
Presentation
A 28-year-old Caucasian male presented to the Wills Eye Emergency Room complaining of a right droopy lid, facial numbness and binocular horizontal diplopia after sustaining a motorcycle crash one week prior to presentation. He was previously admitted at an outside hospital for loss of consciousness and diagnosed with a right inferior orbital wall fracture.
Medical History
The patient's medical history was significant for depression, for which he used Wellbutrin. His social history was negative for tobacco, alcohol or illicit drug use. Family history was noncontributory. Review of systems was negative.
Examination
Initial ophthalmic examination revealed a best corrected visual acuity of 20/30 in the right eye and 20/20 in the left. Pupil exam was brisk with no afferent pupillary defect. Visual fields were full to confrontation in both eyes. Extraocular motility revealed a frozen globe on the right with full motility on the left. Intraocular pressures were 15 mmHg in the right eye and 14 mmHg in the left eye. Color-plate testing was full in both eyes. Hertel exophthalmometry measured 20 mm on the right and 21 mm on the left. External examination demonstrated a right upper lid ptosis. Levator function was measured to be 9 mm on the right and 18 mm on the left. The margin-reflex distance (MRD-1) was -2 mm on the right and 5 mm on the left. A step-off deformity was appreciated on palpation of the right inferior orbital rim. The patient had facial hypesthesia consistent with a V1 and V2 distribution on the right side. Slit lamp examination was within normal limits. His dilated fundus exam was within normal limits in both eyes.
Based on the history and examination, a non-contrast orbital CT was obtained (Figures 1, 2 and 3). Figure 1 (left). Axial non-contrast CT.
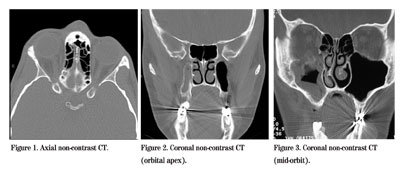
Figure 2 (center). Coronal non-contrast CT (orbital apex).
Figure 3 (right). Coronal non-contrast CT (mid-orbit).
Diagnosis, Workup and Treatment
The CT scan shows a comminuted fracture of the anterior and posterolateral walls of the right maxillary sinus with associated subperiosteal hemorrhage. There is a fracture across the lateral and medial pterygoid plates and the greater wing of the sphenoid, extending into the foramen rotundum. There is a 1- to 2-mm bone fragment at the orbital apex and a fracture of the lateral orbit with a small bone fragment at the posterolateral wall, near the right apex. MRI of the brain and orbits revealed a small amount of subdural blood along the greater wing of the sphenoid in the right middle cranial fossa not evident on CT scan.
The patient was diagnosed with traumatic superior orbital fissure syndrome based on the findings of ophthalmoplegia, ptosis and distribution of hypesthesia. These clinical findings are the result of the traumatic involvement of cranial nerves III, IV and VI, and sensory disturbance of the ophthalmic division of CN V. The insult to V2 was presumed to be secondary to the fracture of the foramen rotundum and inferior orbital wall. The patient was discharged on a medrol dose pack to decrease inflammation and oral antibiotics for infectious prophylaxis. He was followed closely by oculoplastics and continued to improve without surgical intervention.
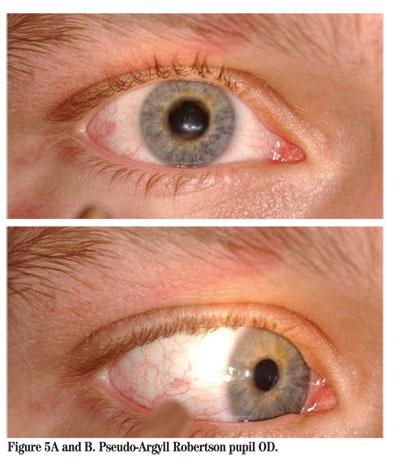
Five weeks later the patient was seen for follow-up and was found to be much improved without diplopia in primary or downgaze. A Goldmann binocular single visual field revealed single vision 30 degrees in all fields of gaze. Interestingly, the patient developed aberrant regeneration of cranial nerve III revealing lid retraction (Pseudo-Von Graefe's sign) and pupillary constriction (Pseudo-Argyll Robertson Pupil) when the patient moved the eye by muscles normally innervated by cranial nerve III (See Figures 4 and 5).

Discussion
Superior orbital fissure syndrome (SOFS) is a clinical diagnosis characterized by ophthalmoplegia, ptosis, proptosis, dilation of the pupil, and hypesthesia of the eyelid and forehead. Hirschfield first described this syndrome in 1858 in the context of trauma. In 1896, André Rochon-Duvignaud described the syndrome secondary to syphilis. The differential diagnosis includes trauma, neoplasm, hematoma in the orbital muscle cone, vascular malformations, inflammation, or infectious process involving the retrobulbar space.
The superior orbital fissure is bound medially by the lesser wing of the sphenoid, inferiorly and laterally by the greater wing of the sphenoid, and superiorly by the frontal bone. It is a conduit between the orbit and the middle cranial fossa. The superior and inferior branches of the oculomotor nerve, trochlear, abducens, and the three branches of the ophthalmic division of the trigeminal nerve—frontal, lacrimal, and nasocilliary—pass through this fissure. The fissure also contains the inferior and superior ophthalmic veins and well as sympathetic fibers from the cavernous plexus.
SOFS is distinguished from orbital apex syndrome (OAS) by the lack of optic nerve involvement. Similar to OAS, cavernous sinus syndrome (CSS) has the added involvement of V2 and oculosympathetic fibers and is commonly bilateral. Ophthalmoplegia is caused by damage to the cranial nerves III, IV and VI. Ptosis is caused by insult to either sympathetic fibers from the cavernous sinus, resulting in decreased tone of Muller's muscle, or to efferent somatic fibers of the superior branch of the oculomotor nerve, resulting in loss of tone to the levator palpebrae superioris muscle. Proptosis is a consequence of the lack of innervation to the globe retractors, causing forward movement of the globe. Pupillary dilation, fixation and loss of accommodation are secondary to parasympathetic fiber damage traveling with the inferior division of the oculomotor nerve. Finally, the eyelid and forehead anesthesia is a result of lacrimal and frontal nerve compromise.
Neuroimaging is critical to the workup of multiple cranial nerve palsies. In the setting of trauma, a CT scan of the brain and orbits is helpful to identify bony anatomy and to evaluate orbital apex fractures. To evaluate the orbital apex and cavernous sinus, an MRI of the brain and orbits with contrast and fat suppression is the preferred study. If a vascular malformation is suspected, an MRA or CT angiogram is a useful diagnostic tool.
The treatment of superior orbital fissure syndrome depends on the suspected process. In the case of traumatic SOFS, conservative management and close observation without surgical intervention is preferred. The use of oral steroids may be helpful in the short-term while considering surgical intervention. Surgery is reserved for the rare circumstance of bony fragments and/or hematoma impinging on the optic nerve. Although some case series recommend the use of corticosteroids, there are no formal studies that document benefit, and, therefore, steroids should be used cautiously. Consultation with internal medicine, otolaryngology or neurosurgery may be useful depending on the underlying etiology considered.
Dr. Fram is a third-year resident.




