Presentation
A 2-and-a-half year old girl presented to her pediatrician with right eyelid swelling and mild ecchymosis. Her parents were unsure of the exact cause of these symptoms, but believed that they appeared shortly after she had fallen and bumped her right upper lid.
The parents were reassured by the pediatrician, and no further workup was pursued at that time. Over the following two months, the parents noticed some improvement in the swelling, but the lump on her right upper lid persisted. It appeared to be waxing and waning in size. At this point, she was referred to a pediatric ophthalmologist.
Medical History
The patient was developmentally normal and in good general health with no significant past medical history. Family history was noncontributory. The family denied recent fevers, rashes or weight loss.
Examination
Visual acuity measured by an Allen picture chart was 20/80 in the right eye, 20/50 in the left eye. Her pupils were briskly reactive with no relative afferent pupillary defect.
Extraocular motility was full and there was no strabismus. Intraocular pressures were within normal limits.
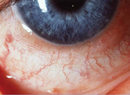
External examination was significant for edema and mild ecchymosis of the right upper eyelid. There was a palpable mass in the temporal aspect of this eyelid, which was noted to be firm, mobile and mildly tender (See Figure 1). No proptosis was observed. She had mild ptosis on the right side secondary to the mass effect from the upper eyelid. The remainder of the anterior segment and dilated fundoscopic examination was within normal limits.
Diagnosis, Workup and Treatment
The differential diagnosis of an otherwise healthy 2-and-a-half year old girl with an eyelid/orbital mass associated with edema and ecchymosis included: neoplastic processes such as Langerhans histiocytosis; fibrous dysplasia; neuroblastoma and rhabdomyosarcoma; a congenital lesion such as a dermoid cyst; vascular/lymphatic abnormalities such as capillary hemangioma orbital varices and lymphangioma; and an infectious etiology such as orbital cellulitis. Given the subacute nature and appearance of the lesion on clinical exam, neoplasia was highest on the differential diagnosis. The appearance of bony erosion on imaging raised suspicion for malignancy such as rhabdomyosarcoma or neuroblastoma metastasis, versus a more benign process such as Langerhans histiocytosis. The history of mild trauma reported by the parents was believed to be coincidental.
The patient was referred to the Oculoplastics service for a diagnostic biopsy of the lesion. Histopathology revealed Langerhans cells with nuclear folds, eosinophils and osteoclast-like giant cells (See Figure 3). Immunohistochemistry demonstrated characteristic positive immunoreactivity for CD1a, confirming a diagnosis of Langerhans histiocytosis.
The child was referred to an oncologist for testing and treatment. A skeletal survey revealed only the right orbital lesion with no other bone involvement, indicating single-site disease. Lab workup was also within normal limits, further supporting that the patient did not likely have other organ involvement. Since the orbital lesion was felt to be threatening the globe and optic nerve by local mass effect, treatment with corticosteroids and systemic chemotherapy was instituted in an attempt to decrease the size of the mass and improve the patient's vision.
Discussion
Langerhans histiocytosis is a collection of rare disorders resulting from the accumulation of proliferating dendritic histiocytes. Other names for this disease spectrum have included histiocytosis X, eosinophilic granuloma, Hand-Schuller-Christian syndrome and Letterer-Siwe Disease. Disease occurs most commonly in children between 5 and 10 years of age, with a higher male-to-female ratio.
The spectrum of disease varies in severity from solitary benign lesions to chronically disseminated fatal disease. Single-site presentations include skin, bone or lymph node involvement. The most common sites for lytic bony lesions are the skull, orbit, ribs and long bones. Multisystem disease can affect the lungs, liver, bone marrow, endocrine system, gastrointestinal system and central nervous system.
From an ophthalmic standpoint, Langerhans histiocytosis may present with a lytic defect affecting the superotemporal orbit or the sphenoid wing. Localized pain and tenderness are relatively common. Other symptoms can include proptosis, ptosis and periorbital swelling. Relapsing episodes of orbital inflammation may initially be misinterpreted as orbital cellulitis.
The diagnosis is confirmed by biopsy of suspicious lesions, which reveals proliferation of large histiocytic cells with folded nuclei along with interspersed eosinophils and multinucleated giant cells. The histiocytic cells show positive immunoreactivity for various markers, including CD1a.
Prognosis is better in children older than 2 years with single-system disease; these may spontaneously resolve without treatment. The survival rate is only 50 percent for children diagnosed before 2 years of age with multifocal involvement. Localized orbital disease may be treated with excisional biopsy, intralesional steroid injection and/or low-dose radiation. Excision alone may be curative and bony defects may reossify completely following remission. Systemic involvement necessitates the administration of cytotoxic agents and systemic corticosteroids.
The author thanks Robert Penne, MD, of the Oculoplastics Service, and Ralph C. Eagle, MD, of the Pathology Department, at Wills Eye Institute for their assistance with this manuscript.
1. Margo CE, Goldman DR. Langerhans cell histiocytosis. Surv Ophthalmol 2008;53:332-58.
2. Maccheron LJ, McNab AA, Elder J, et al. Ocular adnexal Langerhans cell histiocytosis clinical features and management. Orbit 2006;25:169-77.
3. Harris GJ. Langerhans cell histiocytosis of the orbit: A need for interdisciplinary dialogue. Am J Ophthalmol 2006;141:374-378.
4. Cheung N, Selva D, McNab AA. Orbital Langerhans cell histiocytosis in adults. Ophthalmology 2007;114:1569-73.