Ophthalmologists continue to face challenges when dealing with complicated anterior-segment pathologies, similar to the unsolved diseases of the posterior segment we discussed last month. At that time, we discussed interdisciplinary approaches to treating retinal disease, through collaboration with other disease specialists and by making use of technologies like the latest drug delivery systems. Here, we'll focus on the external eye, including conditions such as neurotrophic keratitis and peripheral corneal ulcers. We'll also explore evolving methods for treating corneal damage, such as amniotic membrane grafts. As with the retina, we can maximize the effectiveness of our treatment of corneal pathology by collaborating with other disciplines of medicine.
Corneal Ulceration
A disruption to the corneal surface triggers healing and remodeling processes that can create an environment prone to ulceration. Corneal ulcers can result from infection, post-surgical trauma, contact lens wear and other toxic stimuli. Here are two approaches to treating ulcers.
• Nerve growth factor treatment. Numerous studies have indicated that molecules such as cytokines, growth factors and neuropeptides play roles in corneal recovery after injury. However, an approach to effectively regulate the healing process has not yet been characterized.
Nerve growth factor (NGF) is an endogenous protein necessary for survival, growth and differentiation of peripheral sympathetic and sensory neurons. It also restores the function of injured neurons. Several studies have identified the role of NGF in the pathophysiology of neuropathies of the posterior segment as well as neuropathies of the central and peripheral nervous system. More recent research has recognized NGF as a key regulator in accelerating the healing process of corneal and skin ulcers.
Experimental corneal epithelial injuries were shown to increase levels of NGF in the rat cornea, and inhibiting endogenous NGF delayed corneal epithelial healing. Additional research shows that the application of exogenous NGF to rat eyes with corneal lesions significantly increased the healing rate, which confirms the involvement of NGF in corneal recovery.1
In clinical trials, the treatment potential of NGF has been investigated in patients with neurotrophic keratitis, a disease that involves injury to the trigeminal nerve leading to decreased corneal sensitivity, blinking and, ultimately, corneal degeneration. Neurotrophic keratitis can be caused by a number of ocular or systemic diseases, including fifth-nerve palsy, viral infections, chemical burns, corneal surgery, diabetes and multiple sclerosis. One study found that topical application of NGF effectively healed corneal ulcers caused by neurotrophic keratitis within one month and prevented further degeneration after discontinuation of treatment. The researchers in the study reported no major side effects.2
Subsequent to the observation that topical NGF promoted healing of human corneal ulcers, the same group of researchers investigated the effects of NGF on immune and/or autoimmune cutaneous ulcers. The research investigated the effects of NGF on skin ulcers caused by rheumatoid arthritis, systemic vasculitis and diabetes, as well as cutaneous pressure ulcers in the elderly and skin ulcers of animals. All cases were unresponsive to conventional topical and systemic treatments. They found that topical administration of highly purified murine NGF to the skin ulcers led to complete healing within four to 12 weeks of daily treatment depending on the size and depth of the lesion,3 further revealing the broad applicability of this area of research.
NGF has also been investigated for its anti-inflammatory function, which has been shown to be 10 times more active than dexamethasone and 1,000 times more active than NSAIDs in murine models.4 Research has begun to investigate NGF in treating severe corneal melts resulting from immune-related peripheral corneal ulcers, for which there is no existing therapy.
One study found that, after NGF treatment, patients' immune corneal ulcers were healed within eight weeks without relapse in a follow-up period of three to 12 months.5 The only side effects were transient ocular pain and photophobia. The researchers hypothesized that NGF accelerated corneal healing while also regulating the function of inflammatory cells on the ocular surface.
These studies indicate that NGF plays a key role in the healing process of corneal and skin ulcers. However, we don't completely understand the mechanism by which NGF functions. Further collaborative research among ulcerative disease specialists may lead to established therapeutic applications of NGF.
One minor but frequent side effect of NGF treatment for neurotrophic keratitis was increased tear production, probably resulting from the increase in corneal sensitivity. Neurotrophic keratitis has been associated with a decrease in aqueous tear production as well as reduced cutaneous and nasal mucosal sensation. The decreased corneal sensitivity and, in turn, blink rate, and the clinical signs and symptoms found with this disease are actually similar to those seen in post-LASIK patients with dry eye. Agents that impact these conditions by affecting blink rate, compensatory mechanisms and tear-film production may also have potential for the dry-eye disease itself.
• Amniotic membrane grafts. Another new area of research for the improvement of ocular surface conditions involves the use of amniotic membrane (AM) grafts for healing corneal ulcers.
Treating infectious scleritis, often caused by previous ocular surgery, has long been a challenge. Systemic antibiotics or steroids, early surgical intervention and cryotherapy have proven to be effective treatment methods for certain cases. However, despite these measures, visual acuity is commonly decreased by complications like cataracts, glaucoma, retinal detachment or endophthalmitis. Surgeons have used corneoscleral graft implants, especially in cases of scleral perforation, but recurrent infection often results. Some hypothesize that the difficulties in treating scleral ulcers stem from the disorganization and inflammation within the cornea that prevent proper epithelial regrowth and migration. One solution to this problem is the amniotic membrane graft transplant.
Surgeons first used preserved human AM grafts to promote growth and differentiation of conjunctival epithelial cells and inhibit scars. Research has also shown that these grafts have anti-inflammatory and anti-microbial activity. Recent studies have found that the application of AM graft promotes reepithelialization, reduces stromal melting and prevents perforation in recalcitrant infectious scleral and corneoscleral ulcers.6,7 Other studies have indicated that AM has a wound-healing effect in sterile corneal ulcers associated with persistent epithelial defects, autoimmune disease, acute burns and herpetic function.
Continuing research in this area may lead to successful therapies not only for ocular surface wounds, but also for systemic wounds from burns or ulcers. Collaboration with stem cell researchers from other fields will help improve tissue-engineering techniques to promote epithelial cell differentiation. Researchers are beginning to explore the possibilities of growing artificial corneas built around a scaffold of plastic and protein that can regenerate corneal cells within weeks. They're now focusing on developing transplant materials that can grow nerve connections and act as tissue substitutes. Such advances would have applicability in tissue engineering and regenerative medicine.
The problem of infection is common to all branches of medicine. In addition, bacterial resistance, regardless of cause, is a constantly looming threat, and all medical practitioners can benefit from the development of novel antibiotics. Viral infection presents similar challenges in terms of prevention, vaccine development and treatment in many different therapeutic specialties. Here are the latest approaches for treating infections.
• Trachoma and vaccine research. In ophthalmology, there are three general categories of Chlamydial infection from this parasitic intracellular bacterium: adult inclusion conjunctivitis (AIC), neonatal inclusion conjunctivitis (NIC) and trachoma.
AIC is a sexually transmitted disease causing urethritis in men and cervicitis in women, as well as ocular manifestations. NIC is transferred from mother to child during passage through the birth canal. While these types of infection are more prevalent in economically developed countries, trachoma, the third type of C. trachomatis syndrome, is rare in these regions. However it's endemic to many undeveloped countries.
Treatment of this type of Chlamydia infection is challenging. The primary means of treatment, represented by the acronym SAFE (Surgery, Antibiotics, Facial hygiene and Environmental improvement), is challenging to enact for a variety of reasons. Many regions in which trachoma is most common are also areas of social or political unrest, and governments lack resources to use for health problems. Additional obstacles are access to and use of water for proper hygiene, reluctance of patients to undergo surgery and the relatively high need for retreatment.8,9
Although efforts to treat trachoma can be effective, they involve much time and many resources—monetary, medicinal, educational and socioeconomic—that are often not available in affected regions. Turning research efforts toward prevention may be a much more efficient approach.
Researchers are investigating development of a vaccine to the Chlamydia genus. Some genes and proteins are conserved among Chlamydia species, which works to the advantage of vaccine development, because one vaccine may confer protection from all C. trachomatis infections, even though the different types of infection are caused only by certain immunotypes.
Genital and respiratory manifestations of infection such as pelvic inflammatory disease, ectopic pregnancy, bronchopulmonary pneumonia and tubal factor infertility can occur in the different syndromes. All of these areas could benefit greatly from the development of a vaccine. Scientists select vaccine candidates based on their knowledge of Chlamydial genomics and proteomics. Another hurdle is the development of delivery systems, which may be viral vectors or bacterial delivery systems that may even have the ability to specifically target the intended mucosal sites.10,11
• New materials/technologies. One area in which interdisciplinary cooperation should continue to flourish is that of contact lens and keratoprostheses development. Keratoprostheses in particular present an amazing challenge: replicating the properties of the human cornea.
For patients who have rejected allograft attempts, a keratoprosthesis is often the only remaining option. Researchers are bent on developing a safe, effective keratoprosthesis, in light of the improvement in quality of life it could provide. Success in this endeavor relies upon collaboration among the ophthalmic community, materials scientists, engineers and chemists who develop novel polymers and compounds to fit specific needs, and the talented machinists who actually create the finely detailed devices.
An artificial cornea, in addition to meeting the standards of the natural cornea, also faces the additional obstacles of extrusion and the potential for elevating IOP. The recipient's peripheral keratocytes must adhere to and anchor the implant, though a membrane cannot be allowed to form over the entire prosthesis.
In the 19th century, the original keratoprostheses were made of glass. Today, several of the newest options in keratoprosthesis materials represent the best the collaboration of medical and material science disciplines has to offer. Prime examples of this collaboration are the AlphaCor (manufactured by Argus Biomedical Pty. Ltd., marketed by CooperVision Surgical Inc.) and the Dohlman-Doane Keratoprosthesis (Massachusetts Eye and Ear Infirmary, Boston).
The AlphaCor is composed of poly-2-hydroxyethyl methacrylate (PHEMA), though in two forms: The first is a 1-mm ring or skirt around the outer edge made out of an opaque, sponge-like PHEMA material. This area has a relatively high water content that facilitates biointegration of the device with the host stromal fibroblasts. Second, the central region of the prosthesis is composed of a clear, gel form of PHEMA. The zone between these two regions is called the interpenetrating polymer network, and it's purported to prevent host cells from forming a retroprosthetic membrane over the transparent part of the device.
The Dohlman-Doane keratoprosthesis, of which there are two types, takes a different approach. Type 1 is used in individuals with adequate tear production and is made of two pieces in a configuration known as a twin-plate collarbutton design. Type 2, designed for use in end-stage dry eyes, has an additional anterior cylinder that protrudes through a closed eyelid. Both are made of poly-methyl methacrylate (PMMA), a polymer commonly used in intraocular lenses. The actual manufacture of these devices involves expert, extremely precise machining with lathes, forming tools and polishing machines.12
|
|
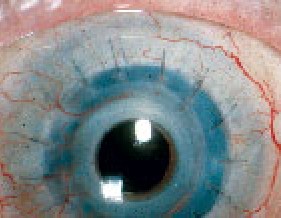
| The Dohlman-Doane keratoprosthesis performs well in standard graft-failure eyes, including those with herpes and chemical burns. Here is one in a herpetic eye two years postop. |
Though the field of keratoprostheses has been riddled with complications, it's clear that researchers are making progress. Continued collaboration among those with expertise in synthetic materials, physicians with clinical experience, and designers with high levels of machining and manufacturing expertise will continue to perfect keratoprostheses. These collaborations will also benefit other areas of ophthalmic practice that use specialized materials and chemical coatings, such as contact lenses, IOLs and sutures, as well as systems using polymers for drug delivery.
As this and the previous Therapeutic Topics column have shown, there are numerous ways in which collaboration among specialists in various medical fields can increase our knowledge of different disease pathologies. This is especially true in broad areas such as inflammation, infection and wound healing.
Whether it's aimed at pathology of the anterior or posterior segment, interdisciplinary medicine will certainly benefit ophthalmology through its continuing efforts.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Fink is manager of medical communications, and Ms. Plumer is a research associate, at Ophthalmic Research Associates in North Andover.
1. Lambiase A, Manni L, Rama P, Bonini S. Clinical application of nerve growth factor on human corneal ulcer. Arch Ital de Biol 2003;141:141-148.
2. Bonini S, Lambiase A, Rama P, et al. Topical treatment with nerve growth factor for neurotrophic keratitis. Ophthalmol 2000;107:1347-1351.
3. Aloe L. Nerve growth factor, human skin ulcers and vascularization. Our experience. Prog Brain Res 2004;146:515-522.
4. Amico-Roxas M, Caruso A, Leone MG, et al. Nerve growth factor inhibits some acute experimental inflammations. Arch Int Pharmacodyn Ther 1989;299:269-285.
5. Lambiase A, Bonini S, Aloe L, Rama P. Anti-inflammatory and healing properties of nerve growth factor in immune corneal ulcers with stromal melting. Arch Ophthalmol 2000;118:1446-1449
6. Ma DH, Wang SF, Su WY, Tsai RJ. Amniotic membrane graft for the management of scleral melting and corneal perforation in recalcitrant infectious scleral and corneoscleral ulcers. Cornea 2002;21:3:275-283.
7. Rodriguez-Ares MT, Tourino R, Lopez-Valladares MJ, Gude F. Multilayer amniotic membrane transplantation in the treatment of corneal perforation. Cornea 2004;23:6:577-83.
8. Kasi PM, Gilani AI, Ahmad K, Janjua NZ. Blinding trachoma: A disease of poverty. PLoS Medicine 2004;1:2:105-108.
9. Adamis AP, Baum TD, Schein OD. Chlamydia and acanthamoeba infections of the eye, Ch 70. In: Albert DM, Jacobiec FA, eds. Principles and Practice of Ophthalmology. Philadelphia: W.B. Saunders Co., 2000: 915-925.
10. Igietseme JU, Eko FO, He Q, Bandea C, Black CM. Developing effective delivery systems for Chlamydia vaccines. Curr Opin Mol Ther 2004;6:2:182-94.
11. Igietseme JU, Eko FO, Black CM. Contemporary approaches to designing and evaluating vaccines against Chlamydia. Expert Rev Vaccines 2003;2:1:129.
12. Doane MG, Dohlman CH, Bearse G. Fabrication of a keratoprosthesis. Cornea 1996;15:2:179-184.