Oculoplastic surgeons in Oregon suggest reanimating the paretic eyelid by insertion of a gold weight in the orbit rather than in a pretarsal pocket. A review of 59 patient charts over a 10-year period reveals this method to be an excellent means of prevention of the unfortunate sequelae of exposure keratopathy, they say.
A single surgeon used a 2.2-g gold weight implant in each case, with no wrapping materials. The ages of the 59 patients ranged from 15 to 92 years. No patients in the study group were Asian. The surgeons defined successful treatment as elimination of exposure keratopathy as determined by slit-lamp biomicroscopy and preservation of the visual axis. They defined postop complications as migration, extrusion, inflammation, infection and/or poor cosmesis.
In this series of patients, the surgeons found that the septum, orbicularis muscle and skin combined provided an adequate barrier to extrusion of the gold weight. They note their technique of a standard weight placed intraorbitally makes preop weight selection and intraoperative implant-wrapping unnecessary. The intraorbital location reduces the potentially unsightly bulk effect over the tarsus.
None of their patients had inflammation or infection from the implant. Only two patients suffered complications (both with confounding factors including previous surgeries). One had shifting of the gold weight, which was repositioned; the other had extrusion of the gold weight that required removal.
The surgeons believe that their technique of placing the implant in an intraorbital space attached to the levator aponeurosis provides excellent results without complication in standard lagophthalmos cases.
(Ophthal Plast Reconstr Surg 2004;20(3):202-206)
Tower R, Dailey R
Drugs Up, Glaucoma Surgeries Down
Researchers supported by Allergan have determined that a decrease in the number of glaucoma surgeries among U.S. Medicare patients coincided with the introduction of improved topical pharmacotherapies for the management of the disease. They consider that the ability to determine a causal relationship between the two is limited but likely, since the number of glaucoma surgeries in this population decreased between 1994 and 1999, while the prevalence of glaucoma in this same population remained stable.
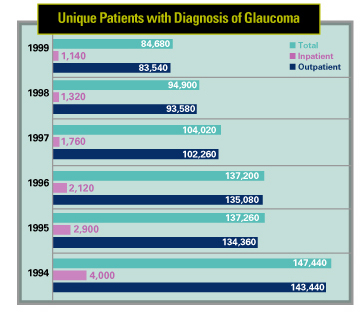 |
Numbers of surgeries were obtained from the Medicare 5% Standard Analytical File. The number of U.S. Medicare patients with a diagnosis of glaucoma during the study period remained constant at approximately 2.5 million. The number of inpatient and outpatient glaucoma surgeries among patients with a diagnosis of glaucoma decreased by nearly 43 percent from 1994 to 1996.
The decreasing trend in glaucoma surgeries over the study period, with the largest decline occurring from 1996 to 1997, was evident for both inpatient and outpatient surgeries and for all assessments including unique patients with a glaucoma diagnosis, unique patients with or without a glaucoma diagnosis, total discharges with a glaucoma diagnosis and total discharges with or without a glaucoma diagnosis.
(J Glaucoma 2004;13:221-226)
Strutton D, Walt J
Cataract Extraction OK Following Penetrating Keratoplasty
Investigators in Philadelphia consider cataract surgery following penetrating keratoplasty to be a safe and effective procedure. They acknowledge a low but definite risk of graft failure following cataract extraction, but add that most patients seem to benefit from improved visual activity and decreased spherical refractive error.
A mean of 8.4 years passed between penetrating keratoplasty and cataract surgery in this group. Following cataract extraction, corneal grafts remained clear in all but one eye, during an average follow-up period of 44.5 months. The patient who developed the graft failure had three episodes of preoperative endothelial rejection and a clear corneal graft at the time of cataract surgery.
Visual acuity improved in the remaining patients, with 15 of 28 having a postop best-corrected acuity of 20/30 or better. Absolute spherical refractive error decreased from a mean 6.6 ±3.4 D preop to 2.4 ±1.6 D postop. Cylindrical refractive error remained relatively stable at a mean 3.2 ±2.9 D preop to 2.8 ±2.4 D postop.
In patients with clear grafts and visually significant cataracts, investigators prefer cataract extraction alone over a repeat combined procedure.
(Cornea 2004;23:377-379)
Nagra P, Rapuano C, Laibson P, Kunimoto D, Kay M, Cohen E



