The patient’s proptosis, hypoglobus and extraocular movement limitations suggested an orbital neoplastic, inflammatory or infectious process. The patient had decreased visual acuity and trace relative afferent pupillary defect, but normal color plates. This could suggest optic nerve involvement, but was more likely a result of mass effect on the globe. The patient underwent a CT scan (See Figure 1), which revealed a lobulated heterogeneous mass arising from the left lacrimal gland 2.6 cm in maximal diameter. The lesion caused mild mass effect on the left globe and extraocular muscles, as well as mild scalloping of the frontal bone.
The patient’s laboratory workup revealed mildly elevated ACE and anti-SSA levels, with normal ANA, ANCAs and anti-SSB. The patient initially underwent X-ray of the chest, which showed opacities in the right upper lobe. Elevated ACE and X-ray findings prompted further investigation into the possibility of sarcoidosis. The patient then underwent CT of the chest, which revealed opacities in the right upper lobe. These findings were consistent with an infectious or inflammatory process. There were no mediastinal or hilar lymphadenopathy or lung parenchymal changes to suggest sarcoidosis.
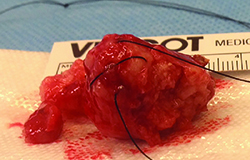
The patient underwent anterior orbitotomy with an excisional biopsy of the left lacrimal gland mass. The pathology report described the mass as a pseudoencapsulated tumor with surface bosselations (See Figure 2). Histopathology revealed a characteristic mix of epithelial ducts and mesenchymal components, and the patient was diagnosed with benign mixed tumor.
Discussion
Pleomorphic adenoma or benign mixed tumor (BMT) is the most common epithelial tumor of the lacrimal gland, comprising 50 percent of cases.1 The main differential diagnostic consideration for BMT is adenoid cystic carcinoma (ACC), which is the most common malignant tumor of the lacrimal gland, accounting for 50 percent of malignant cases.1 BMT usually presents as a slow-growing, painless, round mass that may cause accentuation of the lacrimal gland fossa, but does not cause bone destruction.1-3 On the other hand, ACC classically presents as a rapidly growing painful mass that erodes the bone and infiltrates surrounding structures. ACC’s predilection for perineural invasion is the cause for the severe pain associated with ACC.1-3
|
The suspected preoperative diagnosis is critical in the management of lacrimal gland tumors as it can influence surgical planning. For example, complete excision without biopsy is recommended in the case of pleomorphic adenomas, while an incisional biopsy is recommended for most other lacrimal tumors prior to planning definitive treatment.3 This recommendation is based on the results of Ramon L. Font, MD, and John W. Gamel, MD, who reviewed 136 cases of BMT and found that biopsy prior to excision had adverse influence upon the outcome with five-year recurrence rate of 32 percent, compared to 3 percent in cases that were initially completely removed.4 Recurrence of BMT is particularly concerning because it has been associated with malignant transformation into malignant mixed tumor (MMT).2 Drs. Font and Gamel’s data has been questioned due to its retrospective nature and heterogeneous sources of cases. Another case series of 72 patients in a single center with longer follow-up showed a much lower rate of recurrence with only one case, which occurred in a patient who underwent biopsy prior to excision.5 Some have questioned the absolute “no biopsy” rule in management of lacrimal gland pleomorphic adenoma since fine-needle aspiration biopsy is successfully used for diagnosis of pleomorphic adenomas in other salivary glands.6
The original algorithm for management of an unknown lacrimal gland tumor published in 1979 relied heavily on clinical presentation to determine whether to pursue en bloc excision or incisional biopsy. It was recommended that painless tumors with symptoms for greater than 12 months are likely benign and should undergo complete excision, while painful tumors present for less than 12 months should undergo biopsy. Additionally, X-ray finding of bone destruction steered one toward malignant etiology and incisional biopsy.3
The advent of computer tomography has greatly improved our pre-biopsy diagnostic acumen and changed the original algorithm. In a case series of 63 orbital BMTs, only 69 percent had symptoms for greater than 12 months, 89 percent had no pain and 98 percent had benign imaging characteristics on CT.7 Based on the specificity of CT in identifying benign tumors, the updated algorithm recommended completely excising tumors with benign CT findings, even if they present atypically for BMT with pain and short duration of symptoms.7 The application of the updated algorithm in this case has been shown to be successful. REVIEW
The author would like to thank Jacqueline Carrasco, MD, of Wills Eye Oculoplastic and Orbital Surgery Service, for her time and assistance in preparing this case report.
1. Eagle RC. Eye Pathology. Philadelphia: Wolter Kulver/Lippincott Williams & Wilkins, 2011.
2. von Holstein SL, Coupland SE, Briscoe D, et al. Epithelial tumors of the lacrimal gland: A clinical, histopathological, surgical and oncological survey. Acta Ophthalmol 2013;91:195-206.
3. Wright JE, Steward WB, Krohel GB. Clinical presentation and management of lacrimal gland tumors. Br J Ophthalmol 1979;63(9):600-606.
4. Font RL, Gamel JW. Epithelial tumors of the lacrimal gland: An analysis of 265 cases. In: Jakobiec FA, ed. Ocular and Adnexal Tumors. Birmingham, AL: Aesclulapius Publishers Inc.; 1978:787-805.
5. Currie ZI, Rose GE. Long-term risk of recurrence after intact excision of Pleomorphic Adenomas of the Lacrimal Gland. Arch Ophthalmol 2007;125(12):1643-1646.
6. Lai T, Prabhakaran VC, Malhortra R, Selva D. Pleomorphic adenoma of the lacrimal gland: Is there a role for biopsy? Eye 2009;23:2-6.
7.Rose GE, Wright JE. Pleomorphic adenoma of the lacrimal gland. Br J Ophthalmol 1992;76,395-400.