (neoplasm, sarcoidosis, drusen), congestive (asymmetric pseudotumor, orbital pseudotumor/cellulitis) or vascular (diabetic papillopathy, giant cell arteritis, nonarteritic anterior ischemic optic neuropathy).
B-scan ultrasonography revealed no optic disc drusen. Humphrey visual field testing showed peripheral relative and absolute scotomas (See Figure 2).
The patient was sent for MRI. Initial magnetic resonance imaging of the brain demonstrated a left optic nerve with diffusely increased diameter, with a mildly infiltrative appearance of the intraconal and retro-orbital fat without extraocular muscle enlargement. Mild proptosis was also noted. After gadolinium, there was significant enhancement of the left optic nerve as seen above. The remainder of the scan including cavernous sinus and pituitary was unremarkable. (See Figure 3).
Based on her clinical findings, her differential diagnosis was narrowed to optic nerve meningioma, optic nerve drusen, resolving optic neuritis or an optic nerve glioma. Her imaging was thought to be most consistent with an optic nerve sheath meningioma involving the orbital portion without extension into the canal. She was seen again six weeks after initial evaluation and the findings were unchanged. Given the stability of her examination, visual fields, her good vision and lack of color abnormalities, it was recommended that she have no active treatment. She was referred for consultation with neurosurgery, and advised to return if she noticed any change in vision. Serial MRI images have shown stability of the optic nerve meningioma and the patient has remained asymptomatic.
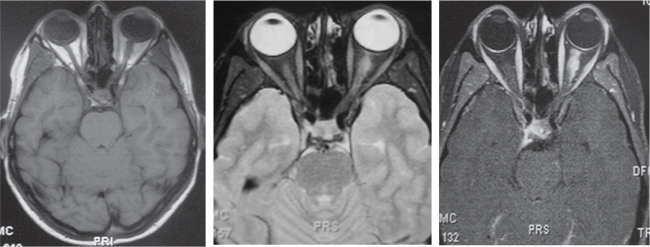 |
| Figure 3. After gadolinium, there was significant enhancement of the left optic nerve. Cavernous sinus and pituitary was unremarkable. |
Discussion
Optic nerve sheath meningiomas are benign neoplasms of the optic nerve sheath.1 In contrast to the intracranial portion of the optic nerve, the intracanalicular and intraorbital optic nerve segments are surrounded by all three layers of meninges (dura, arachnoid and pia mater). The subarachnoid and subdural spaces created by these sheathes are continuous with the brain. The central retinal artery runs along the optic nerve and pierces this dural sheath approximately 1.25 cm behind the globe.
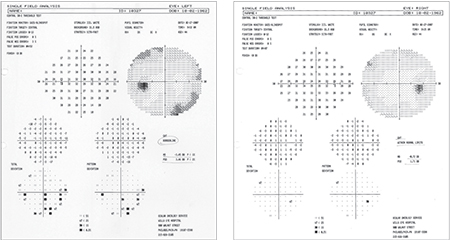 |
| Figure 2. Humphrey visual field testing showed peripheral relative and absolute scotomas. |
The tumor typically tracks along the optic nerve sheath and can grow to surround and compress the optic nerve, central retinal artery or the central retinal vein.3,4 Vision loss is usually caused by a compressive optic neuropathy, but patients may live without symptoms for decades. The mass can also grow back towards the chiasm and cause contralateral field deficits.4
Clinical signs and symptoms include painless monocular vision loss, optic atrophy and opticociliary shunt vessels.3,5 Axial proptosis, optic disc edema, color vision abnormalities and extraocular muscle movement abnormalities may also be noted.5 Unlike many other brain tumors, associated mortality is very low.6
Imaging studies classically show an enlarged optic nerve complex that can either be round or fusiform. There is also often enhancement of the arachnoid and a negative shadow of the optic nerve.3,6,7 Calcification around the optic nerve is also noted in 20 to 50 percent of cases.4
Management depends on symptoms and progression. In asymptomatic patients, observation with exams every six to 12 months including vision, pupils, color vision, visual fields as well as periodic MRI imaging is indicated.1,3,8,9 With quality imaging, biopsy is rarely indicated. Many patients do have progressive visual loss over time, but there are currently no tests available that can predict the aggressiveness of these benign neoplasms. If there is progression of a patient’s symptoms, the optic nerve can be approached with radiotherapy or gamma knife surgery. Historically, surgical removal is rarely indicated, except for very advanced cases with a blind eye. REVIEW
1. Shields JA, Shields CL. Optic nerve sheath meningioma. In Shields JA, Shields CL. Eyelid, Conjunctival and Orbital Tumors. Ed 3. Philadelphia, Wolters Kluwer, 2015:582-588.
2. Yachnis AT, editor. Meningioma. Pathology Outlines. 2015. Available from: http://www.pathologyoutlines.com/topic/cnstumormeningiomageneral.html.
3. Basic and Clinical Science Series. Neuro-Ophthalmology. American Academy of Ophthalmology. 2014-2015.
4. Miller NR. Primary tumours of the optic nerve and its sheath. Eye (Lond) 2004;18:1026-37.
5. Nichols C, Pincus DW, Bhatti MT. Optociliary shunt vessels. Neurology 2005 Apr 26;64(8):1443.
6. Dutton JJ. Optic nerve sheath meningiomas. Neurol Clin 1991;9(1):163-77.
7. Shapey J, Sabin HI, Danesh-Mayer HV, et al. Diagnosis and management of optic nerve sheath meningiomas. J Clin Neuro 2013;20:1045-1056.
8. Singh S, Schiffman JS. Optic Nerve Pathway Gliomas and Optic Nerve Meningiomas. In: Esmaeli B, ed. Ophthalmic Oncology. New York: Springer, 2011:383–393.
9. Turbin RE, Thompson CR, Kennerdell JS, et al. A long-term visual outcome comparison in patients with optic nerve sheath meningioma managed with observation, surgery, radiotherapy, or surgery and radiotherapy. Ophthalmology 2002;109:890-899.



