Mark B. Abelson, MD; David A. Sullivan; George W. Ousler III; Lisa Smith; and Ciera Maffei, North Andover, Mass.
In September, Taormina, Sicily, hosted the 5th International Conference of the Tear Film & Ocular Surface Society: Basic Science and Clinical Relevance. Spectacular beauty and old-world charm provided the perfect setting for this cutting-edge meeting of almost 500 basic scientists, clinicians and industry representatives specializing in the interdisciplinary study of tears and the ocular surface in their broadest and most distilled forms. To help you stay current on the latest research, we've culled the major papers and present them to you here. Read on for the highlights.
The conference, sponsored by the Tear Film & Ocular Surface Society, was inaugurated with a discussion of dry-eye epidemiology by Debra Schaumberg, OD, of Boston's Brigham and Women's Hospital. In the largest studies, the age-adjusted prevalence of dry eye in the United States was 3.2 million women and 1.68 million men, aged 50 years or older. Her research showed no differences between blacks and whites, but there may be a higher incidence in Hispanic and Asian populations. Use of estrogen replacement increased the risk of dry eye by about 70 percent if used alone and by 30 percent if used in combination with progesterone. Androgen deficiency also emerged as a risk factor, both in women and in men. Essential fatty acids also appeared critical to maintaining a healthy ocular surface. The relevance of dry-eye disease and its context as a worldwide public-health problem were brought into focus through this elegant commencement to the meeting.
Tear Film
The first session of TFOS focused on the tear film, specifically the properties and dynamic interactions of the mucin, aqueous and lipid layers. With research conducted at Schepens Eye Research Institute in Boston, Pablo Argüeso, PhD, presented findings on the regulatory role of the transmembrane O-glycosylated mucins, which form the outermost interface between epithelial cells and the external environment. In patients with dry eye, expression of enzymes that synthesize mucin O-glycans was altered, along with the distribution of O-glycosylated mucin, suggesting their role in maintaining a normal ocular surface. The role of mucin O-glycans in preventing apical cell surface adhesion and bacterial infection at the ocular surface was also discussed. Mediation of these enzymatic events could be a potential target in the treatment of tear-film dysfunction.
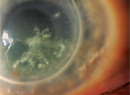
 |
| Researchers and clinicians took in the research and the beautiful Sicilian scenery at this year"s Tear Film & Ocular Surface Society meeting. |
Mucins are integral in maintaining the stability of the tear film, and expression of mucins is believed to be altered in dry-eye patients. Research from Schepens Eye Research Institute investigated this relationship as well. Sandra Spurr-Michaud, MS, and researchers from Alcon and the University of Waterloo, Ontario, highlighted increases in the H185 epitope of MUC16, a membrane-associated mucin in the conjunctival epithelium of patients with moderate dry eye, suggesting that a compensatory increase occurs in glycosylation of cell surface mucins or goblet cell mucins. Vinodh Kakkassery, MD, and co-workers presented data on membrane-associated mucins of an epithelial cell line, which demonstrated increased shedding rates of MUC1 and MUC 16 when exposed to the inflammatory mediators interleukin-6 and tumor necrosis factor-a. Increased shedding is thought to lead to dye penetration and bacterial adherence at the corneal surface.
From the other side of the world, Thomas Millar, PhD, of the University of Western Sydney, Australia, discussed the functional role of the tear film lipid layer. Advances in mass spectroscopy have revealed surprising results on the composition of the meibomian gland lipids: Sterol and wax esters form the bulk of the lipids, and high levels of cholesterol esters are more likely to lead to dry eye. Proteins found in the aqueous layer could serve as surfactants, and these, along with mucins, not only interact with lipids at the lipid-aqueous interface, but also form part of the surface layer and work to slow evaporation.
Contact lens wear is known to induce changes in the tear film and lead to dry-eye symptomatology; however, dry eye associated with contact lens wear may be pathologically different from typical dry eye. Differential tear film characteristics of dry-eye patients and dry-eye contact lens wearers were presented in posters by Cécile Maissa, PhD, and Michel Guillon, PhD, from OTG Research & Consultancy in London. The researchers found that the lipid layer was significantly thinner in dry-eye sufferers, yet the aqueous layer was unchanged. This thin lipid layer was also found in contact lens wearers with dry-eye symptomatology.
Sometimes, clinical observations are more easily understood and analyzed through mathematical models, which give researchers a higher level of control over the project they're engaged in. At the University of Oxford, Eamonn Gaffney, PhD, and colleagues developed a mathematical model of tear volume and osmolarity in relation to the mechanism of damage and clinical features of dry eye. In the normal eye, the tear film had a higher osmolarity than the meniscus, a differential that was increased in dry eye, particularly in the evaporative etiology. This may help to explain clinical features, including the centralized distribution of ocular damage and pain. Furthermore, for a given meniscus hyperosmolarity, the greater tear film osmolarity exposes the ocular surface to a greater risk of damage. Through collaboration of the University of Delaware and Ohio State University, mathematical models were also developed by Professor Richard Braun's team to quantify the dynamics of the tear film and tear-film evolution during the blink cycle.
Ocular Surface
The ocular surface dominated the discussions and presentations of the second session. Researchers delved into the search for novel methods of repair and regeneration of the corneal and conjunctival epithelia, immune regulation and response to infection, and the effect of aging on the ocular surface and tear film.
The potential of ocular stem cell therapy for repairing the damage caused by degenerative and sight-threatening ocular diseases, including retinal degeneration, was discussed in a keynote address by Julie Daniels, PhD, from the UCL Institute of Ophthalmology in London. Due to its transparency and accessibility, the cornea is an ideal system in which to study the regulatory mechanisms that modulate adult epithelial, mesenchymal and endothelial stem cell function. Dr. Daniels outlined the knowledge needed to optimize the clinical application of stem cell research, and emphasized the significance of the cornea in regenerative medicine. Future applications of stem cell research appear limitless: Saadettin Sel, MD, from Martin Luther University Halle-Wittenberg, and colleagues presented a poster that showed that topically applied bone marrow and CD117+ stem cells can successfully treat corneal ulcers.
Discussion of innate and adaptive immunity focused on the mediating role of toll-like receptors and associated mediators in ocular inflammatory diseases. TLR expression was studied in dry eye by a group led by Rachel Redfern, OD, at the University of Houston, who evaluated TLR4, -5 and -9 mRNA expression after simulating dry-eye culture conditions. Cytokines didn't significantly modulate the expression of TLR4, -5 and -9 in the cells tested, but TLR4 and -5 expression was significantly upregulated and TLR9 downregulated in response to hyperosmolar stress in certain cell lines, indicating that TLR4 and 5 might stimulate ocular surface inflammation in severe dry eye.
Ling Huang, representing the University of Houston, gave a keynote address on the role of the antimicrobial peptides defensins and cathelicidin at the ocular surface. Human ocular surface epithelia express three beta-defensins (hBD) and the cathelicidin LL37, some of which are constitutively expressed (hBD-1 and -3), while others are upregulated (hBD-3 and LL37) in response to inflammation and infection. These latter peptides have potent antibacterial activity and have clear clinical potential. Given the clinical potential of antimicrobial peptides, further testing in vitro must be performed to identify the peptides with most potential in vivo. Delivery techniques must also be investigated, since simple topical application could prove toxic.
Prevention of ocular infections is a constant goal, but immunization is not always the easiest or most effective method of doing so. Gerald Pier, PhD, of Brigham and Women's Hospital, discussed the difficulties of developing vaccines for serious ocular pathogens, particularly in proving their efficacy in clinical trials. He suggested that a more rational approach might be to identify specific interventions once a pathogen has been tentatively identified, and then augment standard therapy to create better outcomes of such infections. One example involves passive therapy with IgG antibodies to either the cell surface liposaccharide or alginate capsular polysaccharide for both prophylactic and therapeutic efficacy against P. aeruginosa ulcerative keratitis. Immunological interventions for serious eye disease would likely involve these kinds of passive therapy and/or inhibitors of essential virulence factors or processes that can be used at diagnosis and in conjunction with standard therapies for microbial keratitis.
Tear Film and Surface Interactions
The final section of the conference explored the interactions between the tear film and ocular surface. Presentations pertained to developing and improving diagnostics and clinical models pertinent to dry eye. Researchers emphasized the symbiosis necessary between understanding, diagnosing and treating dry eye. They presented papers and posters in the following areas:
• Diagnostics. Since many clinical dry-eye studies involve the subjective evaluation of pain and irritation, advancement in the measurement of these parameters would greatly aid in the evaluation of new therapeutic modalities. In her presentation, Linda Bartoshuk, PhD, of the University of Florida, discussed the validity and interpretation of subjective grading scales of pain, presenting magnitude-matching studies evaluating unrelated sensory intensities (pain and light). These experiments identified that women's "most intense pain" was 27 percent greater than men's, demonstrating the innate error from visual analogue scale (VAS) readings. The inclusion of multiple potential standards, such as remembered sensations, was suggested as a method to obtain more accurate pain measurement across subjects. A simple modification to the "global VAS" was also presented, which can be used a linear or numerical (0 to 100) scale ranging from "no sensation" to "most intense sensation of any kind." Nevertheless, the validity of these measurements relies on the assumption that the highest score given by all subjects would reflect a reasonably similar intensity in pain. Carlos Belmonte, MD, PhD, from Universidad Miguel Hernandez-CSIC in San Juan de Alicante, Spain, then presented the neural basis of sensation in intact and injured corneas.
An interesting poster presentation within the diagnostics section illustrated a new mathematically defined system for grading ocular surface staining. Representatives in a collaborative effort by the University of Oxford, the University of Louisville and the National Eye Institute, presented a standard recording template and set of panels that provided a grading range of 0 to 10 for each zone of staining assessed, with a total scale range of 0 to 110. This approach could add to the battery of tests striving for improved objectivity in the evaluation of dry eye and the quantification of change.
From a basic science perspective, in vivo confocal microscopy was used to assess inflammatory changes in ocular surface disease by Christophe Baudouin, MD, PhD, and colleagues from France's Quinze-Vingts National Ophthalmology Hospital and Immunotoxicology Center. Using the Rostock Cornea Model of the Heidelberg Retina Tomograph, the researchers evaluated the ocular epithelia in 20 patients with corneal inflammation and/or neovascularization. This technique allowed for the visualization of inflammatory cell processes (i.e., cell rolling, live diapedesis, chromatin fragmentation and quantification of dendritic cell infiltration) which were all correlated with cytological patterns.
• Clinical models. Pamela Walker, PhD, and colleagues at our office (ORA Clinical Research and Development) presented data on diurnal variation in visual function and keratitis in patients with dry eye. Results showed that dry-eye patients were indeed worse in the evening, with impaired visual function and prolonged reading rates, increased corneal keratitis and conjunctival redness. The findings highlight the role of time-of-day in dry-eye patients' signs, symptoms and visual function abilities.
Tear hyperosmolarity returned as the precipitating factor of ocular surface damage in a lecture by Anthony Bron, MD, on findings from researchers at the University of Oxford. He discussed the variables that affect osmolarity: varying distribution of osmolarity at the ocular surface (i.e., between tear film and meniscus); regional differences in airflow; temperature and variations in ambient temperature and humidity; imperfect tear mixing, etc. He hypothesized that interactions among all factors determine the phenotype, frequency and severity of dry eye in a population. He also discussed the relevance of LASIK-induced dry eye and how it differs in etiology from both aqueous-deficient and evaporative dry eye.
• Therapies. In terms of pharmacological agents, several posters presented results of newer generation therapies and others presented data on more classic therapies for dry eye, such as the efficacy found using punctal plugs in post-LASIK dry-eye patients in a study by Ikuko Toda, MD, of the Minamiaoyama Eye Clinic in Tokyo.
From Glasgow Caledonian University in Scotland, Alan Tomlinson, PhD, then discussed objective tests in the differential diagnosis of dry eye. Values of 12 percent per minute for tear turnover, 33 g/cm2/hour for evaporation and 317 mOsm/liter for osmolarity were found to give the optimal sensitivity, specificity and accuracy when used together in a weighted comparison, rather than any test singly.
The keynote address, given by this article's lead author, Dr. Abelson of Schepens Eye Research Institute and ORA Clinical Research and Development, explored the dry-eye pipeline. He discussed the difficulties in matching patient criteria to clinically relevant diagnostics and endpoints in order to significantly quantify change during clinical trial design. Dr. Abelson presented a thorough review of therapeutic agents in the pipeline, with special emphasis on products such as an emerging formulation of doxycycline (Alacrity Biosciences, Laguna Hills, Calif.) and diquafosol tetrasodium (Inspire Pharmaceuticals, Durham, N.C.). Dr. Abelson further explained clinical tools to evaluate novel agents including the Ocular Protection Index (OPI), which provides a binomial measure of ocular surface protection, and a new diagnostic test of the inter-blink interval visual acuity decay (IVAD), which measures changes in visual function. Successful clinical models of dry eye were presented as well, with a focus on the controlled adverse environment (CAE) and its relevance in evaluating new therapeutic agents.
It would be difficult to say which aspect of ocular surface and tear film research benefited most from the exchange of ideas that took place at this year's TFOS meeting. It's clear, however, that the collaboration between basic science, clinical science and industry at the conference presented a tremendous opportunity for advances in dry-eye research and therapies.
Mark B. Abelson, MD, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. David A. Sullivan, PhD, is a senior scientist at the Schepens Eye Research Institute, an associate professor at Harvard Medical School, and the president of the Tear Film & Ocular Surface Society. George Ousler is the director of the dry eye department at Ophthalmic Research Associates in North Andover. Lisa Smith is a consultant and Ciera Maffei is a medical writer for Ophthalmic Research Associates.