Deciding Factors
Though corneal specialists usually see ulcers when they’re at advanced stages, rather than just suspicious specks, they can shed light on what the comprehensive ophthalmologist should watch for in the patient history and exam in order to root out the cause of the patient’s complaint.
• History. “The first-, second-, third- and fourth-most important question to ask is: ‘Are you a contact lens wearer?’ ” says Sadeer Hannush, MD, attending surgeon at the cornea service at Wills Eye Hospital and medical director of the Lions Eye Bank of Delaware Valley. “Contact lens wear is the most common cause of infectious keratitis. If the patient says, ‘Yes,’ you can then try to identify a breach in contact lens-care protocol by asking questions such as, ‘Do you sleep in them? Are you cleaning them correctly? Do you swim in them?’ ”
Christopher Rapuano, MD, director of Wills Eye Hospital’s cornea
 |
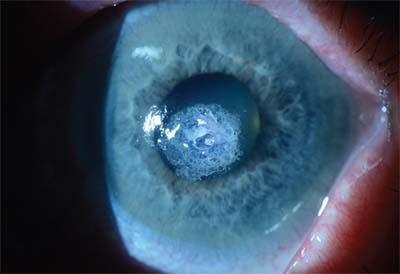
| A large central Scedosporium fungal corneal ulcer with a small hypopyon. Note the irregular edges of the infiltrate. |
If the patient isn’t a contact lens wearer, there are other avenues to explore in the history. “In that case, look for other causes, such as trauma from a child’s fingernail, a mascara brush or working under a car,” Dr. Hannush notes. Physicians also note that a particular kind of injury can lead to a certain type of organism getting into the cornea. An injury from a plant or an animal, or from something that caused a foreign body from the ground to be thrown into the patient’s eye are often behind fungal infections, and exposure to fresh water is a risk factor for Acanthamoeba. Also, ask about prior surgery, as both cataract and refractive procedures are predisposing factors to corneal infections.
Another important part of the history, at least from a corneal specialist’s perspective, is whether the patient has already been treated with something for the condition. “Some patients are on antibiotics—sometimes fortified antibiotics—antifungals, anti-ameobic medications or antivirals,” says Dr. Rapuano. “Some patients come in on all of them! Their referring doctor threw the whole pharmacy at them, hoping something would work.” Dr. Rapuano adds that he also focuses on when the symptoms started. “If the symptoms started a day ago, that gives me a different differential diagnosis than if it was a week or a month ago,” he says.
• Exam. Bennie H. Jeng, MD, chair of the Department of Ophthalmology and Visual Science at the University of Maryland School of Medicine, says it’s important to initially confirm that you are indeed dealing with an infection. “First, when examining the patient, determine if it looks infectious or not,” Dr. Jeng says. “Sometimes a sterile infiltrate might look like an infection when in fact it’s just inflammation in the cornea. An ophthalmologist might see contact-lens-related sterile infiltrates that appear in the periphery due to such things as contact lens overwear and hypoxia. The challenge, then, is to understand the risk factors well enough, and be comfortable enough with the clinical appearance, to know when an infiltrate is probably inflammatory, and to treat it with steroids, not just antibiotics.”
The level of visual acuity is important, as well. “If it’s 20/20 and the patient has a little peripheral ulcer, I’m not as concerned as I would be if it’s hand-motions with a large central ulcer,” Dr. Rapuano says. “How do the lids look? Do the lids have ulcers on them? Did the patient have shingles
 |
| A small, deep corneal ulcer that has caused a central corneal perforation. The striae radiating from the ulcer indicate deep involvement or even perforation. |
Dr. Hannush says if the ulcer is vision-threatening, the general ophthalmologist will almost always refer the patient “because the standard of care for a vision-threatening ulcer is culturing, and most general ophthalmologists aren’t equipped to culture.”
“The next question is what’s the etiology,” says Dr. Jeng, who notes that some presentations can be deceptive. “We often see recurrent herpes simplex virus keratitis manifest in the stroma as an immune process, and it’s actually treated with steroids. However, let’s say we don’t think it’s viral, but it’s more like a classic bacteria or fungus. There are certain characteristics that can point us in one direction or another. For instance, textbooks will tell you that a feathery infiltrate with satellite lesions and a plaque on the endothelium is fungus, and in a lot of cases it is. However, it can be bacterial.
“The patient’s condition is also a clue,” he notes. “For example, say someone who is on chronic topical antibiotics and steroids develops an infection: This eye is in a local immunocompromised state, and the infection could be fungal. The environment where you practice is also a factor. For instance, in the Northeast U.S. or northern California, it’s unusual for us to encounter a fungus, and often there’s some specific reason for it when we do, such as a patient on chronic steroids or who is immunocompromised in some way. In those cases we’d think more along the lines of Candida or a yeast infection. If you’re in Miami, however, where it’s hot and humid, ophthalmologists see more fungus, so they have to have a higher suspicion for it, and the fungus is usually not the indolent yeast but rather the more aggressive filamentous variety.”
Dr. Rapuano says Acanthamoeba can cause specific findings if you know what to look for. “On the history, patients often say that it’s been going on for weeks,” he says. “They may have
 |
| Cyanoacrylate tissue glue was used to treat the perforated ulcer in the previous image, after which a bandage soft contact lens was placed. Small air bubbles can be seen under the contact lens. |
• Culturing and management. Corneal specialists say the next decision, for them, would be whether to culture the organism, and for the comprehensive ophthalmologist, whether to refer the patient for culturing. Dr. Rapuano explains how he approaches the issue. “Things that push me to culture: the more central it is; the bigger it is; the more ulcerated it is—all these things make it worse and more likely for me to culture it,” he explains. “Also, I’ll culture it if there’s an unusual history that would make me suspect fungus or Acanthamoeba. In terms of ulcer size, if it’s under about 2 mm in diameter, I tend not to culture. If it’s larger than that, I tend to culture. This is a guideline, though, and not absolute.”
Dr. Hannush acknowledges that the general ophthalmologist usually isn’t set up to culture, and will usually start the patient on a broad-spectrum antibiotic. “Most use a fourth-generation fluoroquinolone,” he says, “or a very good wide-spectrum drug, Polytrim, which is trimethoprim and polymixin. Trimethoprim is a very good gram- positive-coverage drug, especially for MRSA. Polymixin is a decent gram negative drug, but not great. Moxifloxacin used to be the most popular because it had good gram positive and negative coverage. Gatifloxacin probably has a little bit better pseudomonas coverage. Obviously, if you’re concerned about a contact lens-related ulcer, then pseudomonas is number one on your list until proven otherwise. For pseudomonas, if you’re not giving fortified antibiotics, consider gatifloxacin, ciprofloxacin and tobramycin.”
Dr. Hannush says the corneal specialist will also follow this course for patients with no topical antibiotics already on board and for whom the ulcer isn’t vision-threatening. If there’s significant anterior chamber reaction, hypopyon or an ulcer close to the visual axis, he says corneal specialists will scrape, culture and start the patient on fortified antibiotics. “Fortified antibiotics are usually tobramycin 14 mg/cc and either cefazoline 15 mg/cc or vancomycin 25 mg/cc,” he notes. “All three of these products need to be prepared by a compounding pharmacist.”
Treatment protocols can vary. “I’ll prescribe the drugs for use every half hour while awake and every two hours throughout the night,” says Dr. Hannush. “I never do every hour during the night because it makes patients totally exhausted. I also try to separate the drops’ timing so they don’t wash each other out.” Dr. Hannush then sees the patient after one or two days. “The first sign of recovery is a decrease in pain,” he explains. “This can occur even when the ulcer doesn’t look any better. After that, the next sign is re-epithelialization and resolution of the hypopyon. The hypopyon first gets organized—meaning it’s not liquid anymore. You don’t see a level to it, but instead it just looks like a mass in the inferior angle. Eventually, the corneal infiltrate starts dissolving.”
If cultures were done, sub-specialists say they’ll adjust the medications based on the culture results for maximum efficacy. “If it proves to be fungal, we’ll shift medications significantly,” says Dr. Rapuano. “They get natamycin if it’s fusarium, though a lot of pharmacies don’t carry it so it’s not always easy to find. If it’s Candida, you usually can put them on a compounded amphotericin drop. If the specimens at the pathology lab test positive for Acanthamoeba, or I have a high suspicion for Acanthamoeba, I’ll start them on Brolene and Baquacil, specially compounded.”
Corneal specialists also note that steroids may play a role in the treatment of some ulcers, though they have to be used carefully. “After a few days, if the infection’s under control, we know what we’re treating and the patient’s on the appropriate antibiotics, you can think about starting some steroid drops,” he says. “Steroids are a double-edged sword, though, in patients with infections. We don’t use them early for Acanthamoeba or fungus. In bacterial infections, however, some can respond nicely if there’s a lot of inflammation, since it can improve with judicious use of steroids. Patients on steroids have to be followed very closely, and you have to stop the steroids if it looks like they’re making things worse. When to start the steroids, if you use them at all, depends on the patient. It can be two or three days to a week after treating the infection. For this application, we’ll often use Lotemax or Pred Forte t.i.d. or q.i.d and see how they do.”
Over the next one to three weeks, Dr. Rapuano will slowly decrease the medications and add a nighttime ointment to replace the drops administered throughout the night. “We’ll start a nighttime ointment such as gentamycin, ciprofloxacin, polysporin or the like and then slowly decrease the meds during the day,” he says. “We’ll stop the steroid drop, too, once the inflammation is improved, and go from there.”
Tough Cases
In some cases, organisms prove hard to kill or wounds don’t heal. Here’s how to respond.
• Switch drugs. Dr. Hannush says that, in some cases, the organism may be different than you first expected. “If, for example, the patient’s on fortified tobramycin/vancomycin and there’s no response, you have to re-scrape and culture,” he says. “I just had a case like this. I rescraped and suspected a fungal ulcer, so I empirically started the patient on topical voriconazole 1% and he started getting better.”
• Emergency transplants. “If they’re not getting any better, you can reculture,” says Dr. Rapuano. “Or you might determine that it’s just too deep and isn’t showing up on culture, so you can do a biopsy: go down one-third to one-half corneal thickness with a punch and send half to pathology and half to the culture lab.
“If they’re perforated,” Dr. Rapuano continues, “and it looks like it’s just a small perforation in the cornea, you can use some glue to seal the perforation if you think the infection’s getting better. Often, though, you have to do an emergency—or ‘hot’—transplant.” He says these transplants can be small if the perforation is small and in the periphery, but often they need to be big since they’re often used for large central ulcers. It’s also better not to wait too long to do it, since the ulcer grows over time. “These transplants have a pretty good success rate for resolving the infection, but they often get cloudy and need to be repeated six to 12 months later,” he says.
• Non-healing wound. Dr. Rapuano says that, in some rare instances, he’s able to kill the organism in the cornea but the infection did so much damage to the tissue that the surface is having a difficult time healing. “When we’ve treated the infection and it looks like it’s getting better, but the corneal scratch isn’t healing well, we’ll use amniotic membrane,” he says. Options for this include cryopreserved membrane such as ProKera and dehydrated membrane such as AmbioDisk, OculoMatrix, BioDOptix or Aril. “Using the membrane is pretty straightforward,” Dr. Rapuano says. “There’s not a large learning curve. Some physicians glue them on, some suture them, and some use several layers.” REVIEW
Dr. Rapuano has consulted for Allergan, Bausch + Lomb and Bio-Tissue. Drs. Hannush and Jeng have no financial interest in any products discussed in the article.



