Many surgeons say the adjunctive use of mitomycin-C in PRK cases has helped them avoid haze and regression postop. However, over the years, some studies have called mitomycin's use into question, though PRK surgeons believe their protocols are such that mitomycin's negative effects won't become a problem. Here's a look at some of the current research on MMC's possible effects and what refractive surgeons think about its safety profile.
Possible Complications
In addition to its use in glaucoma surgery, MMC has also been applied to patients' eyes by corneal specialists after pterygium surgery. In one study of complications in that setting, surgeons reported on 10 patients who had serious, vision-threatening complications associated with MMC.1 Complications included: severe secondary glaucoma (four patients); corneal edema (three patients); corneal perforation (one patient); corectopia (two patients); iritis (eight patients); sudden-onset mature cataract (two patients); scleral calcification (one patient); and severe photophobia and pain (eight patients).
The upshot of the study, the researchers said, is to use the lowest possible concentration of MMC for the shortest time period.
Another study of possible complications used 0.02% MMC in goat eyes and found that it resulted in MMC in the corneal endothelium at a level of 0.37 µg/ml and produced a significant increase in corneal endothelial DNA cross-linking with as little as six seconds of application.2 In addition to this cross-linking, the researchers say that they found that exposure to MMC at times and concentrations commonly used in refractive surgery produced persistent DNA damage and endothelial death by apoptosis. They're concerned that MMC use during refractive surgery may increase the potential for long-term deleterious effects on the corneal endothelium.
Another study was undertaken in refractive surgery patients. In it, 18 PRK patients had one eye randomly assigned to a 30-second 0.02% MMC treatment with the fellow receiving balanced salt solution. There was no significant difference in preoperative endothelial cell counts between the two groups, with the MMC group averaging 2,835 ±395 and the control averaging 2,779 ±492. At one and three months postop there was no statistically significant difference in the cell count in the control group compared to preop (one month: p=0.27; three months: p=0.14). However, the endothelial cell loss was statistically significant in the MMC group; at one month there was a 14.7 ±5.1 percent loss (p=0.0006) and at three months the loss was 18.2 ±9 percent (p=0.002).3
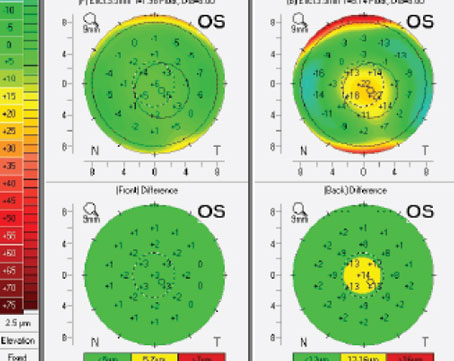
The most recent study of prophylactic MMC in PRK was released this summer in the Journal of Cataract and Refractive Surgery.4 In a nonrandomized controlled trial, surgeons divided 81 PRK patients (162 eyes) into three groups: bilateral MMC treatment; unilateral treatment and no MMC. The patients had low to moderate myopia and corneas that were thick enough to undergo ablation. Seventy-six eyes were ultimately treated with MMC.
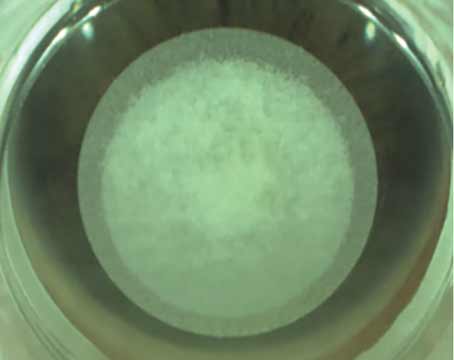
The MMC protocol consisted of a cellulose sponge pledget soaked with MMC 0.02% being placed on eyes with ablation depths of 75 µm or deeper. The duration of contact ranged from 10 to 50 seconds, with deeper ablations receiving a longer contact time.
Postop, treated eyes and untreated eyes were similar in terms of acuity and refraction. However, the MMC-treated eyes lost an average of 14.8 percent of their endothelial cell density six months postop, compared to a loss of 5.1 percent in the untreated eyes (p<0.001). Longer MMC contact time and male sex were associated with greater loss.
Surgeons Respond
Roy Rubinfeld, MD, associate professor at 
Chicago
Long Beach
In terms of other studies of endothelial cell loss and MMC, Dr. Ep-stein and his associates published a study last year in which 16 eyes with a planned ablation depth greater than 75 µm underwent PRK followed by 0.02% MMC application for 12 seconds.5 He and his co-workers examined the endothelial cells preop and at least a year postop with specular microscopy. They didn't find any significant differences in cell density or the percentage of hexagonal cells present.
Edoardo Midena
Many refractive surgeons think MMC is effective for the prevention of corneal haze, but are quick to add that the risks shouldn't be underestimated. Says Dr. Epstein, "In my view, mitomycin-C still needs to be used very judiciously."
1. Rubinfeld RS, Pfister RR, Stein RM, Foster CS, Martin NF, Stoleru S, Talley AR, Speaker MG. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology 1992;99:11:1647-54.
2. Roh DS, Cook AL, Rhee SS, Joshi A, et al. DNA Cross-linking, Double-strand Breaks and Apoptosis in Corneal Endothelial Cells After a Single Exposure to Mitomycin-C. Invest Ophthalmol Vis Sci 2008 Jul 24 [Epub ahead of print].
3. Morales AJ, Zadok D, Mora-Retana R, Martinez-Gama E, Robledo NE, Chayet AS. Intraoperative mitomycin and corneal endothelium after photorefractive keratectomy. Am J Ophthalmol 2006;142:3:400-4.
4. Nassiri N, Farahangiz S, Rahnavardi M, Rahmani L, Nassiri N. Corneal endothelial cell injury induced by mitomycin-C in photorefractive keratectomy: Nonrandomized controlled trial. J Cataract Refract Surg 2008 Jun;34:6:902-8.
5. Goldsberry DH, Epstein RJ, Majmudar PA, Epstein RH, et al. Effect of mitomycin C on the corneal endothelium when used for corneal subepithelial haze prophylaxis following PRK.
J Refract Surg 2007;23:7:724-7.
6. Gambato C, Ghirlando A, Moretto E, et al. Mitomycin C modulation of corneal wound healing after photorefractive keratectomy in highly myopic eyes. Ophthalmology 2005;112:2:208-18.
7. Midena E, Gambato C, Miotto S, Cortese M, et al. Long-term effects on corneal keratocytes of mitomycin C during photorefractive keratectomy: A randomized contralateral eye confocal microscopy study. J Refract Surg. 2007;23:9:S1011.